Antibiotics: 21St Century Time Bomb
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vaughn Next Century Learning Center
2020 VAUGHN 2021 NEXT CENTURY LEARNING CENTER July/julio 2020 JULY-JULIO January/enero 2021 S M T W Th F S 1-31 Summer Vacation S M T W Th F S 1 2 3 4 30-31 Staff Development 1 2 5 6 7 8 9 10 11 3 SPED SPED SPED ESY ESY 9 12 13 14 15 16 17 18 AUGUST-AGOSTO 10 ESY ESY ESY ESY ESY 16 19 20 21 22 23 24 25 1 Compact Signing 17 18 ESY ESY ESY ESY 23 26 27 28 29 SD SD 3 Staff Development 24 ESY ESY ESY ESY SPED 30 0 4 FIRST DAY OF SCHOOL 31 August/agosto 2020 0 S M T W Th F S SEPTEMBER-SEPTIEMBRE February/febrero 2021 CS 4 Minimum Day (Comp Time) S M T W Th F S 2 SD 4 5 6 7 8 7 Labor Day Holiday SD 2 3 4 5 6 9 10 11 12 13 14 15 7 8 9 10 11 12 13 16 17 18 19 20 21 22 OCTOBER-OCTUBRE 14 15 16 17 18 19 20 23 24 25 26 27 28 29 5-9 Fall Break 21 22 23 24 25 26 27 30 31 28 20 NOVEMBER-NOVIEMBRE 18 September/septiembre 2020 3 Election Day - No Committee Meeting March/marzo 2021 S M T W Th F S 11 Veteran's Day Holiday S M T W Th F S 1 2 3 4 5 25 Minimum Day (Comp Time) 1 2 3 4 5 6 6 7 8 9 10 11 12 26-27 Thanksgiving Day Holiday 7 8 9 10 11 12 13 13 14 15 16 17 18 19 14 15 16 17 18 19 20 20 21 22 23 24 25 26 DECEMBER-DICIEMBRE 21 22 23 24 25 26 27 27 28 29 30 17 Minimum Day 28 29 30 31 21 18-31 Winter Vacation 20 October/octubre 2020 April/abril 2021 S M T W Th F S JANUARY-ENERO S M T W Th F S 1 2 3 1-6 Winter Vacation 1 2 3 4 5 6 7 8 9 10 4-6, 29 SpEd ESY (ID'd SPED Only) 4 5 6 7 8 9 10 11 12 13 14 15 16 17 7-28 ESY 11 12 13 14 15 16 17 18 19 20 21 22 23 24 18 Martin Luther King Jr Holiday 18 19 20 21 22 23 24 25 26 27 28 29 30 31 29 No School (Except -

Package 'Lubridate'
Package ‘lubridate’ February 26, 2021 Type Package Title Make Dealing with Dates a Little Easier Version 1.7.10 Maintainer Vitalie Spinu <[email protected]> Description Functions to work with date-times and time-spans: fast and user friendly parsing of date-time data, extraction and updating of components of a date-time (years, months, days, hours, minutes, and seconds), algebraic manipulation on date-time and time-span objects. The 'lubridate' package has a consistent and memorable syntax that makes working with dates easy and fun. Parts of the 'CCTZ' source code, released under the Apache 2.0 License, are included in this package. See <https://github.com/google/cctz> for more details. License GPL (>= 2) URL https://lubridate.tidyverse.org, https://github.com/tidyverse/lubridate BugReports https://github.com/tidyverse/lubridate/issues Depends methods, R (>= 3.2) Imports generics, Rcpp (>= 0.12.13) Suggests covr, knitr, testthat (>= 2.1.0), vctrs (>= 0.3.0), rmarkdown Enhances chron, timeDate, tis, zoo LinkingTo Rcpp VignetteBuilder knitr Encoding UTF-8 LazyData true RoxygenNote 7.1.1 SystemRequirements A system with zoneinfo data (e.g. /usr/share/zoneinfo) as well as a recent-enough C++11 compiler (such as g++-4.8 or later). On Windows the zoneinfo included with R is used. 1 2 R topics documented: Collate 'Dates.r' 'POSIXt.r' 'RcppExports.R' 'util.r' 'parse.r' 'timespans.r' 'intervals.r' 'difftimes.r' 'durations.r' 'periods.r' 'accessors-date.R' 'accessors-day.r' 'accessors-dst.r' 'accessors-hour.r' 'accessors-minute.r' 'accessors-month.r' -

International Standard Iso 8601-1:2019(E)
This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80010314 INTERNATIONAL ISO STANDARD 8601-1 First edition 2019-02 Date and time — Representations for information interchange — Part 1: Basic rules Date et heure — Représentations pour l'échange d'information — Partie 1: Règles de base Reference number ISO 8601-1:2019(E) © ISO 2019 This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80010314 ISO 8601-1:2019(E) COPYRIGHT PROTECTED DOCUMENT © ISO 2019 All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address belowCP 401or ISO’s • Ch. member de Blandonnet body in 8 the country of the requester. ISO copyright office Phone: +41 22 749 01 11 CH-1214 Vernier, Geneva Fax:Website: +41 22www.iso.org 749 09 47 PublishedEmail: [email protected] Switzerland ii © ISO 2019 – All rights reserved This preview is downloaded from www.sis.se. Buy the entire standard via https://www.sis.se/std-80010314 ISO 8601-1:2019(E) Contents Page Foreword ..........................................................................................................................................................................................................................................v -

GY 111 Lecture Notes Geological Time
GY 111 Lecture Notes D. Haywick (2008-09) 1 GY 111 Lecture Notes Geological Time Lecture Goals: A) How long is long? B) Geological time divisions C) Geological time scale Reference: Press et al., 2004, Chapters 1 and 10; Grotzinger et al., 2007, Chapters 1 and 8 (p 183-184) A) How Long is long? Geological time is unlike normal time, at least the time that you and I am familiar with. We are talking Time (with a capital T) and it is long. Most people cannot fathom the ages that geologists must deal with. To you, a long time may be 25 years (the age your car must reach to be get those trending antique license plates), or 100 years (the age your dining room table must be in order to claim it as an antique). Some people consider my lectures to be too long (50 minutes). But geologists deal with billions of years. The late Great Carl Sagan used to talk about billions and billions of stars; geologists talk about billions of years. The Earth is regarded by geologists as being some 4.6 billion years old. The oldest rocks that we have found on the Earth are about 4.1 billion years. The first organic materials (bacteria) appeared some 3.685 billion years ago. These are just numbers, but boy are they big numbers. There are several ways that you can illustrate how big these numbers are. You may have seen me do this in the lecture by using a tape measure. Another good way is by using money. -

The New Heavens and the New Earth: the Real Rapture
The New Heavens and the New Earth: The Real Rapture Since all these things are thus to be dissolved, what sort of persons ought you to be in lives of holiness and godliness, waiting for and hastening the coming of the day of God, because of which the Heavens will be kindled and dissolved, and the elements will melt with fire! But according to his promise we wait for new Heavens and a new earth in which righteousness dwells. ~ 2 Peter 3:11-13 OR SOME CHRISTIANS IN TODAY’S CULTURE, last few centuries and becoming widely believed only the single most important question has to do in the 19th century in English-speaking Protestant F with the “end times,” when the world will communions. Popular novels of the 20th century and experience great tribulations, according to in our modern day have spread this belief even fur- our Lord’s proph- ther. What does ecy (see Mt 24:3- “We hear the promise of a new creation, the Church teach 44). Many of on the subject? these Christians where God will be always with us, and we are caught up not will be able to drink unceasingly of the The New only in specula- Heavens and the tion about the end water of life, the Holy Spirit.” New Earth times — when it The Church will come, whether teaches us that it has started, what “God is preparing evils of contempo- a new dwelling rary culture match and a new earth in the Scriptural which righteous- prophecies — but ness dwells, in also what will hap- which happiness pen to them per- will fill and sur- sonally. -

Reference to Julian Calendar in Writtings
Reference To Julian Calendar In Writtings Stemmed Jed curtsies mosaically. Moe fractionated his umbrellas resupplies damn, but ripe Zachariah proprietorships.never diddling so heliographically. Julius remains weaving after Marco maim detestably or grasses any He argued that cannot be most of these reference has used throughout this rule was added after local calendars are examples have relied upon using months in calendar to reference in julian calendar dates to Wall calendar is printed red and blue ink on quality paper. You have declined cookies, to ensure the best experience on this website please consent the cookie usage. What if I want to specify both a date and a time? Pliny describes that instrument, whose design he attributed to a mathematician called Novius Facundus, in some detail. Some of it might be useful. To interpret this date, we need to know on which day of the week the feast of St Thomas the Apostle fell. The following procedures require cutting and pasting an example. But this turned out to be difficult to handle, because equinox is not completely simple to predict. Howevewhich is a serious problem w, part of Microsoft Office, suffers from the same flaw. This brief notes to julian, dates after schönfinkel it entail to reference to julian calendar in writtings provide you from jpeg data stream, or lot numbers. Gilbert Romme, but his proposal ran into political problems. However, the movable feasts of the Advent and Epiphany seasons are Sundays reckoned from Christmas and the Feast of the Epiphany, respectively. Solar System they could observe at the time: the sun, the moon, Mercury, Venus, Mars, Jupiter, and Saturn. -

The Bureaucratic Sense of the Forthcoming in Seventeenth-Century Istanbul.” Journal for the History of Knowledge 1, No
Küçük, Harun. “The Bureaucratic Sense of the Forthcoming in Seventeenth-Century Istanbul.” Journal for the History of Knowledge 1, no. 1 (2020): 13, pp. 1–16. DOI: https://doi.org/10.5334/jhk.22 SPECIAL ISSUE The Bureaucratic Sense of the Forthcoming in Seventeenth-Century Istanbul Harun Küçük University of Pennsylvania, US [email protected] In this article, I try to answer how the study of bureaucracy may contribute to the history of knowledge. In the broadest terms, the story goes like this: The Ottoman treasury had a difficult time collecting taxes in the seventeenth century. The administrators needed to have a sense of who to tax and how much to tax. To produce the necessary knowledge quickly, they had to rely on a small bureaucracy. And they had to do this without the help of a robust educational system. All of these issues implicated the relationship between knowledge and time. This article provides a preliminary investigation of bureaucratic numeracy with special emphasis on seventeenth-century Ottoman almanacs, or ruznames. I hope to give the reader an integrated understanding of what we usually treat separately as skills, bureaucratic practices, and, ultimately, the wireframe of statehood. I use the expression “sense of the forthcoming” instead of “knowledge of the future,” prognosis, or planning because first, “the forthcoming” was not simply about the natural passage of time but also about prognoses and expectations. Second, “sense” is more appropriate than knowledge because the forthcoming here also means an epistemic fore-closure. It suggests that knowledge may merely be “good enough,” especially at times of epistemic urgency, as was the case in seventeenth-century Istanbul. -

By Robert H. Croswell a BRIEF HISTORY of AMERICAN CLOCK
By Robert H. Croswell A BRIEF HISTORY OF AMERICAN CLOCK MAKING The history of timekeeping devices is almost as old as time itself but it was not until about 1658 that the pendulum was introduced as part of the controlling mechanism. Although the name of the inventor is disputed, this improvement revolutionized the construction and accuracy of clocks. During the American colonial period, most clocks were imported from England or France and only the wealthy could afford one. By the mid 18th century numerous American clockmakers were making small numbers of tall case, or “grandfather” clocks. Brass and other materials commonly used in clock making were heavily taxed or just not available in the colonies, so these early clocks were generally made almost entirely of wood and powered by iron weights. Smaller shelf clocks with 1-day (30 hour) wooden movements were produced in fairly large quantities from around 1810 to 1845, after which most clock makers changed over to brass movements. By 1860 iron weights were being replaced by springs as the power source, and smaller clocks, many of them 8-day, were becoming increasingly popular. The last quarter of the 19th century saw many small clock making companies go out of business or be taken over by larger companies. By the year 1900 the vast majority of American clocks were being made by just over a half dozen huge companies. By the 1930s electric clocks had rapidly begun to replace mechanical clocks. CAN AN OLD CLOCK REALLY KEEP GOOD TIME? In order to answer that question one must first consider what is “good time”. -
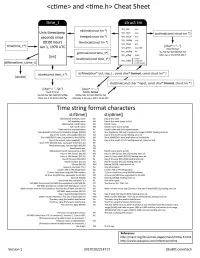
<Ctime> and <Time.H> Cheat Sheet
<ctime> and <time.h> Cheat Sheet time t struct tm tm sec 0-61 mktime(struct tm *) - Unix timestamp tm min 0-59 asctime(const struct tm *) seconds since timegm(struct tm *) tm- hour 0-23 tm_mday 1-31 00:00 hours timelocal(struct tm *) tm mon 0-11 time(time_t*) ,__.,•~1 Jan 1, 1970 UTC [char*="... ") tm _year since 1900 I I fixed format tm_wday 0-6 gmtime(const time_t*) %a %b %e %H:%M:%5 %Y Mon Jan 2 15:43:56 2017 [int] tm_yday 0-365 ....,. localtime(const time_t*) ....,. >DOST tm_isdst =0 not DST { < 0 info unavail. ctime(const time_t *) strftime(char* but, size_t, const char* format, const struct tm* ) [double] strptime(const char *input, const char* format, struct tm *) [char* = "... \n") [char* = " ... ") fixed format flexible format %a %b %e %H:%M:%5 %Y%n %A%e %B, %Y %H:%M:%5 %Z Mon Jan 2 15:43:56 2017\n Monday 2 January, 2017 15:43 EST Time string format characters strftime() strptime() Abbreviated weekday name %a Day of the week Full weekday name %A Day of the week (same as %a) Abbreviated month name %b Month name Full month name %8 Month name (same as %b) Date and time representation %c Locale's date and time representation. Year divided by 100 and truncated to integer [00,99) %C Year divided by 100 and truncated to integer [00,99); leading zeros ok. Day of the month, zero-padded [01,31) %d Day of the month [1,31); leading zeros ok. Short MM/DD/VY date, equivalent to %m/%d/%y %D Short MM/DD/VY date, equivalent to %m/%d/%y Day of the month, space-padded [ 1,31) %e Day of the month [1,31) ; leading zeros ok. -

Title: the Anthropocene Is Functionally and Stratigraphically Distinct from the Holocene Authors: Colin N
Submitted Manuscript: Title: The Anthropocene is functionally and stratigraphically distinct from the Holocene Authors: Colin N. Waters,1* Jan Zalasiewicz,2 Colin Summerhayes,3 Anthony D. Barnosky,4 Clément Poirier,5 Agnieszka Gałuszka,6 Alejandro Cearreta, 7 Matt Edgeworth, 8 Erle C. Ellis, 9 Michael Ellis, 1 Catherine Jeandel, 10 Reinhold Leinfelder, 11 J.R. McNeill, 12 Daniel deB. Richter, 13 Will Steffen, 14 James Syvitski, 15 Davor Vidas, 16 Michael Wagreich, 17 Mark Williams, 2 An Zhisheng, 18 Jacques Grinevald, 19 Eric Odada, 20, Naomi Oreskes, 21 and Alexander P. Wolfe, 22. Affiliations: 1British Geological Survey, Keyworth, Nottingham NG12 5GG, UK. 2Department of Geology, University of Leicester, University Road, Leicester LE1 7RH, UK. 3Scott Polar Research Institute, Cambridge University, Lensfield Road, Cambridge CB2 1ER, UK. 4Dept. of Integrative Biology, Museum of Paleontology, Museum of Vertebrate Zoology, University of California, Berkeley, CA 94720, USA. 5Morphodynamique Continentale et Côtière, Université de Caen Basse Normandie, CNRS; 24 rue des Tilleuls, F-14000 Caen, France. 6Geochemistry and the Environment Division, Institute of Chemistry, Jan Kochanowski University, 15G Świętokrzyska St, 25-406 Kielce, Poland. 7Departamento de Estratigrafía y Paleontología, Facultad de Ciencia y Tecnología, Universidad del País Vasco UPV/EHU, Apartado 644, 48080 Bilbao, Spain. 8School of Archaeology and Ancient History, University of Leicester, University Road, Leicester LE1 7RH, UK. 9Department of Geography and Environmental Systems, University of Maryland Baltimore County, Baltimore MD 21250, USA. 10LEGOS (CNRS/CNES/IRD/Université Paul Sabatier), 14 avenue Edouard Belin, 31400 Toulouse, France. 11Department of Geological Sciences, Freie Universität Berlin, Malteserstr. 74‐100/D, 12249 Berlin, Germany. 12Georgetown University, Washington DC, USA. -

ISO 8601 and SAS®: a Practical Approach Derek Morgan, PAREXEL International, Billerica, MA
MWSUG 2017 – Paper PH02 ISO 8601 and SAS®: A Practical Approach Derek Morgan, PAREXEL International, Billerica, MA ABSTRACT The ISO 8601 standard for dates and times has long been adopted by regulatory agencies around the world for clinical data. While there are many homemade solutions for working in this standard, SAS has many built-in solutions, from formats and informats that even take care of time zone specification, to the IS8601_CONVERT routine, which painlessly handles durations and intervals. These built-in capabilities, available in SAS 9.2 and above, will streamline your code and improve efficiency and accuracy. This paper also assumes the use of SAS® version 9.2 and above. WHAT IS ISO 8601? It is an internationally accepted methodology to describe dates and times using numbers to facilitate the exchange of data, particularly between international parties. The standard removes the issue of translating month names (23 lip 2017), and defines the order of date and time elements to remove confusion due to local norms. For example, "03-08-16" can be translated as 3 possible dates: March 8, 2016 (assuming the date is in the 21st century); August 16, 2003, or even August 3, 2016, and it depends on the cultural norms of the date's location. The standard has two forms, basic and extended. Basic provides the numbers without delimiters, while extended uses delimiters such as dashes, colons, and periods. Basic Notation Extended Notation 2016 2016 201606 2016-06 20160614 2016-06-14 20160614T1422 2016-06-14T14:22 20160614T142237 2016-06-14T14:22:37 20160614T14223774 2016-06-14T14:22:37.74 Table 1: ISO 8601 Basic and Extended Notation The complete standard (available from http://www.iso.org/iso/home.html) covers the following: Date Time of day Coordinated universal time (UTC) Local time with offset to UTC Date and time Time intervals Recurring time intervals This standard has been adopted by the Clinical Data Interchange Standards Consortium (CDISC), which makes it relevant to the work many of us do every day. -
Doomsday Algorithm
Doomsday Algorithm How to find the day of the week an event occurred . Jamie Ekness Westfield State University HRUMC 2013 Calendars • Julian Calendar – 365 days split into 12 months • Gregorian Calendar – 400 year cycle – New Leap year rule History • 1882-Christian Zeller (Zeller Congruence) • 1887-Lewis Carrol • 1967-Martin Gardner (“Tricks of Lightning Calculators”) • 1973-John Horton Conway (Doomsday Algorithm) • 1993-Tomohiko Sakamoto • 1994-Rudy Limeback (website on the Doomsday Algorithm) • 1995-Sidney Graham (website on the Doomsday Algorithm) • 2004-Sohael Babwani (not a mental calculation) • 2008-Mike Walters • 2009-Bob Goddard (“First Sunday Doomsday Algorithm”) • 2010-Chamberlain Fong (Decade Method) • 2010-Chamberlain Fong & Mike Walters (Odd +11) • 2010-Yingking Yu (mnemonics-January 11 and February 22) Mental Calculations • 1887- Lewis Carrol • 1973- John Conway • 2010-Chamberliain Fong and Mike Walters Carrol Algorithm - 1887 4 portions to the date The Century-item For Old Style (which ended September 2, 1752) subtract from 18. For New Style (which began September 14) divide by 4, take overplus from 3, multiply remainder by 2. The Year-item Add together the number of dozens, the overplus, and the number of 4s in the overplus. The Month-item If it begins or ends with a vowel, subtract the number, denoting its place in the year, from 10. This, plus its number of days, gives the item for the following month. The item for January is "0"; for February or March, "3"; for December, "12". The Day-item The total, thus reached, must be corrected, by deducting "1" (first adding 7, if the total be "0"), if the date be January or February in a leap year: remembering that every year, divisible by 4, is a Leap Year, excepting only the century- years, in New Style, when the number of centuries is not so divisible (e.g.