Celsentri, INN-Maraviroc
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effects of Enzyme Inducers Efavirenz and Tipranavir/Ritonavir on the Pharmacokinetics of the HIV Integrase Inhibitor Dolutegravir
Eur J Clin Pharmacol (2014) 70:1173–1179 DOI 10.1007/s00228-014-1732-8 CLINICAL TRIAL Effects of enzyme inducers efavirenz and tipranavir/ritonavir on the pharmacokinetics of the HIV integrase inhibitor dolutegravir Ivy Song & Julie Borland & Shuguang Chen & Phyllis Guta & Yu Lou & David Wilfret & Toshihiro Wajima & Paul Savina & Amanda Peppercorn & Stephen Castellino & David Wagner & Louise Hosking & Michael Mosteller & Justin P.Rubio & Stephen C. Piscitelli Received: 7 May 2014 /Accepted: 11 August 2014 /Published online: 23 August 2014 # The Author(s) 2014. This article is published with open access at Springerlink.com Abstract study due to increases in alanine aminotransferase that were Purpose Dolutegravir (DTG) is an unboosted, integrase in- considered related to TPV/r. Co-administration with EFV hibitor for the treatment of HIV infection. Two studies evalu- resulted in decreases of 57, 39 and 75 % in DTG AUC(0–τ), ated the effects of efavirenz (EFV) and tipranavir/ritonavir Cmax and Cτ, respectively. Co-administration with TPV/r re- (TPV/r) on DTG pharmacokinetics (PK) in healthy subjects. sulted in decreases of 59, 46 and 76 % in DTG AUC(0–τ), Cmax Methods The first study was an open-label crossover where and Cτ, respectively. 12 subjects received DTG 50 mg every 24 hours (q24h) for Conclusions Given the reductions in exposure and PK/ 5 days, followed by DTG 50 mg and EFV 600 mg q24h for pharmacodynamic relationships in phase II/III trials, DTG 14 days. The second study was an open-label crossover where should be given at an increased dose of 50 mg twice daily 18 subjects received DTG 50 mg q24h for 5 days followed by when co-administered with EFV or TPV/r, and alternative TPV/r 500/200 mg every 12 hours (q12h) for 7 days and then regimens without inducers should be considered in integrase DTG 50 mg q24h and TPV/r 500/200 mg q12h for a further inhibitor-resistant patients. -

Treatment-Drugs
© National HIV Curriculum PDF created September 23, 2021, 9:14 am Stavudine (Zerit) Table of Contents Stavudine Zerit Summary Drug Summary Key Clinical Trials Resistance Key Drug Interactions Drug Summary Stavudine, an early nucleoside reverse transcriptase inhibitor (NRTI), was used as part of combination antiretroviral therapy for years, but now has become obsolete and replaced by better-tolerated and safer options. Stavudine poses risk of serious toxicity, including peripheral neuropathy (which can be permanent), pancreatitis, lipoatrophy, and lactic acidosis. Fatal and nonfatal cases of pancreatitis and lactic acidosis have been reported, especially when stavudine was combined with didanosine. According to the Adult and Adolescent ARV Guidelines, stavudine is no longer recommended for the treatment of HIV infection due to potential severe toxicity. Further, all persons currently taking stavudine should be strongly encouraged to switch to a safer medication. The sale and distribution of all strengths of stavudine will be discontinued and removed from the market in the United States in 2020. Key Clinical Trials Stavudine was studied for treatment-naïve patients as part of triple therapy, such as with lamivudine plus indinavir [START I], lamivudine plus lopinavir-ritonavir [M98-863], and lamivudine plus efavirenz [DART II]. Several studies demonstrated benefits of switching stavudine to newer NRTI agents, such as tenofovir disoproxil fumarate; the switch led to decreased rates of metabolic complications and mitochondrial toxicity [903E, SNAP, and ACTG 5142]. Resistance For a listing of the most common clinically significant mutations associated with stavudine (d4T) resistance, see the NRTI Resistance Notes on the Stanford University HIV Drug Resistance Database. Page 1/2 Key Drug Interactions For complete information on stavudine-related drug interactions, see the Drug Interactions section in the Stavudine (Zerit) Prescribing Information. -

Eparate Formulations According to the Prescribed Dosing Recommendations for These Products
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Lamivudine/Zidovudine Teva 150 mg/300 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 150 mg lamivudine and 300 mg zidovudine. For the full list of excipients see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet White, capsule shaped, biconvex, film-coated scored tablet – engraved with “L/Z” on one side and “150/300” on the other side. The tablet can be divided into equal halves. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Lamivudine/Zidovudine Teva is indicated in antiretroviral combination therapy for the treatment of Human Immunodeficiency Virus (HIV) infection (see section 4.2). 4.2 Posology and method of administration Therapy should be initiated by a physician experienced in the management of HIV infection. Lamivudine/Zidovudine Teva may be administered with or without food. To ensure administration of the entire dose, the tablet(s) should ideally be swallowed without crushing. For patients who are unable to swallow tablets, tablets may be crushed and added to a small amount of semi-solid food or liquid, all of which should be consumed immediately (see section 5.2). Adults and adolescents weighing at least 30 kg: the recommended oral dose of Lamivudine/Zidovudine Teva is one tablet twice daily. Children weighing between 21 kg and 30 kg: the recommended oral dose of Lamivudine/Zidovudine Teva is one-half tablet taken in the morning and one whole tablet taken in the evening. Children weighing from 14 kg to 21 kg: the recommended oral dose of Lamivudine/Zidovudine Teva is one-half tablet taken twice daily. -
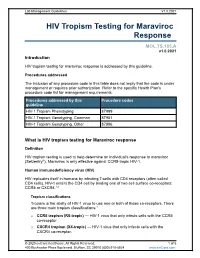
HIV Tropism Testing for Maraviroc Response
Lab Management Guidelines V1.0.2021 HIV Tropism Testing for Maraviroc Response MOL.TS.185.A v1.0.2021 Introduction HIV tropism testing for maraviroc response is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline HIV-1 Tropism Phenotyping 87999 HIV-1 Tropism Genotyping, Common 87901 HIV-1 Tropism Genotyping, Other 87906 What is HIV tropism testing for Maraviroc response Definition HIV tropism testing is used to help determine an individual's response to maraviroc (Selzentry®). Maraviroc is only effective against CCR5-tropic HIV-1. Human immunodeficiency virus (HIV) HIV replicates itself in humans by infecting T-cells with CD4 receptors (often called CD4 cells). HIV-1 enters the CD4 cell by binding one of two cell surface co-receptors: CCR5 or CXCR4.1,2 Tropism classifications Tropism is the ability of HIV-1 virus to use one or both of these co-receptors. There are three main tropism classifications:3 o CCR5 tropism (R5-tropic) — HIV-1 virus that only infects cells with the CCR5 co-receptor. o CXCR4 tropism (X4-tropic) — HIV-1 virus that only infects cells with the CXCR4 co-receptor. © 2020 eviCore healthcare. All Rights Reserved. 1 of 5 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 o Dual or mixed tropism (D/M-tropic) — HIV-1 virus populations that can use either co-receptor to infect cells. -

Revised 4/1/2021 GEORGIA MEDICAID FEE-FOR-SERVICE HIV
GEORGIA MEDICAID FEE-FOR-SERVICE HIV-AIDS PA SUMMARY Preferred (may not be all inclusive) Non-Preferred Abacavir generic Abacavir/lamivudine/zidovudine generic Abacavir/lamivudine generic Aptivus (tipranavir) Complera (emtricitabine/rilpivirine/tenofovir disoproxil Atazanavir capsules generic fumarate) Atripla (efavirenz/emtricitabine/tenofovir disoproxil Crixivan (indinavir) fumarate) Biktarvy (bictegravir/emtricitabine/tenofovir Delstrigo (doravirine/lamivudine/tenofovir disoproxil alafenamide) fumarate) Cimduo (lamivudine/tenofovir disoproxil fumarate) Fuzeon (enfuvirtide) Descovy (emtricitabine/tenofovir alafenamide) Intelence (etravirine) Dovato Invirase (saquinavir) Edurant (rilpivirine)* Lexiva (fosamprenavir) Efavirenz tablets generic Nevirapine extended-release generic Emtriva (emtricitabine) Norvir Powder (ritonavir) Epivir solution (lamivudine) Pifeltro (doravirine) Evotaz (atazanavir/cobicistat)* Reyataz Powder (atazanavir) Genvoya (elvitegravir/cobicistat/emtricitabine/ Ritonavir tablets generic tenofovir alafenamide) Isentress and Isentress HD (raltegravir)* Rukobia (fostemsavir) Juluca (dolutegravir/rilpivirine) Selzentry (maraviroc) Kaletra (lopinavir/ritonavir) Stavudine generic^ Stribild (elvitegravir/cobicistat/emtricitabine/ tenofovir Lamivudine generic disoproxil fumarate) Symfi (efavirenz 600 mg/lamivudine/tenofovir Lamivudine/zidovudine generic disoproxil fumarate) Symfi Lo (efavirenz 400 mg/lamivudine/tenofovir Nevirapine immediate-release tablets generic disoproxil fumarate) Norvir (ritonavir) Temixys (lamivudine/tenofovir -

Truvada (Emtricitabine / Tenofovir Disoproxil)
Pre-exposure Prophylaxis (2.3) HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use Recommended dose in HIV-1 uninfected adults: One tablet TRUVADA safely and effectively. See full prescribing information (containing 200 mg/300 mg of emtricitabine and tenofovir for TRUVADA. disoproxil fumarate) once daily taken orally with or without food. (2.3) TRUVADA® (emtricitabine/tenofovir disoproxil fumarate) tablets, for oral use Recommended dose in renally impaired HIV-uninfected Initial U.S. Approval: 2004 individuals: Do not use TRUVADA in HIV-uninfected individuals if CrCl is below 60 mL/min. If a decrease in CrCl is observed in WARNING: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH uninfected individuals while using TRUVADA for PrEP, evaluate STEATOSIS, POST-TREATMENT ACUTE EXACERBATION OF potential causes and re-assess potential risks and benefits of HEPATITIS B, and RISK OF DRUG RESISTANCE WITH USE OF continued use. (2.4) TRUVADA FOR PrEP IN UNDIAGNOSED HIV-1 INFECTION -----------------------DOSAGE FORMS AND STRENGTHS------------------- See full prescribing information for complete boxed warning. Tablets: 200 mg/300 mg, 167 mg/250 mg, 133 mg/200 mg, and 100 Lactic acidosis and severe hepatomegaly with steatosis, mg/150 mg of emtricitabine and tenofovir disoproxil fumarate . (3) including fatal cases, have been reported with the use of nucleoside analogs, including VIREAD, a component of TRUVADA. (5.1) --------------------------------CONTRAINDICATIONS----------------------------- TRUVADA is not approved for the treatment of chronic Do not use TRUVADA for pre-exposure prophylaxis in individuals with hepatitis B virus (HBV) infection. Severe acute unknown or positive HIV-1 status. TRUVADA should be used in exacerbations of hepatitis B have been reported in patients HIV-infected patients only in combination with other antiretroviral coinfected with HIV-1 and HBV who have discontinued agents. -

Page: Treatment-Drugs
© National HIV Curriculum PDF created September 29, 2021, 5:12 am Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine (Symtuza) Table of Contents Darunavir-Cobicistat-Tenofovir alafenamide-Emtricitabine Symtuza Summary Drug Summary Key Clinical Trials Key Drug Interactions Drug Summary The fixed-dose combination tablet darunavir-cobicistat-tenofovir alafenamide-emtricitabine is a single-tablet regimen that can be considered for treatment-naïve or certain treatment-experienced adults living with HIV. This single-tablet regimen offers a one pill daily regimen with high barrier to resistance (due to the darunavir- cobicistat), with potentially less renal and bone toxicity as compared to regimens that include tenofovir DF; however, it has potential gastrointestinal adverse effects and drug-drug interactions, primarily due to the cobicistat component. In clinical trials, darunavir-cobicistat-tenofovir alafenamide-emtricitabine was compared to darunavir-cobicistat plus tenofovir DF-emtricitabine as initial therapy for treatment-naïve individuals and found to be equally effective in terms of viral suppression. A switch to the fixed-dose combination tablet was also compared to continuing a boosted protease inhibitor plus tenofovir DF- emtricitabine and again determined to have equivalent efficacy. The FDA has approved darunavir-cobicistat- tenofovir alafenamide-emtricitabine as a complete regimen for treatment-naïve individuals or treatment- experienced individuals who have a suppressed HIV RNA level on a stable regimen for at least 6 months and no resistance to darunavir or tenofovir. Key Clinical Trials A phase 3 trial in treatment-naïve individuals compared the fixed-dose single-tablet regimen darunavir- cobicistat-tenofovir alafenamide-emtricitabine with the regimen darunavir-cobicistat plus tenofovir DF- emtricitabine emtricitabine [AMBER]. -

Download Article PDF/Slides
New Antiretrovirals in Development: Reprinted from The PRN Notebook,™ june 2002. Dr. James F. Braun, Editor-in-Chief. Tim Horn, Executive Editor. Published in New York City by the Physicians’ Research Network, Inc.,® John Graham Brown, Executive Director. For further information and other articles The View in 2002 available online, visit http://www.PRN.org All rights reserved. © june 2002. Roy “Trip” Gulick, md, mph Associate Professor of Medicine, Weill Medical College of Cornell University Director, Cornell Clinical Trials Unit, New York, New York Summary by Tim Horn Edited by Scott Hammer, md espite the fact that 16 antiretro- tiviral activity of emtricitabine was estab- Preliminary results from two random- virals are approved for use in the lished, with total daily doses of 200 mg or ized studies—FTC-302 and FTC-303—were United States, there is an indis- more producing the greatest median viral reported by Dr. Charles van der Horst and putable need for new anti-hiv com- load suppression: 1.72-1.92 log. Based on his colleagues at the 8th croi, held in Feb- pounds that have potent and these data, a once-daily dose of 200 mg ruary 2001 in Chicago (van der Horst, durable efficacy profiles, unique re- was selected for further long-term clinical 2001). FTC-302 was a blinded comparison sistance patterns, patient-friendly dosing study. “This is what we’re looking forward of emtricitabine and lamivudine, both in schedules, and minimal toxicities. To pro- to with emtricitabine,” commented Dr. combination with stavudine (Zerit) and vide prn with a glimpse of drugs current- Gulick. -

Review CCR5 Antagonists: Host-Targeted Antivirals for the Treatment of HIV Infection
Antiviral Chemistry & Chemotherapy 16:339–354 Review CCR5 antagonists: host-targeted antivirals for the treatment of HIV infection Mike Westby* and Elna van der Ryst Pfizer Global R&D, Kent, UK *Corresponding author: Tel: +44 1304 649876; Fax: +44 1304 651819; E-mail: [email protected] The human chemokine receptors, CCR5 and suggest that these compounds have a long plasma CXCR4, are potential host targets for exogenous, half-life and/or prolonged CCR5 occupancy, which small-molecule antagonists for the inhibition of may explain the delay in viral rebound observed HIV-1 infection. HIV-1 strains can be categorised by following compound withdrawal in short-term co-receptor tropism – their ability to utilise CCR5 monotherapy studies. A switch from CCR5 to (CCR5-tropic), CXCR4 (CXCR4-tropic) or both (dual- CXCR4 tropism occurs spontaneously in approxi- tropic) as a co-receptor for entry into susceptible mately 50% of HIV-infected patients and has been cells. CCR5 may be the more suitable co-receptor associated with, but is not required for, disease target for small-molecule antagonists because a progression. The possibility of a co-receptor natural deletion in the CCR5 gene preventing its tropism switch occurring under selection pressure expression on the cell surface is not associated by CCR5 antagonists is discussed. The completion with any obvious phenotype, but can confer of ongoing Phase IIb/III studies of maraviroc, resistance to infection by CCR5-tropic strains – the aplaviroc and vicriviroc will provide further insight most frequently sexually-transmitted strains. into co-receptor tropism, HIV pathogenesis and The current leading CCR5 antagonists in clinical the suitability of CCR5 antagonists as a potent development include maraviroc (UK-427,857, new class of antivirals for the treatment of HIV Pfizer), aplaviroc (873140, GlaxoSmithKline) and infection. -

Product Monograph for CELSENTRI
PRODUCT MONOGRAPH PrCELSENTRI maraviroc Tablets 150 and 300 mg CCR5 antagonist ViiV Healthcare ULC 245, boulevard Armand-Frappier Laval, Quebec H7V 4A7 Date of Revision: July 05, 2019 Submission Control No: 226222 © 2019 ViiV Healthcare group of companies or its licensor. Trademarks are owned by or licensed to the ViiV Healthcare group of companies. Page 1 of 60 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION.........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS..................................................................................4 ADVERSE REACTIONS....................................................................................................9 DRUG INTERACTIONS ..................................................................................................19 DOSAGE AND ADMINISTRATION..............................................................................28 OVERDOSAGE ................................................................................................................31 ACTION AND CLINICAL PHARMACOLOGY ............................................................31 STORAGE AND STABILITY..........................................................................................36 -

Epzicom and Ziagen Safety Review
Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology Pediatric Postmarketing Pharmacovigilance Date: July 11, 2018 Safety Evaluator: Margee P. Webster, Pharm.D., BCPS Division of Pharmacovigilance – I (DPV-I) Medical Officer: Ivone Kim, MD, FAAP DPV-I Team Leader: Kelly Cao, Pharm.D. DPV-II Deputy Division Director: Ida-Lina, Pharm.D., MS DPV-II Product Name: Abacavir (Ziagen®) and Abacavir/Lamivudine (Epzicom®) Pediatric Labeling Approval Date: Ziagen: March 23, 2015/Epzicom: September 17, 2015 Application Type/Number: NDA 020977 (Ziagen)/ NDA 021652 (Epzicom) Applicant/Sponsor: ViiV HealthCare/GlaxoSmithKline OSE RCM #: 2018-589 1 Reference ID: 4289856 TABLE OF CONTENTS Executive Summary........................................................................................................................ 1 1 Introduction............................................................................................................................. 1 1.1 Pediatric Regulatory History............................................................................................ 1 1.2 Relevant Labeled Safety Information .............................................................................. 1 1.2.1 Ziagen product labeling ........................................................................................... 1 1.2.2 Epzicom product labeling ....................................................................................... -

Annex I Summary of Product Characteristics
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT VIRACEPT 250 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION VIRACEPT 250 mg film-coated tablets contain 292.25 mg of nelfinavir mesylate corresponding to 250 mg of nelfinavir (as free base). For excipients, see 6.1. 3. PHARMACEUTICAL FORM Film-coated tablets 4. CLINICAL PARTICULARS 4.1 Therapeutic indications VIRACEPT is indicated in antiretroviral combination treatment of human immunodeficiency virus (HIV-1) infected adults, adolescents and children of 3 years of age and older. In protease inhibitor experienced patients the choice of nelfinavir should be based on individual viral resistance testing and treatment history. Refer to Section 5.1 Pharmacodynamic properties. 4.2 Posology and method of administration VIRACEPT film-coated tablets are administered orally and should be ingested with food. Patients older than 13 years: the recommended dosage of VIRACEPT film-coated tablets is 1250 mg (five 250 mg tablets) twice a day (BID) or 750 mg (three 250 mg tablets) three times a day (TID) by mouth. The efficacy of the BID regimen has been evaluated versus the TID regimen primarily in patients naïve to protease inhibitors (see section 5.1, pharmacodynamic properties). Patients aged 3 to 13 years: for children, the recommended starting dose is 25 – 30 mg/kg body weight per dose given TID. For children unable to take tablets, VIRACEPT oral powder may be administered (see Summary of Product Characteristics for VIRACEPT oral powder). The recommended dose of VIRACEPT film-coated tablets to be administered TID to children aged 3 to 13 years is as follows: Body Weight Number of Viracept 250mg kg film-coated tablets* 18 to < 23 2 ≥ 23 3 * see Summary of Product Characteristics for VIRACEPT oral powder for patients with less than 18 kg body weight.