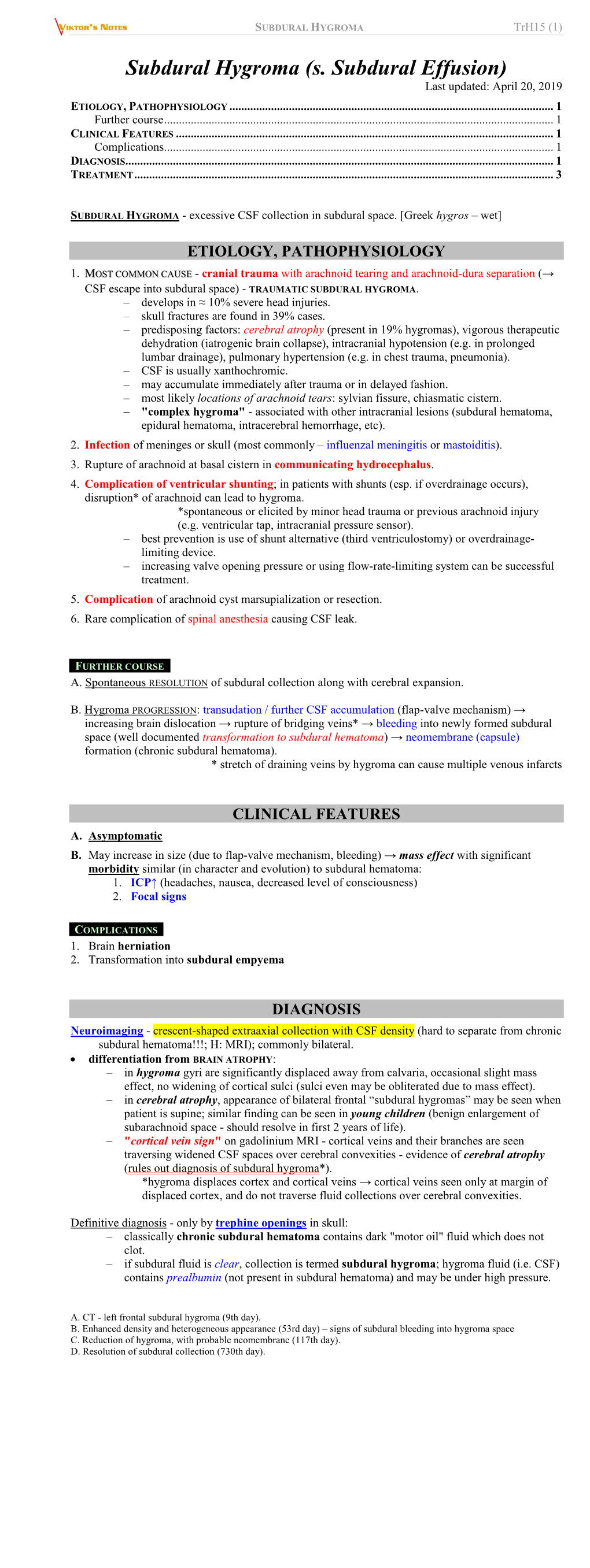
Trh15. Subdural Hygroma.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Positron Emission Tomography in Aging and Dementia: Effect of Cerebral Atrophy
CLINICAL SCIENCES Positron Emission Tomography in Aging and Dementia: Effect of Cerebral Atrophy John B. Chawluk, Abass Alavi, Robert Dann, Howard I. Hurtig, Sanjiv Bais, Michael J. Kushner, Robert A. Zimmerman, and Martin Reivich Department of Neurology, Cerebrovascular Research Center, and Department of Radiology. Hospital of the University of Pennsylvania, Philadelphia, Pennsylvania The spatial resolution of current positron emission tomography (PET) scanners does not allow a distinction between cerebrospinal fluid (CSF) containing spaces and contiguous brain tissue. Data analysis strategies which therefore purport to quantify cerebral metabolism per unit mass brain tissue are in fact measuring a value which may be artifactually reduced due to contamination by CSF. We studied cerebral glucose metabolism (CMRglc) in 17 healthy elderly individuals and 24 patients with Alzheimer's dementia using [18F]fluorodeoxyglucose and PET. All subjects underwent x-ray computed tomography (XCT) scanning at the time of their PET study. The XCT scans were analyzed volumetrically, in order to determine relative areas for ventricles, sulci, and brain tissue. Global CMRglc was calculated before and after correction for contamination by CSF (cerebral atrophy). A greater increase in global CMRglc after atrophy correction was seen in demented individuals compared with elderly controls (16.9% versus 9.0%, p < 0.0005). Additional preliminary data suggest that volumetric analysis of proton-NMR images may prove superior to analysis of XCT data in quantifying the degree of atrophy. Appropriate corrections for atrophy should be employed if current PET scanners are to accurately measure actual brain tissue metabolism in various pathologic states. J NucÃMed 28:431-^137,1987 he pioneering nitrous oxide technique of Kety and inability to measure glucose or oxygen metabolism Schmidt first enabled investigators to measure global directly. -

Clinical and MRI Clues and Pitfalls in the Diagnosis and Differential Diagnosis of Multiple Sclerosis
Clinical and MRI clues and pitfalls in the diagnosis and differential diagnosis of Multiple Sclerosis Aksel Siva, M.D. MS Clinic & Department Of Neurology Istanbul University Cerrahpaşa School of Medicine [email protected] MSParis2017 - 7th Joint ECTRIMS - ACTRIMS Meeting, 25 - 28 October 2017 Disclosure • Received research grants to my department from The Scientific and Technological Research Council Of Turkey - Health Sciences Research Grants numbers : 109S070 and 112S052.; and also unrestricted research grants from Merck-Serono and Novartis to our Clinical Neuroimmunology Unit • Honoraria or consultation fees and/or travel and registration coverage for attending several national or international congresses or symposia, from Merck Serono, Biogen Idec/Gen Pharma of Turkey, Novartis, Genzyme, Roche and Teva. • Educational presentations at programmes & symposia prepared by Excemed internationally and at national meetings and symposia sponsored by Bayer- Schering AG; Merck-Serono;. Novartis, Genzyme and Teva-Turkey; Biogen Idec/Gen Pharma of Turkey Introduction… • The incidence and prevalence rates of MS are increasing, so are the number of misdiagnosed cases as MS! • One major source of misdiagnosis is misinterpretation of nonspecific clinical and imaging findings and misapplication of MRI diagnostic criteria resulting in an overdiagnosis of MS! • The differential diagnosis of MS includes the MS spectrum and related disorders that covers subclinical & clinical MS phenotypes, MS variants and inflammatory astrocytopathies, as well as other Ab-associated atypical inflammatory-demyelinating syndromes • There are a number of systemic diseases in which either the clinical or MRI findings or both may mimic MS, which further cause confusion! Related publication *Siva A. Common Clinical and Imaging Conditions Misdiagnosed as Multiple Sclerosis. -

Inflammation, Demyelination, and Degeneration
Biochimica et Biophysica Acta 1812 (2011) 275–282 Contents lists available at ScienceDirect Biochimica et Biophysica Acta journal homepage: www.elsevier.com/locate/bbadis Review Inflammation, demyelination, and degeneration — Recent insights from MS pathology Christine Stadelmann ⁎, Christiane Wegner, Wolfgang Brück Institute of Neuropathology, University Medical Centre, Göttingen, Germany article info abstract Article history: Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system which responds to Received 15 March 2010 anti-inflammatory treatments in the early disease phase. However, the pathogenesis of the progressive Received in revised form 30 June 2010 disease phase is less well understood, and inflammatory as well as neurodegenerative mechanisms of tissue Accepted 6 July 2010 damage are currently being discussed. This review summarizes current knowledge on the interrelation Available online 15 July 2010 between inflammation, demyelination, and neurodegeneration derived from the study of human autopsy and biopsy brain tissue and experimental models of MS. Keywords: Multiple sclerosis © 2010 Elsevier B.V. All rights reserved. Pathogenesis Pathology Neuroaxonal damage Autoimmunity Progressive disease 1. Introduction in MS is necessarily the myelin sheath or oligodendrocyte [4].This review summarizes current knowledge and recent advances in MS Multiple sclerosis (MS) is an inflammatory demyelinating CNS immunopathology. disease frequently starting in young adulthood. Supported by experimental evidence mainly derived from its principal model, 2. Inflammation and demyelination experimental allergic encephalomyelitis (EAE), MS is generally considered a predominantly T cell-mediated autoimmune disease MS lesions can arise anywhere in the CNS. However, they show a [1]. In line with this notion, immunomodulatory and anti-inflamma- predilection for the optic nerve, spinal cord, brain stem, and tory therapies prove to be effective, especially early in the disease periventricular areas. -

And Cerebral Atrophy in Senile Dementia
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.8.751 on 1 August 1976. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1976, 39, 751-755 Correlation between diffuse EEG abnormalities and cerebral atrophy in senile dementia DUSAN STEFOSKI, DONNA BERGEN, JACOB FOX, FRANK MORRELL, MICHAEL HUCKMAN, AND RUTH RAMSEY From the Department ofNeurological Sciences and Department ofDiagnostic Radiology, Rush-Presbyterian-St. Luke's Medical Center, Chicago, Illinois, USA SYNOPSIS Thirty-five elderly patients were investigated because of clinical signs of dementia. The presence of diffuse cerebral atrophy, and its severity, were determined by the use of computed tomog- raphy (CT scan). All of the patients were also examined by electroencephalography (EEG), and the presence of diffuse abnormalities, especially diffuse slowing, was noted. Specifically, patients with normal or near-normal EEGs were compared with those with severe diffuse slowing. No correlation guest. Protected by copyright. between the presence or severity of diffuse EEG abnormalities and the degree of cerebral atrophy as measured by CT scan was found. Though the EEG is clearly identifying physiological dysfunction of nerve cells in demented patients it does not appear to be a reliable tool for the prediction of diffuse cerebral atrophy in this population. Senile dementia in association with diffuse defined as the gradual onset of intellectual deteriora- cerebral atrophy is one of the problems com- tion after the age of 59 years. Those patients with a monly encountered by the clinical neurologist. In past history of strokes or major focal findings on the numerous studies the EEG of demented indi- neurological examination were excluded. -

Stroke Subtype, Vascular Risk Factors, and Total MRI Brain Small-Vessel Disease Burden
ARTICLES Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden Julie Staals, MD, PhD ABSTRACT Stephen D.J. Makin, Objectives: In this cross-sectional study, we tested the construct validity of a “total SVD score,” MBChB which combines individual MRI features of small-vessel disease (SVD) in one measure, by testing Fergus N. Doubal, associations with vascular risk factors and stroke subtype. MBChB, PhD Methods: We analyzed data from patients with lacunar or nondisabling cortical stroke from 2 pro- Martin S. Dennis, spective stroke studies. Brain MRI was rated for the presence of lacunes, white matter hyperin- MBChB, MD, FRCP tensities, cerebral microbleeds, and perivascular spaces independently. The presence of each Joanna M. Wardlaw, SVD feature was summed in an ordinal “SVD score” (range 0–4). We tested associations with MBChB, MD, FRCR vascular risk factors, stroke subtype, and cerebral atrophy using ordinal regression analysis. Results: In 461 patients, multivariable analysis found that age (odds ratio [OR] 1.10, 95% confi- Correspondence to dence interval [CI] 1.08–1.12), male sex (OR 1.58, 95% CI 1.10–2.29), hypertension (OR 1.50, Dr. Wardlaw: 95% CI 1.02–2.20), smoking (OR 2.81, 95% CI 1.59–3.63), and lacunar stroke subtype (OR [email protected] 2.45, 95% CI 1.70–3.54) were significantly and independently associated with the total SVD score. The score was not associated with cerebral atrophy. Conclusions: The total SVD score may provide a more complete estimate of the full impact of SVD on the brain, in a simple and pragmatic way. -

Intracranial Hypotension
Romanian Neurosurgery (2011) XVIII 3: 279 – 285 279 Intracranial hypotension Şt.M. Iencean Neurosurgery, Emergency Clinical Hospital “Prof. Dr. N. Oblu” Iaşi, Romania Abstract the case of chronic subdural hematomas). The intracranial hypotension is the The decrease in the volume of the decrease in the intracranial pressure caused cerebral parenchyma, by various by the decrease in the volume of the mechanisms – senile cerebral atrophy, cerebrospinal fluid secondary to the CSF surgical resection, etc., does not generate loss. The intracranial hypotension is first of all an intracranial hypotension characterized by an orthostatic cephalea, not syndrome, but there may be focal calmed by antalgics accompanied by nausea, neurological symptoms depending on the vomiting, vertigos, diplopia, etc. The suffering cerebral areas. The volume of the diagnosis is confirmed by a lumbar diminished cerebral parenchyma is manometry and by the performed progressively diminished by gliosis and/or paraclinical explorations (cerebral CT, by CSF; therefore, the intracranial pressure cerebral MRI). is maintained at normal values. The The intracranial hypotension treatment decrease in the intracranial sanguine is - etiologic, and it consists in closing the volume by arterial hypotension leads to the CSF fistula; pathogenic, which consists in decrease in the cerebral perfusion pressure recreating the normal CSF volume, and with ischemic phenomena; this may also symptomatic, which refers to the treatment lead to a decreased CSF secretion, but the of the symptoms related to intracranial intracranial pressure decrease seems to be hypotension. less important than ischemia. The surgical Keywords: cerebrospinal fluid, CSF removal of a pathologic volume produces a fistula, intracranial hypotension, intracranial sudden decrease in the endocranial volume pressure and in the intracranial pressure, also known as the surgical cerebral-ventricular collapse, Introduction and which is rapidly compensated from a therapeutic point of view. -

LETTERS Potassium of 3.4 Mmol/L
820 J Neurol Neurosurg Psychiatry 2003;74:820–826 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.6.823 on 1 June 2003. Downloaded from sodium concentration of 136 mmol/l and The two patients presented here showed LETTERS potassium of 3.4 mmol/l. The serum phos- aclose temporal association between severe phate concentration was profoundly low at hypophosphataemia and the development of 0.13 mmol/l. T2 weighted and FLAIR se- CPM. Both patients abused alcohol, and the Central pontine myelinolysis quence MRI done three days after admission first patient had moderate hyponatraemia temporally related to showed abnormal signal within the central with hypokalaemia. They may therefore have brain stem suggestive of CPM (fig 1). hypophosphataemia been particularly susceptible to CPM for a She was treated with oral thiamine, multi- variety of reasons. It is possible, however, that Central pontine myelinolysis (CPM) is known vitamins, and minerals including phosphate. severe hypophosphataemia adversely affected to be associated with the rapid correction of She made a rapid improvement such that her the Na+/K+-ATPase pump and finally trig- severe hyponatraemia. However, there have dysarthria had resolved and gait improved gered apoptosis and CPM. The temporal been case reports of CPM occurring in sufficiently for her to be discharged 11 days association of neurological deterioration with 1 after admission. normonatraemic patients. Here we describe the rapid correction of profound hypophos- two patients in whom chronic alcohol abuse Comment phataemia in case 1 is unlikely to relate to led to profound hypophosphataemia that was The pathophysiology of CPM is not well osmotic stress in view of the small contribu- closely temporally related to the development understood. -

Epileptic Seizures Caused by Encephalomalasic Cysts Following Radiotherapy: a Case Report Fatih Serhat Erol and Bekir Akgun*
Open Access Case report Epileptic seizures caused by encephalomalasic cysts following radiotherapy: a case report Fatih Serhat Erol and Bekir Akgun* Address: Department of Neurosurgery, Firat Universitesi, Tip Fakultesi, Firat Tip Merkezi, Beyin Cerrahi Klinigi, 23200, Elazig, Turkey Email: FSE - [email protected]; BA* - [email protected] * Corresponding author Received: 2 July 2008 Accepted: 2 April 2009 Published: 16 July 2009 Cases Journal 2009, 2:7026 doi: 10.4076/1757-1626-2-7026 This article is available from: http://casesjournal.com/casesjournal/article/view/7026 © 2009 Erol and Akgun; licensee Cases Network Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Introduction: Cerebral radionecrosis is a delayed and rarely observed complication of radio- therapy. Cerebral radionecrosis may occur as cystic encephalomalasic formations which cover the intracranial region. These cysts may, in rare cases, become quite large. They may cause drug-resistant seizures, neurological deficits and consciousness disorders. Case presentation: A 55-year-old, Turkish female patient was admitted to hospital with seizure, consciousness disorder and weakness in the right side of her body. The patient had history of an operation in the left maxillary area due to basal cell carcinoma 7 years previously and then history of radiotherapy due to relapse 2 years later the operation. The patient had large cystic encephalomalasic lesions. Despite steroid and dual antiepileptic treatments, the patient’s complaints had significantly worsened and seizures continued. -

CSF Dynamics for Shunt Prognostication and Revision in Normal Pressure Hydrocephalus
Journal of Clinical Medicine Review CSF Dynamics for Shunt Prognostication and Revision in Normal Pressure Hydrocephalus Afroditi Despina Lalou 1,*, Marek Czosnyka 1,2 , Michal M. Placek 1 , Peter Smielewski 1, Eva Nabbanja 1 and Zofia Czosnyka 1 1 Brain Physics Laboratory, Division of Neurosurgery, Department of Clinical Neurosciences, University of Cambridge, Cambridge CB2 0QQ, UK; [email protected] (M.C.); [email protected] (M.M.P.); [email protected] (P.S.); [email protected] (E.N.); [email protected] (Z.C.) 2 Institute of Electronic Systems, Faculty of Electronics and Information Sciences, Warsaw University of Technology, 00-661 Warsaw, Poland * Correspondence: [email protected]; Tel.: +44-774-3567-585 Abstract: Background: Despite the quantitative information derived from testing of the CSF circula- tion, there is still no consensus on what the best approach could be in defining criteria for shunting and predicting response to CSF diversion in normal pressure hydrocephalus (NPH). Objective: We aimed to review the lessons learned from assessment of CSF dynamics in our center and summarize our findings to date. We have focused on reporting the objective perspective of CSF dynamics testing, without further inferences to individual patient management. Discussion: No single parameter from the CSF infusion study has so far been able to serve as an unquestionable outcome predictor. Resistance to CSF outflow (Rout) is an important biological marker of CSF circulation. It should not, however, be used as a single predictor for improvement after shunting. Testing of CSF dynamics Citation: Lalou, A.D.; Czosnyka, M.; Placek, M.M.; Smielewski, P.; provides information on hydrodynamic properties of the cerebrospinal compartment: the system Nabbanja, E.; Czosnyka, Z. -

Characteristic Diagnostic Imaging Findings in Alzheimer's Disease
Ⅵ Alzheimer’s Disease Characteristic Diagnostic Imaging Findings in Alzheimer’s Disease JMAJ 46(6): 269–276, 2003 Shin KITAMURA Assistant Professor, Department of Internal Medicine, Nippon Medical School Second Hospital Abstract: There are characteristic neuroimaging findings in Alzheimer’s disease. X-ray computed tomography (CT) and magnetic resonance imaging (MRI) reveal cerebral atrophy. The atrophy is recognized in the frontal, temporal, and parietal lobes, but not in the occipital lobe. Dilation of the inferior horn, which reflects the atrophy of the medial temporal cortex, is a characteristic finding in Alzheimer’s disease, but, cerebral atrophy is a nonspecific finding. MRI is superior as method of detecting atrophy of the hippocampus. Estimation of hippocampal volume is useful for differentiation between Alzheimer’s disease and a normal brain but it is not practical because the method is complicated. Single-photon emission computed tomography (SPECT) and positron emission tomography (PET) reveal reduced blood flow and metabolism in the temporal and the parietal cortex. Reduced blood flow and metabolism in the posterior cingulate cortex are detected by analysis using three-dimensional stereotactic surface projections. These find- ings are also recognized in the early stage of Alzheimer’s disease. Since functional changes in the brain, namely reduction of cerebral blood flow and metabolism, precede the morphological changes, SPECT and PET are more useful for the early diagnosis of Alzheimer’s disease than CT and MRI. Key words: Alzheimer’s disease; Cerebral blood flow; SPECT; MRI Introduction important to make a definitive diagnosis of Alzheimer’s disease. In clinical practice, the Almost three years have passed since thera- diagnosis as Alzheimer’s disease may be made peutic drugs for the treatment of Alzheimer’s based on the clinical course of dementia, the disease were approved in Japan. -

Diagnostic and Therapeutic Aspects of Hemiplegic Migraine
Migraine J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2020-322850 on 19 May 2020. Downloaded from REVIEW Diagnostic and therapeutic aspects of hemiplegic migraine Vincenzo Di Stefano ,1 Marianna Gabriella Rispoli,2 Noemi Pellegrino,3 Alessandro Graziosi,3 Eleonora Rotondo,3 Christian Napoli,4 Daniela Pietrobon,5,6 Filippo Brighina,1 Pasquale Parisi 7 For numbered affiliations see ABSTRact hypothesised a role for gene PRRT2 in migraine end of article. Hemiplegic migraine (HM) is a clinically and genetically pathophysiology, but its specific implication in heterogeneous condition with attacks of headache HM is still debated. Given the lack of a recognised Correspondence to and motor weakness which may be associated with fourth autosomal dominant gene for FHM, other Professor Pasquale Parisi, Dipartimento di Neuroscienze impaired consciousness, cerebellar ataxia and intellectual genetic mechanisms might be supposed and further 2 Salute Mentale e Organi di disability. Motor symptoms usually last <72 hours and genetic analyses are needed. Sporadic hemiplegic Senso (NESMOS), University of are associated with visual or sensory manifestations, migraine (SHM) shares similar clinical character- Rome La Sapienza Faculty of speech impairment or brainstem aura. HM can occur istics with FHM but it differs for the absence of Medicine and Psychology, Roma family history for HM.6 00189, Lazio, Italy; pasquale. as a sporadic HM or familiar HM with an autosomal parisi@ uniroma1. it dominant mode of inheritance. Mutations in CACNA1A, As HM is a rare condition, few studies are ATP1A2 and SCN1A encoding proteins involved in ion reported and there are no specific treatments. In Received 21 January 2020 transport are implicated. -

Hippocampal and Prefrontal Atrophy in Patients with Early Non-Demented
1467 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2003.031237 on 16 September 2004. Downloaded from SHORT REPORT Hippocampal and prefrontal atrophy in patients with early non-demented Parkinson’s disease is related to cognitive impairment A Bru¨ck, T Kurki, V Kaasinen, T Vahlberg, J O Rinne ............................................................................................................................... J Neurol Neurosurg Psychiatry 2004;75:1467–1469. doi: 10.1136/jnnp.2003.031237 there was prefrontal atrophy it would be related to impair- Background: Early stage patients with Parkinson’s disease ment in tests requiring frontal lobe functions. (PD) show cognitive impairment in frontal lobe functions and memory tests. Hippocampal atrophy is seen in medicated patients with advanced PD. SUBJECTS AND METHODS Objectives: To examine whether prefrontal or hippocampal The patient sample consisted of 20 non-demented patients (seven women and 13 men) with idiopathic PD at an early atrophy are already present in early stage PD, and whether stage of the disease. The patients were diagnosed at the such atrophy is associated with cognitive impairment. department of neurology, University of Turku and had at Methods: Twenty non-medicated, non-demented patients least two of the main symptoms of PD: tremor, rigidity, and with early stage PD and 22 neurologically healthy age hypokinesia. None of the patients exhibited atypical symp- matched controls were studied. All subjects underwent toms.8 All patients fulfilled the UK Parkinson’s disease brain magnetic resonance imaging to study hippocampal and bank criteria for definite PD. None of the patients had prefrontal atrophy. Atrophy was evaluated by a neuro- received antiparkinsonian medication before the examina- radiologist using a five point scale.