Initial Flare Symptoms Resulting from Use of LHRH Agonist in Metastatic Prostate Cancer: Systematic Review and Economic Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download PDF File
Ginekologia Polska 2019, vol. 90, no. 9, 520–526 Copyright © 2019 Via Medica ORIGINAL PAPER / GYNECologY ISSN 0017–0011 DOI: 10.5603/GP.2019.0091 Anti-androgenic therapy in young patients and its impact on intensity of hirsutism, acne, menstrual pain intensity and sexuality — a preliminary study Anna Fuchs, Aleksandra Matonog, Paulina Sieradzka, Joanna Pilarska, Aleksandra Hauzer, Iwona Czech, Agnieszka Drosdzol-Cop Department of Pregnancy Pathology, Department of Woman’s Health, School of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland ABSTRACT Objectives: Using anti-androgenic contraception is one of the methods of birth control. It also has a significant, non-con- traceptive impact on women’s body. These drugs can be used in various endocrinological disorders, because of their ability to reduce the level of male hormones. The aim of our study is to establish a correlation between taking different types of anti-androgenic drugs and intensity of hirsutism, acne, menstrual pain intensity and sexuality . Material and methods: 570 women in childbearing age that had been using oral contraception for at least three months took part in our research. We examined women and asked them about quality of life, health, direct causes and effects of that treatment, intensity of acne and menstrual pain before and after. Our research group has been divided according to the type of gestagen contained in the contraceptive pill: dienogest, cyproterone, chlormadynone and drospirenone. Ad- ditionally, the control group consisted of women taking oral contraceptives without antiandrogenic component. Results: The mean age of the studied group was 23 years ± 3.23. 225 of 570 women complained of hirsutism. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

Epigenetic Therapy with Panobinostat Combined with Bicalutamide Rechallenge in Castration- Resistant Prostate Cancer Anna C
Published OnlineFirst January 3, 2019; DOI: 10.1158/1078-0432.CCR-18-1589 Clinical Trials: Targeted Therapy Clinical Cancer Research Epigenetic Therapy with Panobinostat Combined with Bicalutamide Rechallenge in Castration- Resistant Prostate Cancer Anna C. Ferrari1, Joshi J. Alumkal2, Mark N. Stein3, Mary-Ellen Taplin4, James Babb5, Ethan S. Barnett6, Alejandro Gomez-Pinillos5, Xiaomei Liu5, Dirk Moore6, Robert DiPaola7, and Tomasz M. Beer2 Abstract Purpose: This study assesses the action of panobino- Results: In the model, panobinostat/bicalutamide demon- stat, a histone deacetylase inhibitor (HDACI), in restor- strated synergistic antitumor effect while reducing AR activity. ing sensitivity to bicalutamide in a castration-resistant The dose-limiting toxicity was not reached. The probabilities of prostate cancer (CRPC) model and the efficacy and safety remaining rPF were 47.5% in the A arm and 38.5% in the B arm, of the panobinostat/bicalutamide combination in CRPC exceeding the protocol-specified threshold of 35%. The A arm patients resistant to second-line antiandrogen therapy but not the B arm exceeded expectations for times (medians) to (2ndLAARx). rP (33.9 and 10 weeks), and from PSA progression to rP (24 and Patients and Methods: The CWR22PC xenograft and 5.9 weeks). A arm/B arm events included: adverse events (AE), isogenic cell line were tested for drug interactions on 62%/19%; treatment stopped for AEs, 27.5%/11.5%; dose tumor cell growth and on the androgen receptor (AR), reduction required, 41%/4%. The principal A-arm grade 3 AR-splice variant7, and AR targets. A phase I trial had a AEs were thrombocytopenia (31%) and fatigue (14%). -

Comparing the Effects of Combined Oral Contraceptives Containing Progestins with Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis In
JMIR RESEARCH PROTOCOLS Amiri et al Review Comparing the Effects of Combined Oral Contraceptives Containing Progestins With Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis in Patients With Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis Mina Amiri1,2, PhD, Postdoc; Fahimeh Ramezani Tehrani2, MD; Fatemeh Nahidi3, PhD; Ali Kabir4, MD, MPH, PhD; Fereidoun Azizi5, MD 1Students Research Committee, School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 2Reproductive Endocrinology Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 3School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 4Minimally Invasive Surgery Research Center, Iran University of Medical Sciences, Tehran, Islamic Republic Of Iran 5Endocrine Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran Corresponding Author: Fahimeh Ramezani Tehrani, MD Reproductive Endocrinology Research Center Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences 24 Parvaneh Yaman Street, Velenjak, PO Box 19395-4763 Tehran, 1985717413 Islamic Republic Of Iran Phone: 98 21 22432500 Email: [email protected] Abstract Background: Different products of combined oral contraceptives (COCs) can improve clinical and biochemical findings in patients with polycystic ovary syndrome (PCOS) through suppression of the hypothalamic-pituitary-gonadal (HPG) axis. Objective: This systematic review and meta-analysis aimed to compare the effects of COCs containing progestins with low androgenic and antiandrogenic activities on the HPG axis in patients with PCOS. -
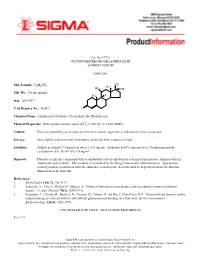
Fluoxymesterone-Dea Schedule Iii Androfluorene
Cat. No. F7751 FLUOXYMESTERONE--DEA SCHEDULE III ANDROFLUORENE Androgen. OH Mol. Formula: C20H29FO3 HO H3C CH3 Mol. Wt.: 336.45 (anhyd.) F H3C m.p.: 288-290°C CAS Registry No.: 76-43-7 O Chemical Name: 4-Androsten-9a-fluoro-17a-methyl-11b,17b-diol-3-one 22 Physical Properties: White photosensitive solid. [a] D = +102.34° (c = 0.47, EtOH). Caution: Due care should be exercised to prevent skin contact, ingestion or inhalation of this compound. Storage: Store tightly sealed at room temperature, protected from exposure to light. Solubility: Soluble in ethanol (7.3 mg/ml) or water (< 0.5 mg/ml). Solubility in 45% aqueous (w/v) 2-hydroxypropyl-b- cyclodextrin (Cat. No. H-107): 6.4 mg/ml. Disposal: Dissolve or mix the compound with a combustible solvent and burn in a chemical incinerator equipped with an afterburner and scrubber. This product is controlled by the Drug Enforcement Administration. Appropriate security must be maintained until the substance is destroyed. Records must be kept which detail the ultimate disposition of the material. References: 1. Merck Index 11th Ed., No. 4113. 2. Saborido, A., Vila, J., Molano, F., Megias, A. “Effect of steroids on mitochondria and sarcotubular system of skeletal muscle.” J. Appl. Physiol. 70(3), 1038 (1991). 3. Fernandez, L., Chirino, R., Boada, L.D., Navarro, D., Cabrera, N., del Rio, I., Diaz-Chico, B.N. “Stanozolol and danazol, unlike natural androgens, interact with the low affinity glucocorticoid-binding sites from male rat liver microsomes.” Endocrinology 134(3), 1401 (1994). CONTROLLED SUBSTANCE - DEA LICENSE REQUIRED (III) Rev. -

Feminizing Hormone Therapy
FEMINIZING HORMONE THERAPY Julie Thompson, PA-C Medical Director of Trans Health, Fenway Health April 2020 fenwayhealth.org GOALS AND OBJECTIVES 1. Review process of initiating hormone therapy through the informed consent model 2. Provide an overview of feminizing hormone therapy 3. Review realistic expectations and benefits of hormone therapy vs their associated risks 4. Discuss recommendations for monitoring fenwayhealth.org PROTOCOLS AND STANDARDS OF CARE fenwayhealth.org WPATH STANDARDS OF CARE, 2011 The criteria for hormone therapy are as follows: 1. Well-documented, persistent (at least 6mo) gender dysphoria 2. Capacity to make a fully informed decision and to consent for treatment 3. Age of majority in a given country 4. If significant medical or mental health concerns are present, they must be reasonably well controlled fenwayhealth.org INFORMED CONSENT MODEL ▪ Requires healthcare provider to ▪ Effectively communicate benefits, risks and alternatives of treatment to patient ▪ Assess that the patient is able to understand and consent to the treatment ▪ Informed consent model does not preclude mental health care! ▪ Recognizes that prescribing decision ultimately rests with clinical judgment of provider working together with the patient ▪ Recognizes patient autonomy and empowers self-agency ▪ Decreases barriers to medically necessary care fenwayhealth.org INITIAL VISITS ▪ Review history of gender experience and patient’s goals ▪ Document prior hormone use ▪ Assess appropriateness for gender affirming medical treatment ▪ WPATH criteria -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole Mass Spectrom
No. LCMSMS-065E Liquid Chromatography Mass Spectrometry Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole No. LCMSMS-65E Mass Spectrometry This application news presents a method for the determination of 17 hormone residues in milk using Shimadzu Ultra-High-Performance Liquid Chromatograph (UHPLC) LC-30A and Triple Quadrupole Mass Spectrometer LCMS- 8040. After sample pretreatment, the compounds in the milk matrix were separated using UPLC LC-30A and analyzed via Triple Quadrupole Mass Spectrometer LCMS-8040. All 17 hormones displayed good linearity within their respective concentration range, with correlation coefficient in the range of 0.9974 and 0.9999. The RSD% of retention time and peak area of 17 hormones at the low-, mid- and high- concentrations were in the range of 0.0102-0.161% and 0.563-6.55% respectively, indicating good instrument precision. Method validation was conducted and the matrix spike recovery of milk ranged between 61.00-110.9%. The limit of quantitation was 0.14-0.975 g/kg, and it meets the requirement for detection of hormones in milk. Keywords: Hormones; Milk; Solid phase extraction; Ultra performance liquid chromatograph; Triple quadrupole mass spectrometry ■ Introduction Since 2008’s melamine-tainted milk scandal, the With reference to China’s national standard GB/T adulteration of milk powder has become a major 21981-2008 "Hormone Multi-Residue Detection food safety concern. In recent years, another case of Method for Animal-derived Food - LC-MS Method", dairy product safety is suspected to cause "infant a method utilizing solid phase extraction, ultra- sexual precocity" (also known as precocious puberty) performance liquid chromatography and triple and has become another major issue challenging the quadrupole mass spectrometry was developed for dairy industry in China. -

INTEGRIS Formulary July 2017
INTEGRIS Formulary July 2017 Foreword FORMULARY EXCLUDED THERAPEUTIC DRUG This document represents the efforts of the MedImpact Healthcare Systems THERAPEUTIC DRUGS CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide ALTERNATIVES physicians and pharmacists with a method to evaluate the safety, efficacy and cost- clindamycin/tretinoin, ACNE AGENTS, effectiveness of commercially available drug products. A structured approach to the VELTIN drug selection process is essential in ensuring continuing patient access to rational ZIANA TOPICAL drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ANALGESICS, KADIAN prescribing decisions that reflect the most current clinical consensus associated ER, NUCYNTA, NARCOTICS with drug therapy decisions. NUCYNTA ER ANALGESICS, This is accomplished through the auspices of the MedImpact P & T and Formulary BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, fentanyl citrate ANALGESICS, LAZANDA, lozenge NARCOTICS As you use this Formulary, you are encouraged to review the information and ONSOLIS, provide your input and comments to the MedImpact P & T and Formulary SUBSYS Committees. immediate-release GRALISE ANTICONVULSANTS The MedImpact P & T -

Anabolic Steroids/Androgens Pa Summary
ANABOLIC STEROIDS/ANDROGENS PA SUMMARY PREFERRED Anadrol-50, Danazol, Fluoxymesterone, Methitest, Oxandrolone, Testosterone Cypionate Injection, Testosterone Enanthate Injection NON-PREFERRED Android, Testred LENGTH OF AUTHORIZATION: Varies NOTE: All preferred and non-preferred agents require prior authorization. See PA criteria labeled “Topical Testosterone” for Androderm, Androgel, Striant, and Testim. The criteria details below are for the outpatient pharmacy program. If an injectable medication is being administered in a physician’s office then the criteria information below does not apply. Instead, the physician’s office must bill this drug through the DCH physician’s injectable program and not the outpatient pharmacy program. Information regarding the physician’s injectable program can be located at www.mmis.georgia.gov. PA CRITERIA: For Anadrol-50 Approvable for the following diagnoses: anemia caused by deficient red blood cell production, acquired or congenital aplastic anemia, myelofibrosis, hypoplastic anemia due to administration of myelotoxic drugs Also approvable for HIV or AIDS wasting when significant weight loss is documented in members currently receiving nutritional support For Danazol Approvable for the following diagnoses: endometriosis, fibrocystic breast disease, hereditary angioedema For Fluoxymesterone, Methyltestosterone (Android, Methitest, Testred), Testosterone Cypionate or Enanthate Injection Approvable in male members 12 years of age or older for the following diagnoses: primary hypogonadism, secondary