Acne Fulminans
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Azelaic Acid
Azelaic Acid (FINACEA) Topical Foam 15% National Drug Monograph August 2016 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Azelaic acid is a naturally occurring C9-dicarboxylic acid that is found in plants Action (such as whole grain cereals), animals and humans. Azelaic acid has antiinflammatory, antioxidative and antikeratinizing effects. In rosacea skin, azelaic acid decreases cathelicidin levels and kallikrein 5 (KLK5) activity and possibly inhibits toll-like receptor 2 (TLR2) expression.1 A 15% gel formulation has been marketed for rosacea, and 20% cream has been available for acne vulgaris. The newer foam formulation consists of an oil- in-water emulsion and was designed to have a higher lipid content than the gel for dry and sensitive skin. Indication(s) Under Review Topical treatment of inflammatory papules and pustules of mild to moderate in This Document rosacea. Dosage Form(s) Under Foam, 15% Review REMS REMS No REMS Postmarketing Requirements See Other Considerations for additional REMS information Pregnancy Rating Category B Executive Summary Efficacy There have been no head-to-head trials comparing the foam and gel formulations of azelaic acid in terms of safety, tolerability and efficacy in the treatment of papulopustular (PP) rosacea.. In two major randomized clinical trials, azelaic acid foam produced small benefits over vehicle foam in achieving Investigator’s Global Assessment (IGA) treatment success (NNTs of 9.2 and 11.5) and in reducing inflammatory lesion counts. -

Targeted Topical Delivery of Retinoids in the Management of Acne Vulgaris: Current Formulations and Novel Delivery Systems
pharmaceutics Review Targeted Topical Delivery of Retinoids in the Management of Acne Vulgaris: Current Formulations and Novel Delivery Systems Gemma Latter 1, Jeffrey E. Grice 2, Yousuf Mohammed 2 , Michael S. Roberts 2,3 and Heather A. E. Benson 1,* 1 School of Pharmacy and Biomedical Sciences, Curtin Health Innovation Research Institute, Curtin University, Perth 6845, Australia; [email protected] 2 Therapeutics Research Group, The University of Queensland Diamantina Institute, School of Medicine, University of Queensland, Translational Research Institute, Brisbane 4109, Australia; jeff[email protected] (J.E.G.); [email protected] (Y.M.); [email protected] (M.S.R.) 3 School of Pharmacy and Medical Sciences, University of South Australia, Basil Hetzel Institute for Translational Health Research, Adelaide 5011, Australia * Correspondence: [email protected]; Tel.: +61-8-9266-2338 Received: 19 August 2019; Accepted: 17 September 2019; Published: 24 September 2019 Abstract: Acne vulgaris is a common inflammatory pilosebaceous condition that affects 80–90% of adolescents. Since the introduction of tretinoin over 40 years ago, topical retinoid products have been a mainstay of acne treatment. The retinoids are very effective in addressing multiple aspects of the acne pathology as they are comedolytic and anti-inflammatory, and do not contribute to antibiotic resistance or microbiome disturbance that can be associated with long-term antibiotic therapies that are a common alternative treatment. However, topical retinoids are associated with skin dryness, erythema and pain, and may exacerbate dermatitis or eczema. Thus, there is a clear need to target delivery of the retinoids to the pilosebaceous units to increase efficacy and minimise side effects in surrounding skin tissue. -

Skin - Sulfa*Derm Sulfaderm Or Sulfa*Derm - Helps Promote Healthy Skin Function
Skin - Sulfa*Derm Sulfaderm or Sulfa*Derm - Helps promote Healthy skin Function. Has been shown to help clear up most Acne in 24 hours, Bacterial infections, Rashes, Bed Sores, Dermatitis, Eczema, Fungus/Yeast, Psoriasis type problems, Ring Worm and Wounds that won't heal. HISTORY OF SULFUR Harnessing the power of volcanos, our cutting edge formula is considered a breakthrough for the treatment of acne. Sulfa*Derm has been shown to clear up acne in one day. The active ingredient sulfur from volcanic ash destroys bacteria quickly. The Zinc Oxide combats rashes. Tea Tree Oil is a well known antiseptic and anti-fungal, while the Aloe Vera re-nourishes the skin. Vitamin E is used as the base instead of oils that clog up the skin. Sulfa*Derm is probably the best acne and everything else cream that has ever been made. When treating skin problems it is recommended to detoxify your liver. Sulfur is a yellow mineral that quite often occurs in nature in powder form. It can, under pressure bond to water, as in mineral springs or mix into the earth, as in mud baths. Normally sulfur is expunged from under the ground through the craters of venting volcanoes, where it is spread around in chunky blocks. Sulfur has been around for a long time. Native Polynesians claim to have cured a variety of infections in their hot sulfur mineral springs. Russian mud treatments, high in sulfur, have been used for centuries as a reputed therapy for arthritis. California's Napa Valley, specifically the city called Sulfur Springs, was the health spa for the wealthy until the early 1900's. -

Outpatient Acne Care Guideline
Outpatient Acne Care Guideline Severity Mild Moderate Severe < 20 comedones or < 20-100 comedones or 15-50 > 5 cysts, >100 comedones, or inflammatory lesions inflammatory lesions >50 inflammatory lesions Initial Treatment Initial Treatment Initial Treatment Benzoyl Peroxide (BP) or Topical Combination Therapy Combination Therapy Topical Retinoid Retinoid + BP Oral antibiotic or OR + (Retinoid + Antibiotic) + BP Topical retinoid Topical Combination Therapy or + BP + Antibiotic Retinoid + (BP + Antibiotic) or OR BP Retinoid + BP Oral antibiotic + topical retinoid + +/- or BP Topical antibiotic Retinoid + Antibiotic + BP or Topical Dapsone IF Inadequate Response IF Inadequate Response IF Inadequate Consider dermatology Response referral Change topical retinoid Consider changing oral concentrations, type and/or antibiotic formulation AND or Add BP or retinoid, if not already Change topiocal combination Consider isotretinoin prescribed therapy Consider hormone therapy or and/or (females) Change topical retinoid Add or change oral antibiotic concentrations, type and/or or formulation Consider isotretinoin Additional Considerations or Consider hormone therapy (females) Change topical comination Previous treatment/history Side effects therapy Costs Psychosocial impact Vehicle selection Active scarring Ease of use Regimen complexity Approved Evidence Based Medicine Committee 1-18-17 Reassess the appropriateness of Care Guidelines as condition changes. This guideline is a tool to aid clinical decision making. It is not a standard of care. The physician should deviate from the guideline when clinical judgment so indicates. GOAL: Pediatricians should initiate treatment for cases of “Mild” to “Severe” acne (see algorithms attached). Pediatricians should also counsel patients in order to maximize adherence to acne treatment regimens: 1. Realistic expectations. Patients should be counseled that topical therapies typically take up to 6-8 weeks to start seeing results. -
Enhanced Catalytic Ozonation of Ibuprofen Using a 3D Structured
www.nature.com/scientificreports OPEN Enhanced catalytic ozonation of ibuprofen using a 3D structured catalyst with MnO2 nanosheets on carbon microfbers Guhankumar Ponnusamy1, Hajar Farzaneh2, Yongfeng Tong1, Jenny Lawler1, Zhaoyang Liu1* & Jayaprakash Saththasivam1* Heterogeneous catalytic ozonation is an efective approach to degrade refractory organic pollutants in water. However, ozonation catalysts with combined merits of high activity, good reusability and low cost for practical industrial applications are still rare. This study aims to develop an efcient, stable and economic ozonation catalyst for the degradation of Ibuprofen, a pharmaceutical compound frequently detected as a refractory pollutant in treated wastewaters. The novel three-dimensional network-structured catalyst, comprising of δ-MnO2 nanosheets grown on woven carbon microfbers (MnO2 nanosheets/carbon microfber), was synthesized via a facile hydrothermal approach. Catalytic ozonation performance of Ibuprofen removal in water using the new catalyst proves a signifcant enhancement, where Ibuprofen removal efciency of close to 90% was achieved with a catalyst loading of 1% (w/v). In contrast, conventional ozonation was only able to achieve 65% removal efciency under the same operating condition. The enhanced performance with the new catalyst could be attributed to its signifcantly increased available surface active sites and improved mass transfer of reaction media, as a result of the special surface and structure properties of this new three- dimensional network-structured catalyst. Moreover, the new catalyst displays excellent stability and reusability for ibuprofen degradation over successive reaction cycles. The facile synthesis method and low-cost materials render the new catalyst high potential for industrial scaling up. With the combined advantages of high efciency, high stability, and low cost, this study sheds new light for industrial applications of ozonation catalysts. -

Moisturizer Use Enhances Facial Tolerability of Tazarotene 0.1% Cream Without Compromising Efficacy in Patients with Acne
Poster 101 Moisturizer Use Enhances Facial Tolerability of Tazarotene 0.1% Cream Without Compromising Efficacy in Patients With Acne Vulgaris Emil Tanghetti,1 Zoe Draelos,2 Pearl Grimes,3 Sunil Dhawan,4 Michael Gold,5 Leon Kircik,6 Lawrence Green,7 Angela Moore,8 Fran Cook-Bolden9 1Center for Dermatology and Laser Surgery, Sacramento, CA; 2Dermatology Consulting Services, High Point, NC; 3Vitiligo & Pigmentation Institute of Southern California, Los Angeles, CA; 4Center for Dermatology, Cosmetic and Laser Surgery, Fremont, CA; 5Tennessee Clinical Research Center, Nashville, TN; 6Physicians Skin Care PLLC, Louisville, KY; 7The George Washington University, Washington, DC; 8Arlington Center for Dermatology, Arlington, TX; 9The Skin Specialty Group, New York, NY • 6 months for systemic retinoids Table 1. Scale used to assess overall disease severity. • Mean levels of compliance were between “mostly compliant” and Efficacy Tolerability INTRODUCTION “very compliant” in both groups throughout the study. There were Score Overall disease severity no significant between-group differences in the degree of • The reduction in lesion counts with tazarotene + moisturizer was at • No adverse events considered probably or definitely related to treatment The use of any topical retinoid can involve a period of “retinization” in the first Treatment regimen 0 None—clear, no inflammatory lesions compliance. least as great as that with tazarotene alone at week 16: were reported. few weeks of treatment while the skin is adapting to the retinoid. During this • Patients were randomly assigned (on a 1:2 basis) to one of the following 1 Sparse comedones, with very few or no inflammatory lesions present period of acclimatization, some patients transiently experience dryness, – 57% vs. -
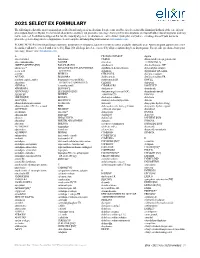
2021 SELECT EX FORMULARY the Following Is a List of the Most Commonly Prescribed Brand and Generic Medications
2021 SELECT EX FORMULARY The following is a list of the most commonly prescribed brand and generic medications. It represents an abbreviated version of the formulary list that is at the core of your prescription drug benefit plan. The list is not all-inclusive and does not guarantee coverage. Some preferred medications overlap with other clinical programs and may not be covered. In addition to drugs on this list, the majority of generic medications are covered under your plan and you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. Search complete formulary drug information at elixirsolutions.com. PLEASE NOTE: Preferred brand drugs may move to non-preferred status if a generic version becomes available during the year. Any medication approved to enter the market will not be covered until reviewed by Elixir. Not all drugs listed are covered by all prescription drug benefit programs. For specific questions about your coverage, please visit elixirsolutions.com. A B CILOXAN OINTMENT digoxin abacavir tablet balsalazide CIMDUO diltiazem ER (except generics for abacavir-lamivudine BAQSIMI cinacalcet CARDIZEM LA) ABILIFY MAINTENA [INJ] BASAGLAR [INJ] ciprofloxacin dimethyl fumarate DR* abiraterone* BD ULTRAFINE INSULIN SYRINGES ciprofloxacin-dexamethasone diphenoxylate-atropine acetic acid & NEEDLES citalopram dipyridamole ER-aspirin acitretin BELBUCA CITRANATAL divalproex sodium ACUVAIL BELSOMRA clarithromycin divalproex sodium ER acyclovir capsule, tablet benzonatate (except NDCs: clarithromycin ER DIVIGEL -
DF Fall 2019-Webready
A DERMATOLOGY FOUNDATION PUBLICATION SPONSORED BY ORTHO DERMATOLOGICS VOL. 38 NO. 2 FALL 2019 DDEERRMMAATTOOLLOOGGYY ™ Also In This Issue FOCUSFOCUS Janet Fairley, MD, New DF President: “DF support has profoundly advanced our specialty.” DF Clinical Symposia: Stiefel Scholar Cancer Research— Proceedings 2019–Part II Aiming to Normalize KC Cells Explaining that the child’s skin barrier has a structural defect enables ADVANCES IN DERMATOLOGY parents to understand the involvement of inadequate hydration, more bacteria, and increased penetration of antigens and allergens. Then The Dermatology Foundation presented its Maguiness explains the need to simultaneously treat the dehydrated annual 3-day cutting-edge CME symposia series skin, itch, inflammation, and infection, and teaches parents the entire earlier this year. Informal Breakfast Roundtables 2-week topical “eczema boot camp” routine: bleach baths, topical and evening Therapeutics Forums amplified the steroids, emollients, and wet wraps, typically done at home. She reassuringly likens a bleach bath to a swimming pool. Maguiness take-home value. Part II of the Proceedings includes described the procedures and benefits of bleach baths and wet wraps Therapeutic Updates; Diagnostic Dilemmas; and in detail, provided practical tips for gaining parental confidence and Medical Dermatology. (Part I, which appeared understanding, noted variations to the overall “boot camp” routine, and in the previous issue, included the Keynote talk discussed tapering. Then she shared her excitement about “entering -

Precipitated Sulfur: Summary Report
Precipitated Sulfur: Summary Report Item Type Report Authors Yuen, Melissa V.; Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Mattingly, Ashlee N. Publication Date 2020-02 Keywords Precipitated sulfur; Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration Rights Attribution-NoDerivatives 4.0 International Download date 02/10/2021 22:32:18 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12274 Summary Report Precipitated Sulfur Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy February 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATIONS ................................................................................................... 4 METHODOLOGY ................................................................................................................... -

CVS Formulary Drug Listing
January 2021 Updated 11/01/2020 Performance Drug List - Standard Control The CVS Caremark® Performance Drug List - Standard Control is a guide within select therapeutic categories for clients, plan members and health care providers. Generics should be considered the first line of prescribing. If there is no generic available, there may be more than one brand-name medicine to treat a condition. These preferred brand-name medicines are listed to help identify products that are clinically appropriate and cost-effective. Generics listed in therapeutic categories are for representational purposes only. This is not an all-inclusive list. This list represents brand products in CAPS, branded generics in upper- and lowercase Italics, and generic products in lowercase italics. PLAN MEMBER HEALTH CARE PROVIDER Your benefit plan provides you with a prescription benefit program Your patient is covered under a prescription benefit plan administered administered by CVS Caremark. Ask your doctor to consider by CVS Caremark. As a way to help manage health care costs, prescribing, when medically appropriate, a preferred medicine from authorize generic substitution whenever possible. If you believe a this list. Take this list along when you or a covered family member brand-name product is necessary, consider prescribing a brand name sees a doctor. on this list. Please note: Please note: • Your specific prescription benefit plan design may not cover • Generics should be considered the first line of prescribing. certain products or categories, regardless of their appearance in • The member's prescription benefit plan design may alter coverage this document. Products recently approved by the U.S. Food and of certain products or vary copay1 amounts based on the condition Drug Administration (FDA) may not be covered upon release being treated. -

Disfiguring Ulcerative Neutrophilic Dermatosis Secondary To
RESIDENT HIGHLIGHTS IN COLLABORATION WITH COSMETIC SURGERY FORUM Disfiguring Ulcerative Neutrophilic Dermatosis Secondary to Doxycycline and Isotretinoin in an Bahman Sotoodian, MD Top 10 Fellow and Resident Adolescent Boy With Grant Winner at the 8th Cosmetic Surgery Forum Acne Conglobata Bahman Sotoodian, MD; Paul Kuzel, MD, FRCPC; Alain Brassard, MD, FRCPC; Loretta Fiorillo, MD, FRCPC copy accompanied by systemic symptoms including fever and leuko- RESIDENT cytosis. We report a challenging case of a 13-year-old adolescent PEARL boy who acutely developed hundreds of ulcerative plaques as well • Doxycycline and isotretinoin have been widely used as systemicnot symptoms after being treated with doxycycline and for treatment of inflammatory and nodulocystic acne. isotretinoin for acne conglobata. He was treated with prednisone, Although outstanding results can be achieved, para- dapsone, and colchicine and had to switch to cyclosporine to doxical worsening of acne while starting these medi- achieve relief from his condition. cations has been described. In patients with severeDo Cutis. 2017;100:E23-E26. acne (ie, acne conglobata), initiation of doxycycline and especially isotretinoin at regular dosages as the sole treatment can impose devastating risks on the patient. These patients are best treated with a combi- cne fulminans is an uncommon and debilitating nation of low-dose isotretinoin (at the beginning) with disease that presents as an acute eruption of nodular a moderate dose of steroids, which should be gradu- A and ulcerative acne lesions with associated systemic ally tapered while the isotretinoin dose is increased to symptoms.1,2 Although its underlying pathophysiology is 0.5 to 1 mg/kg once daily. -

Canadian Clinical Practice Guideline on the Management of Acne (Full Guideline)
Appendix 4 (as supplied by the authors): Canadian Clinical Practice Guideline on the Management of Acne (full guideline) Asai, Y 1, Baibergenova A 2, Dutil M 3, Humphrey S 4, Hull P 5, Lynde C 6, Poulin Y 7, Shear N 8, Tan J 9, Toole J 10, Zip C 11 1. Assistant Professor, Queens University, Kingston, Ontario 2. Private practice, Markham, Ontario 3. Assistant Professor, University of Toronto, Toronto, Ontario 4. Clinical Assistant Professor, University of British Columbia, Vancouver, British Columbia 5. Professor, Dalhousie University, Halifax, Nova Scotia 6. Associate Professor, University of Toronto, Toronto, Ontario 7. Associate Clinical Professor, Laval University, Laval, Quebec 8. Professor, University of Toronto, Toronto, Ontario 9. Adjunct Professor, University of Western Ontario, Windsor, Ontario 10. Professor, University of Manitoba, Winnipeg, Manitoba 11. Clinical Associate Professor, University of Calgary, Calgary, Alberta Appendix to: Asai Y, Baibergenova A, Dutil M, et al. Management of acne: Canadian clinical practice guideline. CMAJ 2015. DOI:10.1503/cmaj.140665. Copyright © 2016 The Author(s) or their employer(s). To receive this resource in an accessible format, please contact us at [email protected]. Contents List of Tables and Figures ............................................................................................................. v I. Introduction ................................................................................................................................ 1 I.1 Is a Clinical Practice Guideline