Geographical Variation in Use of Intensive Care in Denmark: a Nationwide Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Guide to the SKIVE AREA
TIPS FOR WALKING AND CYCLING TRIPS ADRENALINE KICKS AND MOMENTS NEW IN THE AREA? SAFE ENVIRONMENT OF PEACE Guide to the SKIVE AREA A HUB FOR GREEN ACTION PURE LIFE BECOME PART OF THE COMMUNITY SKIVE IN FIGURES EXPLORE THE AREA SKIVE MUNICIPALITY PAGE 03 Welcome to the PURE LIFE WELCOME TO THE SKIVE AREA The Skive Area is a special place to live. It lets you lead a greener life – both via its unique countryside and leading position in terms of climate-friendly solutions. Strong communities, good schools and an active business com- SKIVE munity are some of the elements that characterise the area. In the Skive Area you will find desirable residences and building sites which will form a basis for your everyday life here. The urban development project BigBlue Skive is priming Skive for a more climate-friendly future and uniting the city on both sides of the picturesque river. And finally, development projects AREA in the rural areas are creating a framework for new strong communities. No matter where you choose to live, you will always be close to nature with green woods, wide heathlands and THE LIMFJORD that is never more than 12 kilometres away, as the crow flies. The area is connected geographically by the surrounding fjord. And with a 199-kilometre stretch of coast (that is more than four metres for each resident) and six active harbours, the Skive Area provides ample opportunity for you to fulfil your dream of living by or close to the sea. �⟶ STRETCH OF COAST AREA 199 kilometres 684km2 With more than four metres of coast for each resident This results in a pop- and six active harbours, the area provides ample op- ulation density of 67 portunity for you to fulfil your dream of living by the sea. -

Growing Smart Cities in Denmark
GROWING SMART CITIES IN DENMARK DIGITAL TECHNOLOGY FOR URBAN IMPROVEMENT AND NATIONAL PROSPERITY RESEARCH AND EDITORIAL ABOUT TEAM About Invest in Denmark Léan Doody As part of the Ministry of Foreign Affairs of Denmark, Invest Associate Director – Arup in Denmark is a customized one-stop service for foreign [email protected] companies looking to set up a business in Denmark. Nicola Walt www.investindk.com Principal Consultant – Arup [email protected] About Arup Ina Dimireva Consultant – Arup Arup is an independent consultancy providing professional [email protected] services in management, planning, design and engineering. As a global firm Arup draws on the skills and expertise of Anders Nørskov Director – CEDI nearly 11,000 consultants. Arup’s dedication to exploring [email protected] innovative strategies and looking beyond the constraints of individual specialisms allows the firm to deliver holistic, multi-disciplinary solutions for clients. STEERING COMMITTEE www.arup.com This research was commissioned by: About CEDI CEDI is a consulting company with expertise in public sector digitization in Denmark. CEDI provides strategic consulting Financing partners and steering committee: to the government and the IT industry based on solid insight into the subjects of digitization and technology, extensive knowledge on the administrative and decision-making pro- cesses of government agencies, and a deep understanding of the political agenda. www.cedi.dk Additional participants in the steering committee meetings were the Central Denmark Region, Local Government Den- mark (LGDK) and the municipalities of Aarhus and Vejle. Layout Mads Toft Jensen +45 25143599 [email protected] www.spokespeople.dk ©2016 Arup, CEDI. -

VEST Uddannelse Job-1.Xlsx
Deltagerliste*VEST:*Uddannelse/Job*D*2.*Juni*2014 Anders'Ladegaard [email protected] UU'DANMARK Anders'Skov [email protected] UU'Aarhus'Samsø Anne?Me@e'Almind'Andersen anne?me@e@uu?lillebaelt.dk UU'Lillebælt Bente'Sønderup [email protected] Ungeenheden'Herning BeGna'Dichmann beGna@uu?lillebaelt.dk UU'Lillebælt Birgit'Petersen [email protected] UU'Odder'Skanderborg BJarne'Jeppesen bJarne@uu?lillebaelt.dk UU'Lillebælt Bri@'Bitsch [email protected]@svendborg.dk UU'Center'Sydfyn Charlo@e'Aalbæk'Hansen charlo@e@uu?lillebaelt.dk UU'Lillebælt Dorien'Hansen dorien@uu?lillebaelt.dk UU'Lillebælt Elin'Holst [email protected] UU'Aalborg Erik'Lykkegaard erik@uu?lillebaelt.dk UU'Lillebælt Eva'Geer [email protected] UU'Aarhus'Samsø Eva'Sherson [email protected] UU'Odder'Skanderborg Gurli'Nyborg'Mogensen gurli@uu?lillebaelt.dk UU'Lillebælt Hanne'Skov'ChrisPansen [email protected] UU'Center'Sydfyn Henrik'Michael'Nielsen [email protected] UU'Varde/Team'Ung'i'Uddannelse Henry'Hansen [email protected] UU'Skive Iben'Bak'Larsen [email protected] UU'Odder'Skanderborg Jens'Oluf'Bundgaard [email protected] UU'Aalborg Jens'Seifert'Baier'Andersen [email protected]'Randers Jens'Søndergaard'Nielsen [email protected] UU'Ringkøbing'FJord John'A.'Hansen [email protected] UU'Odder'Skanderborg Jørgen'Danielsen [email protected] UU'Odder'Skanderborg Jørgen'Krogh'Poulsen [email protected] UU?Herning Jørn'Tollef'Dresler [email protected] UU'Center'Sydfyn karen'dinesen -

Referral of Paediatric Patients Follows Geographic Borders of Administrative Units
Dan Med Bul ϧϪ/Ϩ June ϤϢϣϣ DANISH MEDICAL BULLETIN ϣ Referral of paediatric patients follows geographic borders of administrative units Poul-Erik Kofoed1, Erik Riiskjær2 & Jette Ammentorp3 ABSTRACT e ffect of economic incentives rooted in local govern- ORIGINAL ARTICLE INTRODUCTION: This observational study examines changes ment’s interest in maximizing the number of patients 1) Department in paediatric hospital-seeking behaviour at Kolding Hospital from their own county/region who are treated at the of Paediatrics, in The Region of Southern Denmark (RSD) following a major county/region’s hospitals in order not to have to pay the Kolding Hospital, change in administrative units in Denmark on 1 January higher price at hospitals in other regions or in the pri- 2) School of 2007. vate sector. Treatment at another administrative unit is Economics and MATERIAL AND METHODS: Data on the paediatric admis- Management, usually settled with 100% of the diagnosis-related group University of sions from 2004 to 2009 reported by department of paedi- (DRG) value, which is not the case for treatment per - Aarhus, and atrics and municipalities were drawn from the Danish formed at hospitals within the same administrative unit. 3) Health Services National Hospital Registration. Patient hospital-seeking On 1 January 2007, the 13 Danish counties were Research Unit, behaviour was related to changes in the political/admini s- merged into five regions. The public hospitals hereby Kolding Hospital/ trative units. Changes in number of admissions were com- Institute of Regional became organized in bigger administrative units, each pared with distances to the corresponding departments. Health Services with more hospitals than in the previous counties [7]. -

University of Copenhagen
Geographical Variation in Opioid Use in Elderly Patients with Dementia A Nationwide Study Jensen-Dahm, Christina; Zakarias, Johanne Købstrup; Gasse, Christiane; Waldemar, Gunhild Published in: Journal of Alzheimer's Disease DOI: 10.3233/JAD-190413 Publication date: 2019 Document version Publisher's PDF, also known as Version of record Document license: CC BY-NC Citation for published version (APA): Jensen-Dahm, C., Zakarias, J. K., Gasse, C., & Waldemar, G. (2019). Geographical Variation in Opioid Use in Elderly Patients with Dementia: A Nationwide Study. Journal of Alzheimer's Disease, 70(4), 1209-1216. https://doi.org/10.3233/JAD-190413 Download date: 01. Oct. 2021 Journal of Alzheimer’s Disease 70 (2019) 1209–1216 1209 DOI 10.3233/JAD-190413 IOS Press Geographical Variation in Opioid Use in Elderly Patients with Dementia: A Nationwide Study Christina Jensen-Dahma,∗, Johanne Købstrup Zakariasa, Christiane Gasseb,c and Gunhild Waldemara aDanish Dementia Research Centre, Department of Neurology, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark bDepression and Anxiety/Psychosis Research Unit, Aarhus University Hospital Psychiatry, Aarhus N, Denmark cNational Centre for Register Based Research, Aarhus University, Aarhus, Denmark Handling Associate Editor: Alba Malara Accepted 8 June 2019 Abstract. Background: We recently reported frequent use of opioids among elderly with dementia. Discrepancies in clinical practice may in part explain the higher use of opioids in elderly with dementia, which geographical variation may be able to clarify. Objective: To investigate geographical variation in opioid use in elderly with dementia compared to elderly without dementia. Methods: Register-based cross-sectional study in the entire elderly (≥65 years) population of Denmark in 2015. -
ADDRESSING the METROPOLITAN CHALLENGE in BARCELONA METROPOLITAN AREA Appendix
ADDRESSING THE METROPOLITAN CHALLENGE IN BARCELONA METROPOLITAN AREA Appendix. Case studies of five metropolitan areas: Amsterdam, Copenhagen, Greater Manchester, Stuttgart and Zürich Case Studies of Five Metropolitan Areas: Amsterdam, Copenhagen, Greater Manchester, Stuttgart and Zürich is part of the study Addressing Metropolitan Challenges in Barcelona Metropolitan Area, which was drafted by the Metropolitan Research Institute of Budapest for the Barcelona Metropolitan Area (AMB). The views expressed herein are those of the authors alone, and the AMB cannot be held responsible for any use that may be made of the information contained in this document. © Àrea Metropolitana de Barcelona June 2018 Table of contents Amsterdam . 29 Copenhagen ....................................................... 36 Greater Manchester ................................................ 42 Stuttgart .......................................................... 52 Zürich ............................................................. 60 Addressing the Metropolitan Challenge in AMB. Case Studies AMSTERDAM (Netherlands) 1. National level framework 1.1. Formal government system The Netherlands is a constitutional monarchy with that is, only binding to the administrative unit which a representative parliamentary democracy and a has developed them (OECD 2017a:21). Aside from decentralised unitary state, characterised by a strong establishing the general legal framework and setting a political tradition of broad consensus seeking in policy strategic course, the state defined -

RUTE 11 OG RUTE 24 ESBJERG - TØNDER Forundersøgelse >>> Opgradering Af Vejforbindelsen Esbjerg - Grænsen
RUTE 11 OG RUTE 24 ESBJERG - TØNDER Forundersøgelse >>> Opgradering af vejforbindelsen Esbjerg - grænsen RAPPORT 425 - 2012 RUTE 11 ESBJERG - TØNDER Forundersøgelse >>> Opgradering af vejforbindelsen Esbjerg - Grænsen Rapport 425 - 2012 REDAKTION: OPLAG: Vejdirektoratet xxx DATO: TRYK: November 2012 Vejdirektoratet LAYOUT: ISBN (NET): Vejdirektoratet 9788770607162 FOTOS: ISBN: Vejdirektoratet 9788770607148 GRUNDKORT: COPYRIGHT: © Copyright Kort- og Matrikelstyrelsen Vejdirektoratet, 2012 INDHOLD 1. INDLEDNING 5 2. SAMMENFATNING 6 3. EKSISTERENDE FORHOLD 10 4. ANDRE PLANINITIATIVER 16 5. ERHVERVSFORHOLD 18 6. LØSNINGSFORSLAG 22 7. TRAFIKALE KONSEKVENSER 28 8. AREALBEHOV 34 9. PLAN- OG MILJØFORHOLD 36 10. ANLÆGSOVERSLAG OG SAMFUNDSØKONOMI 48 E20 E20 VEJEN BRAMMING ESBJERG 11 24 32 Gredstedbro FANØ 32 RIBE 24 Gram MANDØ 11 VADEHAVET Rejsby 25 Toftlund Arrild Skærbæk RØMØ 25 11 Løgumkloster Bredebro Abild Møgeltønder Tinglev TØNDER 8 Rute 11 Rute 24 FIGUR 1.1 Undersøgelsesstrækningen 1. INDLEDNING INDLEDNING Det fremgår af aftalen om ”Bedre mobilitet”, af 26. novem- ber 2010, at der skal gennemføres en forundersøgelse af mulighederne for udbygning af strækningen mellem Esbjerg ”Bedre mobilitet” er en aftale af 26. november 2010 mellem og Tønder. regeringen (Socialdemokraterne, Det Radikale Venstre og Socialistisk Folkeparti), Venstre, Dansk Folkeparti, Liberal Alliance og Det Konservative Folkeparti. Undersøgelsen skal omfatte rute 11 mellem E20, Esbjerg- motorvejen ved Korskro og den dansk - tyske grænse syd for Tønder, en strækning på ca. 77 km. Endvidere skal rute 24 mellem Gredstedbro og Esbjerg inddrages i undersøgelsen. Denne strækning er ca. 13 km. Strækningerne er vist på figur 1.1. Forundersøgelsen skal belyse behov og muligheder for op- gradering af rute 11 samt af rute 24, ligesom undersøgelsen skal belyse de væsentligste konsekvenser i forhold til trafik, miljø og økonomi. -
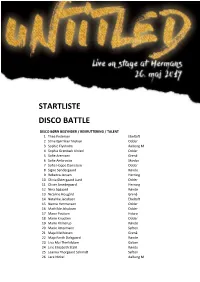
Startliste Disco Battle
d STARTLISTE DISCO BATTLE DISCO BØRN BEGYNDER / REKRUTTERING / TALENT 1 Thea Pedersen Ebeltoft 2 Stine Bjørnkær Nielsen Odder 3 Sophie Flyvholm Aalborg M 4 Sophia Grønbæk Ulsted Odder 5 Sofie Arentzen Grenå 6 Sofie Ambrosius Skovby 7 Sofia Hoppe Danielsen Odder 8 Signe Søndergaard Rønde 9 Rebecca Jensen Herning 10 Olivia Østergaard Lund Odder 11 Oliver Smedegaard Herning 12 Nina Søgaard Rønde 13 Nicoline Hougård Grenå 14 Natahlie Jacobsen Ebeltoft 15 Nanna Hermansen Odder 16 Mathilde Jakobsen Odder 17 Marie Poulsen Hobro 18 Marie Knudsen Odder 19 Marie Flinterup Rønde 20 Marie Attermann Søften 21 Maja Mathiesen Grenå 22 Maja Fanth Dalsgaard Rønde 23 Liva Mai Therkildsen Galten 24 Line Elisabeth Stahl Rønde 25 Leanna Thorgaard Schmidt Søften 26 Lara Nickel Aalborg M 1 27 Katrine Høj Kristensen Rønde 28 Josefine Hoier Galten 29 Johanne Nybye Michell Odder 30 Ida Kauffeldt Søften 31 Frida Houlberg Ballerup 32 Frida Hansen Aalborg M 33 Emma Erland Therry Odder 34 Emilie Laursen Herning 35 Emilie Jensen Odder 36 Emilia Warming Odder 37 Elise Toftelund Søften 38 Clara-Amalie Koefoed Aarhus V 39 Celine Christoffersen Skovby 40 Carla Hededam Vangsgaard Odder 41 Ashley Horley Aalborg M BØRN KONKURRENCE / SUPERKONKURRENCE 42 Regitze Andersen Hatting GT 43 Mikkeline Jagd Niekrenz Rønde 44 Mia Christensen Hatting GT 45 Klara Nygaard Ballerup 46 Karoline Mathilde Zappe Skanderborg 47 Ida Haulrik-Friis Rønde 48 Emma Bruun Rønde 49 Amanda Degn Hatting GT 50 Alida Christensen Rønde BØRN STAR / SUPERSTAR 109 Olivia Obiefule Viborg JUNIOR BEGYNDER / REKRUTTERING / TALENT 51 Thilde Hougaard Grenå 52 Sophia Vangsgaard Aalborg PH 53 Silje Gundestrup Odder 54 Ninna Vinter Bruhn Odder 55 Melina Sølvhøj Ballerup 56 Mathilde Dam Nybye Odder 57 Liv Dahl Schou Aalborg PH 58 Lina Rasmusssen Køge B. -

New Hospital Construction - Future Hospitals in Denmark
INNOVATING BETTER LIFE SUSTAINABLE HOSPITALS New Hospital Construction - Future Hospitals in Denmark WHITE PAPER SUSTAINABLE HOSPITALS Future Hospitals in Denmark About this white paper Steering Committee This white paper presents the Danish approach to new hospital Danish Ministry of Health, Martin Nyrop Holgersen, [email protected] construction and includes a wide range of innovative solutions that Danish Regions, Kristian Taageby Nielsen, [email protected] contribute to creating sustainable healthcare for the future. It is part North Denmark Region, Niels Uhrenfeldt, [email protected] of a series of white papers that show how Danish solutions can con- Region Zealand, Helle Gaub, [email protected] tribute to increase efficiency in healthcare while empowering patients Region of Southern Denmark, Torben Kyed Larsen, [email protected] and staff. Danish Export Association, Thomas Andersen, [email protected] Danish healthcare innovation is not exclusive for the Danes: many Systematic, Jacob Gade, [email protected] years of global presence show that our healthcare products and solu- tions create value internationally. Danish ideas and products are used Contributors every day in hospitals, medical clinics, ambulances, and nursing homes 3XN, Stig Vesterager Gothelf, [email protected] across the world. Agitek, Jean-Paul Bergmann, [email protected] Arkitema Architects, Birgitte Gade Ernst, [email protected] We hope to inspire you and would like to invite you to Denmark to Bim Equity, Ida Maria Sandgreen, [email protected] learn more about the Danish -

Strategic Energy Planning in Denmark at Municipal And
STRATEGIC ENERGY PLANNING IN DENMARK AT MUNICIPAL AND REGIONAL LEVEL STRATEGIC ENERGY PLANNING IN DENMARK AT MUNICIPAL AND REGIONAL LEVEL STRATEGIC ENERGY PLANNING IN DENMARK AT MUNICIPAL AND REGIONAL LEVEL STRATEGIC ENERGY PLANNING IN DENMARK AT MUNICIPAL AND REGIONAL LEVEL STRATEGIC ENERGY PLANNING IN DENMARK AT MUNICIPAL AND REGIONAL LEVEL The Danish government’s long-term vision is that Denmark becomes independent of fossil fuels. Municipalities have the local knowledge that can ensure political anchoring and commitment from citizens and local businesses to the green transition of the energy system and the economy. In their capacity as local planning and land-use authority, as owner of supply and transport companies, and as a major consumer, the municipalities are in a unique position to facilitate change. A program with 3.3 mill. EUR was launched in 2014 to support municipal strategic energy planning, providing a 50% grant for the projects. Strengthening partnerships: Cost-effective transition to green growth: • Vertically – state, region, municipality • Mapping energy efficiency and renewable energy resources • Horizontally – across municipalities • Analysing energy futures and strategic choices • Locally – businesses, supply companies, municipality • Setting targets and action plans • Internally – municipal administrations • Demonstrating green solutions • Democratically – citizens and interest organisations In total, 14 partnership projects for strategic energy planning were initiated with each their unique partnership structure and with each their individual energy perspective. The support program aimed at demonstrating different types of partnerships and tackle different aspects of a cost-effective transition to green growth. The 14 projects include 6 regional projects (in the five Danish regions) and 8 projects involving a smaller number of municipalities. -

Water in Figures 2019
WATER IN FIGURES 2019 DANVA STATISTICS & BENCHMARKING Denmark LEADER TEXT: CARL-EMIL LARSEN/ PHOTO: DANVA Wastewater heat pumps take heat production to a new level ater companies act efficiently and expenses. The total annual cost of drinking related to last year's hot summer in Denmark, create value for households and in- water and wastewater is € 771 for an average when the water companies experienced more W dustry. This document shows the family. The average water price has increased ruptures than usual as a result of the soil being water sector's key figures compiled by DANVA by only 0.94% from € 9.23 to € 9.32. It is less affected by the heat and creating more stress in “Water in figures 2019”. We will also review than the general net price trend for society as around the water pipes that caused several relevant topics including how water compa- a whole, which from 2017 to 2018 increased ruptures and resulted in water loss. nies are starting to use water as hydroelectric by more than 1%. The key figures also show that Danes have power plants to generate CO2-neutral energy, Moreover, the small change in the price access to tap water almost 24 hours a day, 365 which benefit consumers and the Danish cli- trend has to be seen in the context of the im- days of the year. Danes, on average, are without mate change plan. plementation of the "Three-Step Tariffs Model”, access to water for only 35 minutes out of the For example, Kalundborg Forsyning's new which led to cheaper wastewater prices for large 525,600 minutes in the year, which means they heat pumps pull heat out of the wastewater, consumers, and was during 2018 fully phased have access to water 99.99% of the time. -

How Cultural and Natural Heritage Can Strengthen Climate Change Adaptation CONTENS
2019 Combatting climate change culturally How cultural and natural heritage can strengthen climate change adaptation CONTENS Climate and culture – a complex relationship ...............................................................................................................3 Why include heritage in climate projects? ......................................................................................................................4 Coast 2 Coast – Climate Challenge ....................................................................................................................................6 The United Nations sustainable development goals and heritage ..................................................................7 Climate change – a major societal challenge of our time .....................................................................................8 Talanoa Dialogue ............................................................................................................................................................................9 Addressing climate change through heritage ............................................................................................................10 Actors in climate & heritage projects ...............................................................................................................................12 Marcy Rockman, International Council on Monuments and Sites Cultural Heritage as a Source of Creativity for Climate Change ............................................................14