Osteoarthritis of the Carpometacarpal Thumb Joint Patient Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Study on the Absence of Palmaris Longus in a Multi-Racial Population
108472 NV-OA7 pg26-28.qxd 11/05/2007 05:02 PM Page 26 (Black plate) Malaysian Orthopaedic Journal 2007 Vol 1 No 1 SA Roohi, etal A Study on the Absence of Palmaris Longus in a Multi- racial Population SA Roohi, MS (Ortho) (UKM), L Choon-Sian, MD (UKM), A Shalimar, MS (Ortho) (UKM), GH Tan, MS (Ortho) (UKM), AS Naicker, M Med Rehab (UM) Hospital Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia ABSTRACT Most standard textbooks of hand surgery quote the prevalence of absence of palmaris longus at around 15%3-5. Palmaris longus is a dispensable muscle with a long tendon However, this figure varies considerably in different ethnic which is very useful in reconstructive surgery. It is absent groups. A study by Thompson et al6 on 300 Caucasian 2.8 to 24% of the population depending on the race/ethnicity subjects found that palmaris longus was absent unilaterally in studied. Four hundred and fifty healthy subjects (equally 16%, and bilaterally in 9% of the study sample for an overall distributed among Malaysia’s 3 major ethnic groups) were prevalence of absence of 24%. Similarly, George7 noted on clinically examined for the presence or absence of palmaris 276 cadavers of European descent that its absence was 13% longus. This tendon was found to be absent unilaterally in unilaterally, 8.7% bilaterally for an overall absence of 15.2%. 6.4% of study subjects, and bilaterally in 2.9% of study Another cadaveric study by Vanderhooft8 in Seattle, USA participants. Malays have a high prevalence of palmaris reported its overall absence to be 12%. -

Complex Regional Pain Syndrome Type I (Shoulder-Hand Syndrome) in an Elderly Patient After Open Cardiac Surgical Intervention; a Case Report
Eastern Journal of Medicine 16 (2011) 56-58 L. Ediz et al / CRPS type I after open cardiac Surgery Case Report Complex regional pain syndrome type I (shoulder-hand syndrome) in an elderly patient after open cardiac surgical intervention; a case report Levent Ediza*, Mehmet Fethi Ceylanb , Özcan Hıza, İbrahim Tekeoğlu c a Department of Physical Medicine and Rehabilitation, Yüzüncü Yıl University Medical Faculty, Van, Turkey b Department of Orthopaedics and Traumatology,Yüzüncü Yıl University Medical Faculty, Van, Turkey c Department of Rheumatology, Yüzüncü Yıl University Medical Faculty, Van, Turkey Abstract. We described the first case report in the literature who developed Complex Regional Pain Syndrome (CRPS type I) symptoms in his right shoulder and right hand within 15 days after open cardiac surgery and discussed shoulder-hand syndrome (CRPS type I) and frozen shoulder diagnosis along with the reasons of no report of CRPS type I in these patients. We also speculated whether frozen shoulder seen in postthoracotomy and postcardiac surgery patients might be CRPS type I in fact. Key words: Complex regional pain syndrome, cardiac surgery, frozen shoulder 1. Introduction Improper patient positioning, muscle division, perioperative nerve injury, rib spreading, and Complex Regional Pain Syndrome (CRPS) is consequent postoperative pain influence the complication of injuries which is seen at the patient's postoperative shoulder function and distal end of the affected area characterized by quality of life (5). In a study Tuten HR et al pain, allodyni, hyperalgesia, edema, abnormal retrospectively evaluated for the incidence of vasomotor and sudomotor activity, movement adhesive capsulitis of the shoulder of two disorders, joint stiffness, regional osteopenia, and hundred fourteen consecutive male cardiac dystrophic changes in soft tissue (1,2). -

Fundamental Shoulder Exercises
FUNDAMENTAL SHOULDER EXERCISES RANGE OF MOTION EXERCISES 1. L-BAR FLEXION Lie on back and grip L-Bar between index finger and thumb, elbows straight. Raise both arms overhead as far as possible keeping thumbs up. Hold for _____ seconds and repeat _____ times. 2. L-BAR EXTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using unin- volved arm, push involved arm into external rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. 3. L-BAR INTERNAL ROTATION, SCAPULAR PLANE Lie on back with involved arm 450 from body and elbow bent at 900. Grip L-Bar in the hand of involved arm and keep elbow in flexed position. Using the uninvolved arm, push involved arm into internal rotation. Hold for _____ seconds, return to starting position. Repeat _____ times. Dr. Meisterling (800) 423-1088 1 of 2 STRENGTHENING EXERCISES 1. TUBING, EXTERNAL ROTATION Standing with involved elbow fixed at side, elbow bent to 900 and involved arm across the front of the body. Grip tubing handle while the other end of tubing is fixed. Pull out with arm, keeping elbow at side. Return tubing slowly and controlled. Perform _____ sets of _____ reps. 2. TUBING, INTERNAL ROTATION Standing with elbow at side fixed at 900 and shoulder rotated out. Grip tubing handle while other end of tubing is fixed. Pull arm across body keeping elbow at side. Return tubing slowly and controlled. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Isolated Trapezoid Fractures a Case Report with Compilation of the Literature
Bulletin of the NYU Hospital for Joint Diseases 2008;66(1):57-60 57 Isolated Trapezoid Fractures A Case Report with Compilation of the Literature Konrad I. Gruson, M.D., Kevin M. Kaplan, M.D., and Nader Paksima, D.O., M.P.H. Abstract as an axial load5,6 or bending stress7 transmitted indirectly Isolated fractures of the trapezoid bone have been rarely to the trapezoid through the second metacarpal. We present reported in the literature, the mechanism of injury being a case of an acute, isolated trapezoid fracture that resulted an axial or bending load transmitted through the second from direct trauma to the distal carpus and that was treated metacarpal. We report a case of an isolated, nondisplaced nonoperatively. Additionally, strategies for diagnosis and trapezoid fracture that was sustained by direct trauma treatment, as well as a synthesis of the published results and subsequently treated successfully in a short-arm cast. for both isolated and concomitant trapezoid fractures, are Diagnostic and treatment strategies for isolated fractures presented. of the trapezoid bone are reviewed as well as the results of operative and nonoperative treatment. Case Report A 25-year-old right-hand dominant male presented to the ractures of the carpus most commonly involve the emergency room (ER) complaining of isolated right-wrist scaphoid,1 with typical physical examination findings pain and swelling of 1 day’s duration. The patient stated Fof “snuffbox” tenderness. This presentation is fre- that a heavy metal door at work had closed onto the back quently the result of the patient falling onto an outstretched of his wrist causing an immediate onset of swelling and hand. -

Hand, Elbow, Wrist Pain
Physical and Sports Therapy Hand, Elbow, Wrist Pain The hand is a wondrously complex structure of tiny bones, muscles, ligaments, and tendons which work together to perform tasks. The wrist and elbow are stabilizing joints that support the steady use of the hand and provide attachment points for the muscles that control the hand and wrist. All three of these areas are prone to injury from overuse or trauma. Their complexity requires the skills of an expert for proper rehabilitation from injury. Some Hand, Wrist, and Elbow Issues Include: Tennis/Golfer’s Elbow: Tendonitis, or inflammation of the tendons, at the muscular attachments near the elbow. Symptoms typically include tenderness on the sides of the elbow, which increase with use of the wrist and hand, such as shaking hands or picking up a gallon of milk. Tendonitis responds well to therapy, using eccentric exercise, stretching, and various manual therapy techniques. Carpal Tunnel Syndrome: Compression of the Median Nerve at the hand/base of your wrist. Symptoms include pain, numbness, and tingling of the first three fingers. The condition is well-known for waking people at night. Research supports the use of therapy, particularly in the early phase, for alleviation of the compression through stretching and activity modification. Research indicates that the longer symptoms are present before initiating treatment, the worse the outcome for therapy and surgical intervention due to underlying physiological changes of the nerve. What can Physical or Occupational therapy do for Hand, Wrist, or Elbow pain? Hand, wrist, and elbow injuries are commonly caused by trauma, such as a fall or overuse. -

Wrist and Hand Examina[On
Wrist and Hand Examinaon Daniel Lueders, MD Assistant Professor Physical Medicine and Rehabilitaon Objecves • Understand the osseous, ligamentous, tendinous, and neural anatomy of the wrist and hand • Outline palpable superficial landmarks in the wrist and hand • Outline evaluaon of and differen.aon between nerves to the wrist and hand • Describe special tes.ng of wrist and hand Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Inspec.on • Ecchymosis • Erythema • Deformity • Laceraon Inspec.on • Common Finger Deformies • Swan Neck Deformity • Boutonniere Deformity • Hypertrophic nodules • Heberden’s, Bouchard’s Inspec.on • Swan Neck Deformity • PIP hyperextension, DIP flexion • Pathology is at PIP joint • Insufficiency of volar/palmar plate and suppor.ng structures • Distally, the FDP tendon .ghtens from PIP extension causing secondary DIP flexion • Alternavely, extensor tendon rupture produces similar deformity Inspec.on • Boutonniere Deformity • PIP flexion, DIP hyperextension • Pathology is at PIP joint • Commonly occurs from insufficiency of dorsal and lateral suppor.ng structures at PIP joint • Lateral bands migrate volar/palmar, creang increased flexion moment • Results in PIP “buTon hole” effect dorsally Inspec.on • Nodules • Osteoarthri.c • Hypertrophic changes of OA • PIP - Bouchard’s nodule • DIP - Heberden’s nodule • Rheumatoid Arthri.s • MCP joints affected most • Distal radioulnar joint can also be affected -
Stretching and Positioning Regime for Upper Limb
Information for patients and visitors Stretching and Positioning Regime for Upper Limb Physiotherapy Department This leaflet has been designed to remind you of the exercises you Community & Therapy Services have been taught, the correct techniques and who to contact with any queries. For more information about our Trust and the services we provide please visit our website: www.nlg.nhs.uk Information for patients and visitors Muscle Tone Muscle tone is an unconscious low level contraction of your muscles while they are at rest. The purpose of this is to keep your muscles primed and ready to generate movement. Several neurological causes may change a person’s muscle tone to increase or decrease resulting in a lack of movement. Over time, a lack of movement can cause stiffness, pain, and spasticity. In severe cases this may also lead to contractures. Spasticity Spasticity can be defined as a tightening or stiffness of the muscle due to increased muscle tone. It can interfere with normal functioning. It can also greatly increase fatigue. However, exercise, properly done, is vital in managing spasticity. The following tips may prove helpful: • Avoid positions that make the spasticity worse • Daily stretching of muscles to their full length will help to manage the tightness of spasticity, and allow for optimal movement • Moving a tight muscle to a new position may result in an increase in spasticity. If this happens, allow a few minutes for the muscles to relax • When exercising, try to keep head straight • Sudden changes in spasticity may -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -
Symptomatic Carpal Coalition: Scaphotrapezial Joint
A Case Report & Literature Review E. Campaigniac et al Symptomatic Carpal Coalition: Scaphotrapezial Joint Erin Campaigniac, MD, Mark Eskander, MD, and Marci Jones, MD joint formation may be radiographically visible, with joint Abstract space narrowing wherein bone or fibrous material is present Carpal coalition is an uncommon congenital in place of articular cartilage.2,4 Minaar8 developed a classifi- abnormality that arises from incomplete cavita- cation system based on his observations of 12 lunotriquetral tion of the common cartilaginous precursor that coalitions and their differences in coalition: ◾ Type I, incomplete fusion resembling pseudarthrosis or syn- forms the carpal bones. When carpal coalition chondrosis is discovered, it is typically an asymptomatic ◾ Type II, proximal fusion with a distal notching incidental radiographic finding, and is often ◾ Type III, complete fusion, and bilateral. We present a case of symptomatic ◾ Type IV, complete fusion associated with other anomalies. unilateral carpal coalition of the scaphotrapezial Although these 4 types were based on lunotriquetral coali- joint, which was treated by excising the fibrous tions, this classification system is used to describe the coalition coalition and placing an interposition fat graft. of any carpal bone. This treatment was effective in alleviating the Carpal coalition is uncommon, and the reported prevalence 2,5,6,9 patient’s symptoms. is close to 0.1%. There is, however, an increase of up to 1.5% in patients of African descent, and 9.5% in the West Af- rican -
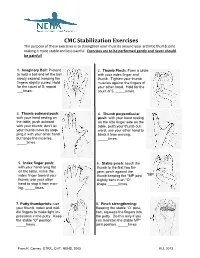
CMC Stabilization Exercises the Purpose of These Exercises Is to Strengthen Your Muscles Around Your Arthritic Thumb Joint Making It More Stable and Less Painful
CMC Stabilization Exercises The purpose of these exercises is to strengthen your muscles around your arthritic thumb joint making it more stable and less painful. Exercises are to be performed gently and never should be painful! 1. Imaginary Ball: Pretend 2. Thumb Pinch: Form a circle to hold a ball and let the ball with your index finger and slowly expand, keeping the thumb. Tighten your thumb fingers slightly curled. Hold muscles against the fingers of for the count of 5, repeat your other hand. Hold for the ___times. count of 5, _____times. 3. Thumb outward push: 4. Thumb perpendicular with your hand resting on push: with your hand resting the table, push outward on the little finger side on the with your thumb; don’t let table, push your thumb out- your thumb move by stop- ward; use your other hand to ping it with your other hand block it from moving. but tense the muscles. _____times. _____times. 5. Index finger push: 6. Stable pinch: touch the with your hand lying flat thumb to the first two fin- on the table, move the gers; pinch against the index finger toward your thumb keeping the *MP joint *MP thumb; use your other slightly bent in an “O” hand to stop it from mov- shape. _____times. ing. _____times. 7. Putty thumbprints: use 8. Pinch strengthening: your thumb, index and mid- Keeping the stable “O” posi- dle fingers to make light im- tion, squeeze the fingers into pressions in the putty. Keep the putty. Do this only if you the stable “O” position. -

Post-Operative Instructions for Flexor Tendon Repair Purpose of Surgery
Post-Operative Instructions for Flexor Tendon Repair Purpose of surgery The goal of the operation is to repair or reattach lacerated or detached flexor tendons. The flexor tendons (muscles) are responsible for flexing (bending) your fingers. What to expect after surgery? You will have a firm splint covering your forearm and the back of your hand and fingers holding your fingers flexed (bent). All your fingers will be included in the splint for any finger flexor tendon repair; and, only your thumb will be included in the splint for a thumb flexor tendon repair. You will be able to see the tips of your fingers/thumb to insure they are getting good circulation. The palm side of your fingers/thumb will be protected by a soft padding that they will be resting on while the plaster will keep your fingers bent from the nail side. You may have some numbness or tingling of fingers/thumb due to the local anesthetic injections used to help control post-operative pain (this should wear off within about 24 hours). After this first 24 hours, you may still experience some numbness and tingling in parts of the operative finger(s)/thumb if you also had a nerve repair. What should you do to help recover? While we do not anticipate significant swelling following this procedure, it would be helpful to keep your hand/wrist elevated as best you can for the first 24 hours after surgery. The thickness of the dressing will prevent the effective placement of a cold-pack. Please do not move your fingers, even if they were not operated on.