Nandrolone Decanoate: Use, Abuse and Side Effects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparison of the Effects of High Dose Testosterone and 19-Nortestosterone to a Replacement Dose of Testosterone on Strength and Body Composition in Normal Men
J. Steroid Biochem. Molec. Biol. Vol. 40, No. 4-6, pp. 607~12, 1991 0960-0760/91 $3.00 + 0.00 Printed in Great Britain Pergamon Press plc COMPARISON OF THE EFFECTS OF HIGH DOSE TESTOSTERONE AND 19-NORTESTOSTERONE TO A REPLACEMENT DOSE OF TESTOSTERONE ON STRENGTH AND BODY COMPOSITION IN NORMAL MEN KARL E. FRIEDL,* JOSEPH R. DETTORI, CHARLES J. HANNAN JR, TROY H. PATIENCE and STEPHENR. PLYMATE Exercise Physiology Division, U.S. Army Research Institute of Environmental Medicine, Natick, MA and Department of Clinical Investigation, Madigan Army Medical Center, Tacoma, WA, U.S.A. Summary--We examined the extent to which supraphysiological doses of androgen can modify body composition and strength in normally virilized men. In doubly blind tests, 30 healthy young men received testosterone enanthate (TE) or 19-nortestosterone decanoate (ND), at 100mg/wk or 300mg/wk for 6 weeks. The TE-100mg/wk group served as replacement dose comparison, maintaining pretreatment serum testosterone levels, while keeping all subjects blinded to treatment, particularly through reduction in testicular volumes. Isokinetic strength measurements were made for the biceps brachii and quadriceps femoris muscle groups before treatment and 2-3 days after the 6th injection. Small improvements were noted in all groups but the changes were highly variable; a trend to greater and more consistent strength gain occurred in the TE-300mg/wk group. There was no change in weight for TE-100 mg/wk but an average gain of 3 kg in each of the other groups. No changes in 4 skinfold thicknesses or in estimated percent body fat were observed. -
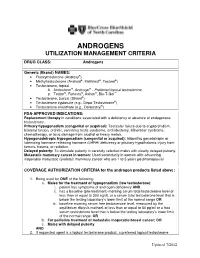
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Detectx® Serum 17Β-Estradiol Enzyme Immunoassay Kit
DetectX® Serum 17β-Estradiol Enzyme Immunoassay Kit 1 Plate Kit Catalog Number KB30-H1 5 Plate Kit Catalog Number KB30-H5 Species Independent Sample Types Validated: Multi-Species Serum and Plasma Please read this insert completely prior to using the product. For research use only. Not for use in diagnostic procedures. www.ArborAssays.com KB30-H WEB 210308 TABLE OF CONTENTS Background 3 Assay Principle 4 Related Products 4 Supplied Components 5 Storage Instructions 5 Other Materials Required 6 Precautions 6 Sample Types 7 Sample Preparation 7 Reagent Preparation 8 Assay Protocol 9 Calculation of Results 10 Typical Data 10-11 Validation Data Sensitivity, Linearity, etc. 11-13 Samples Values and Cross Reactivity 14 Warranty & Contact Information 15 Plate Layout Sheet 16 ® 2 EXPECT ASSAY ARTISTRY KB30-H WEB 210308 BACKGROUND 17β-Estradiol, C18H24O2, also known as E2 or oestradiol (1, 3, 5(10)-Estratrien-3, 17β-diol) is a key regulator of growth, differentiation, and function in a wide array of tissues, including the male and female reproductive tracts, mammary gland, brain, skeletal and cardiovascular systems. The predominant biological effects of E2 are mediated through two distinct intracellular receptors, ERα and ERβ, each encoded by unique genes possessing the functional domain characteristics of the steroid/thyroid hormone superfamily of nuclear receptors1. ERα is the predominant form expressed in the breast, uterus, cervix, and vagina. ERβ exhibits a more limited pattern and is primarily expressed in the ovary, prostate, testis, spleen, lung, hypothalamus, and thymus2. Estradiol also influences bone growth, brain development and maturation, and food intake3, and it is also critical in maintaining organ functions during severe trauma4,5. -

A Guide to Feminizing Hormones – Estrogen
1 | Feminizing Hormones A Guide to Feminizing Hormones Hormone therapy is an option that can help transgender and gender-diverse people feel more comfortable in their bodies. Like other medical treatments, there are benefits and risks. Knowing what to expect will help us work together to maximize the benefits and minimize the risks. What are hormones? Hormones are chemical messengers that tell the body’s cells how to function, when to grow, when to divide, and when to die. They regulate many functions, including growth, sex drive, hunger, thirst, digestion, metabolism, fat burning & storage, blood sugar, cholesterol levels, and reproduction. What are sex hormones? Sex hormones regulate the development of sex characteristics, including the sex organs such as genitals and ovaries/testicles. Sex hormones also affect the secondary sex characteristics that typically develop at puberty, like facial and body hair, bone growth, breast growth, and voice changes. There are three categories of sex hormones in the body: • Androgens: testosterone, dehydroepiandrosterone (DHEA), dihydrotestosterone (DHT) • Estrogens: estradiol, estriol, estrone • Progestin: progesterone Generally, “males” tend to have higher androgen levels, and “females” tend to have higher levels of estrogens and progestogens. What is hormone therapy? Hormone therapy is taking medicine to change the levels of sex hormones in your body. Changing these levels will affect your hair growth, voice pitch, fat distribution, muscle mass, and other features associated with sex and gender. Feminizing hormone therapy can help make the body look and feel less “masculine” and more “feminine" — making your body more closely match your identity. What medicines are involved? There are different kinds of medicines used to change the levels of sex hormones in your body. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

TESTOSTERONE and ANABOLIC STEROIDS Summary Testosterone Is a Hormone Naturally Produced by the Body
FactSHEET TESTOSTERONE AND ANABOLIC STEROIDS Summary Testosterone is a hormone naturally produced by the body. Low levels of testosterone can cause symptoms of fatigue, malaise, loss of sex drive, and loss of muscle tissue. These symptoms can often be treated with synthetic testosterone. Anabolic steroids are compounds related to testosterone. Using synthetic testosterone or anabolic steroids may help people with HIV-related wasting gain weight, especially muscle mass. What is testosterone? Sometimes HIV-positive men develop low testosterone levels which can cause symptoms Although it is usually thought of as a male of fatigue, muscle wasting, low (or no) sex hormone, women’s bodies also make drive, impotence, and loss of facial or body testosterone, but at much lower levels than hair. This condition is called hypogonadism. men’s. Testosterone has two different effects on Hormone replacement therapy with synthetic the body: anabolic effects which promote growth testosterone may help to relieve those and muscle building, and androgenic effects symptoms. which develop the male sex organs and secondary sex characteristics such as deepening HIV-positive women may also develop low of the voice and growth of facial hair. testosterone levels and experience symptoms of fatigue, loss of sex drive, and a decreased sense of well-being. Because the androgenic What are anabolic steroids? (masculinizing) effects of testosterone and Anabolic steroids are synthetic compounds anabolic steroids can be permanent, that resemble the natural hormone researchers have been cautious about studying testosterone. Makers of anabolic steroids these drugs in women. change the testosterone molecule slightly to 2. To treat weight loss change the balance of androgenic and anabolic effects, which can allow these drugs to build Anabolic steroids can be used in order to build muscle with fewer masculinizing effects. -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

Part I Biopharmaceuticals
1 Part I Biopharmaceuticals Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 3 1 Analogs and Antagonists of Male Sex Hormones Robert W. Brueggemeier The Ohio State University, Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, Columbus, Ohio 43210, USA 1Introduction6 2 Historical 6 3 Endogenous Male Sex Hormones 7 3.1 Occurrence and Physiological Roles 7 3.2 Biosynthesis 8 3.3 Absorption and Distribution 12 3.4 Metabolism 13 3.4.1 Reductive Metabolism 14 3.4.2 Oxidative Metabolism 17 3.5 Mechanism of Action 19 4 Synthetic Androgens 24 4.1 Current Drugs on the Market 24 4.2 Therapeutic Uses and Bioassays 25 4.3 Structure–Activity Relationships for Steroidal Androgens 26 4.3.1 Early Modifications 26 4.3.2 Methylated Derivatives 26 4.3.3 Ester Derivatives 27 4.3.4 Halo Derivatives 27 4.3.5 Other Androgen Derivatives 28 4.3.6 Summary of Structure–Activity Relationships of Steroidal Androgens 28 4.4 Nonsteroidal Androgens, Selective Androgen Receptor Modulators (SARMs) 30 4.5 Absorption, Distribution, and Metabolism 31 4.6 Toxicities 32 Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 4 Analogs and Antagonists of Male Sex Hormones 5 Anabolic Agents 32 5.1 Current Drugs on the Market 32 5.2 Therapeutic Uses and Bioassays -

Testosterone: a Metabolic Hormone in Health and Disease
D M KELLY and T H JONES Testosterone metabolic hormone 217:3 R25–R45 Review Testosterone: a metabolic hormone in health and disease Daniel M Kelly1 and T Hugh Jones1,2 Correspondence should be addressed to 1Department of Human Metabolism, Medical School, The University of Sheffield, Sheffield S10 2RX, UK 2Robert T H Jones Hague Centre for Diabetes and Endocrinology, Barnsley Hospital NHS Foundation Trust, Gawber Road, Barnsley S75 Email 2EP, UK [email protected] Abstract Testosterone is a hormone that plays a key role in carbohydrate, fat and protein metabolism. Key Words It has been known for some time that testosterone has a major influence on body fat " metabolism composition and muscle mass in the male. Testosterone deficiency is associated with an " testosterone increased fat mass (in particular central adiposity), reduced insulin sensitivity, impaired " type 2 diabetes glucose tolerance, elevated triglycerides and cholesterol and low HDL-cholesterol. All these " metabolic syndrome factors are found in the metabolic syndrome (MetS) and type 2 diabetes, contributing to cardiovascular risk. Clinical trials demonstrate that testosterone replacement therapy improves the insulin resistance found in these conditions as well as glycaemic control and also reduces body fat mass, in particular truncal adiposity, cholesterol and triglycerides. The mechanisms by which testosterone acts on pathways to control metabolism are not fully clear. There is, however, an increasing body of evidence from animal, cell and clinical studies that testosterone at the molecular level controls the expression of important regulatory proteins involved in Journal of Endocrinology glycolysis, glycogen synthesis and lipid and cholesterol metabolism. The effects of testosterone differ in the major tissues involved in insulin action, which include liver, muscle and fat, suggesting a complex regulatory influence on metabolism. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object.