Bacterial Factors and Immune Pathogenesis in Helicobacter Pylori Infection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Official Nh Dhhs Health Alert
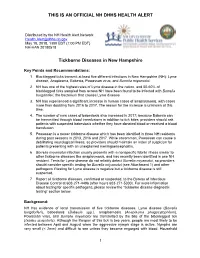
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

Iron Is an Essential Nutrient 4 Bacteria and Humans
Abstract The bhuTUV and bhuO genes play vital roles in the ability of Brucella abortus to use heme as an iron source and are regulated in an iron-responsive manner by RirA and Irr by Jenifer F. Ojeda April, 2012 Dissertation Advisor: RM Roop II Department of Microbiology and Immunology Brucella abortus is a Gram negative intracellular pathogen that causes the zoonotic disease brucellosis. Antibiotic treatment for brucellosis in humans is prolonged and sometimes followed by relapses. Currently, the United States employs prevention of the illness in humans through cattle vaccinations, eliminating the bacterium in its natural host. Unfortunately, these vaccine strains cause the disease in humans, and Brucella research ultimately aims to identify new vaccine targets as well as alternative treatment options. Brucella abortus resides in the phagosomal compartment of the host macrophage where essential nutrients such as iron are limited. Most bacteria need iron, and within the macrophage, heme is a likely source of iron due to the breakdown of red blood cells by the host macrophage. Heme transporters in Gram negative bacteria are highly conserved, and include components for outer membrane, periplasmic, and cytoplasmic membrane transport. BhuA has been previously characterized as the outer membrane heme transporter of Brucella abortus and here we report that BhuT, BhuU, and BhuV (BhuTUV) are the periplasmic and cytoplasmic heme transport components and that they are required in order for Brucella abortus to transport heme as an iron source. Utilization of heme as an iron source requires the breakdown of heme into ferrous iron, carbon monoxide, and biliverdin by a heme oxygenase. -

Phenotypic and Genomic Analyses of Burkholderia Stabilis Clinical Contamination, Switzerland Helena M.B
RESEARCH Phenotypic and Genomic Analyses of Burkholderia stabilis Clinical Contamination, Switzerland Helena M.B. Seth-Smith, Carlo Casanova, Rami Sommerstein, Dominik M. Meinel,1 Mohamed M.H. Abdelbary,2 Dominique S. Blanc, Sara Droz, Urs Führer, Reto Lienhard, Claudia Lang, Olivier Dubuis, Matthias Schlegel, Andreas Widmer, Peter M. Keller,3 Jonas Marschall, Adrian Egli A recent hospital outbreak related to premoistened gloves pathogens that generally fall within the B. cepacia com- used to wash patients exposed the difficulties of defining plex (Bcc) (1). Burkholderia bacteria have large, flexible, Burkholderia species in clinical settings. The outbreak strain multi-replicon genomes, a large metabolic repertoire, vari- displayed key B. stabilis phenotypes, including the inabil- ous virulence factors, and inherent resistance to many anti- ity to grow at 42°C; we used whole-genome sequencing to microbial drugs (2,3). confirm the pathogen was B. stabilis. The outbreak strain An outbreak of B. stabilis was identified among hos- genome comprises 3 chromosomes and a plasmid, shar- ing an average nucleotide identity of 98.4% with B. stabilis pitalized patients across several cantons in Switzerland ATCC27515 BAA-67, but with 13% novel coding sequenc- during 2015–2016 (4). The bacterium caused bloodstream es. The genome lacks identifiable virulence factors and has infections, noninvasive infections, and wound contamina- no apparent increase in encoded antimicrobial drug resis- tions. The source of the infection was traced to contaminat- tance, few insertion sequences, and few pseudogenes, ed commercially available, premoistened washing gloves suggesting this outbreak was an opportunistic infection by used for bedridden patients. After hospitals discontinued an environmental strain not adapted to human pathogenic- use of these gloves, the outbreak resolved. -

Potential of Bacterial Cellulose Chemisorbed with Anti-Metabolites, 3-Bromopyruvate Or Sertraline, to Fight Against Helicobacter Pylori Lawn Biofilm
International Journal of Molecular Sciences Article Potential of Bacterial Cellulose Chemisorbed with Anti-Metabolites, 3-Bromopyruvate or Sertraline, to Fight against Helicobacter pylori Lawn Biofilm Paweł Krzy˙zek 1,* , Gra˙zynaGo´sciniak 1 , Karol Fijałkowski 2 , Paweł Migdał 3 , Mariusz Dziadas 4 , Artur Owczarek 5 , Joanna Czajkowska 6, Olga Aniołek 7 and Adam Junka 8 1 Department of Microbiology, Faculty of Medicine, Wroclaw Medical University, 50-368 Wroclaw, Poland; [email protected] 2 Department of Immunology, Microbiology and Physiological Chemistry, Faculty of Biotechnology and Animal Husbandry, West Pomeranian University of Technology in Szczecin, 70-311 Szczecin, Poland; karol.fi[email protected] 3 Department of Environment, Hygiene and Animal Welfare, Wroclaw University of Environmental and Life Sciences, 51-630 Wroclaw, Poland; [email protected] 4 Faculty of Chemistry, University of Wroclaw, 50-353 Wroclaw, Poland; [email protected] 5 Department of Drug Form Technology, Wroclaw Medical University, 50-556 Wroclaw, Poland; [email protected] 6 Laboratory of Microbiology, Polish Center for Technology Development PORT, 54-066 Wroclaw, Poland; [email protected] 7 Faculty of Medicine, Lazarski University, 02-662 Warsaw, Poland; [email protected] 8 Department of Pharmaceutical Microbiology and Parasitology, Wroclaw Medical University, 50-556 Wroclaw, Poland; [email protected] * Correspondence: [email protected] Received: 23 November 2020; Accepted: 11 December 2020; Published: 14 December 2020 Abstract: Helicobacter pylori is a bacterium known mainly of its ability to cause persistent inflammations of the human stomach, resulting in peptic ulcer diseases and gastric cancers. Continuous exposure of this bacterium to antibiotics has resulted in high detection of multidrug-resistant strains and difficulties in obtaining a therapeutic effect. -

Gastroenteritis and Transmission of Helicobacter Pylori Infection in Households1 Sharon Perry,* Maria De La Luz Sanchez,* Shufang Yang,* Thomas D
Gastroenteritis and Transmission of Helicobacter pylori Infection in Households1 Sharon Perry,* Maria de la Luz Sanchez,* Shufang Yang,* Thomas D. Haggerty,* Philip Hurst,† Guillermo Perez-Perez,‡ and Julie Parsonnet* The mode of transmission of Helicobacter pylori gastrointestinal infections, infection is associated with infection is poorly characterized. In northern California, conditions of crowding and poor hygiene (7,8) and with 2,752 household members were tested for H. pylori infec- intrafamilial clustering (9–12). The organism has been tion in serum or stool at a baseline visit and 3 months later. recovered most reliably from vomitus and from stools dur- Among 1,752 person considered uninfected at baseline, ing rapid gastrointestinal transit (13). These findings raise 30 new infections (7 definite, 7 probable, and 16 possible) occurred, for an annual incidence of 7% overall and 21% the hypothesis that gastroenteritis episodes provide the in children <2 years of age. Exposure to an infected opportunity for H. pylori transmission. household member with gastroenteritis was associated Household transmission of gastroenteritis is common in with a 4.8-fold (95% confidence interval [CI] 1.4–17.1) the United States, particularly in homes with small chil- increased risk for definite or probable new infection, with dren (14). If H. pylori is transmitted person to person, one vomiting a greater risk factor (adjusted odds ratio [AOR] might expect rates of new infection to be elevated after 6.3, CI 1.6–24.5) than diarrhea only (AOR 3.0, p = 0.65). exposure to persons with H. pylori–infected cases of gas- Of probable or definite new infections, 75% were attributa- troenteritis. -

Package Inserts
Individuals using assistive technology may not be able to fully access the information contained in this file. For assistance, please send an e-mail to: [email protected] and include 508 Accommodation and the title of the document in the subject line of your e-mail. HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use • Carefully consider benefits and risks before administering VAXELIS to VAXELIS safely and effectively. See full prescribing information for persons with a history of: VAXELIS. - fever ≥40.5°C (≥105°F), hypotonic-hyporesponsive episode (HHE) or VAXELISTM (Diphtheria and Tetanus Toxoids and Acellular Pertussis, persistent, inconsolable crying lasting ≥3 hours within 48 hours after a Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B previous pertussis-containing vaccine. (5.2) Vaccine) - seizures within 3 days after a previous pertussis-containing vaccine. (5.2) Suspension for Intramuscular Injection Initial U.S. Approval: 2018 • If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome ----------------------------RECENT MAJOR CHANGES ------------------------ may be increased following VAXELIS. (5.3) Dosage and Administration (2.2) 09/2020 • Apnea following intramuscular vaccination has been observed in some ----------------------------INDICATIONS AND USAGE--------------------------- infants born prematurely. The decision about when to administer an VAXELIS is a vaccine indicated for active immunization to prevent intramuscular vaccine, including VAXELIS, to an infant born prematurely diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease should be based on consideration of the individual infant’s medical status due to Haemophilus influenzae type b. -

Pseudomonas Aeruginosa1
The Journal of Immunology IL-17 Is a Critical Component of Vaccine-Induced Protection against Lung Infection by Lipopolysaccharide-Heterologous Strains of Pseudomonas aeruginosa1 Gregory P. Priebe,2*†‡ Rebecca L. Walsh,* Terra A. Cederroth,* Akinobu Kamei,* Yamara S. Coutinho-Sledge,* Joanna B. Goldberg,§ and Gerald B. Pier*‡ In a murine model of acute fatal pneumonia, we previously showed that nasal immunization with a live-attenuated aroA deletant of Pseudomonas aeruginosa strain PAO1 elicited LPS serogroup-specific protection, indicating that opsonic Ab to the LPS O Ag was the most important immune effector. Because P. aeruginosa strain PA14 possesses additional virulence factors, we hypoth- esized that a live-attenuated vaccine based on PA14 might elicit a broader array of immune effectors. Thus, an aroA deletant of PA14, denoted PA14⌬aroA, was constructed. PA14⌬aroA-immunized mice were protected against lethal pneumonia caused not only by the parental strain but also by cytotoxic variants of the O Ag-heterologous P. aeruginosa strains PAO1 and PAO6a,d. Remarkably, serum from PA14⌬aroA-immunized mice had very low levels of opsonic activity against strain PAO1 and could not passively transfer protection, suggesting that an antibody-independent mechanism was needed for the observed cross-serogroup protection. Compared with control mice, PA14⌬aroA-immunized mice had more rapid recruitment of neutrophils to the airways early after challenge. T cells isolated from P. aeruginosa ⌬aroA-immunized mice proliferated and produced IL-17 in high quan- tities after coculture with gentamicin-killed P. aeruginosa. Six hours following challenge, PA14⌬aroA-immunized mice had sig- nificantly higher levels of IL-17 in bronchoalveolar lavage fluid compared with unimmunized, Escherichia coli-immunized, or PAO1⌬aroA-immunized mice. -

Identification of Bordetella Spp. in Respiratory Specimens From
504 Clinical Microbiology and Infection, Volume 14 Number 5, May 2008 isolates of extended-spectrum-beta-lactamase-producing Original Submission: 27 October 2007; Revised Sub- Shigella sonnei. Ann Trop Med Parasitol 2007; 101: 511–517. mission: 5 December 2007; Accepted: 19 December 21. Rice LB. Controlling antibiotic resistance in the ICU: 2007 different bacteria, different strategies. Cleve Clin J Med 2003; 70: 793–800. Clin Microbiol Infect 2008; 14: 504–506 22. Boyd DA, Tyler S, Christianson S et al. Complete nucleo- 10.1111/j.1469-0691.2008.01968.x tide sequence of a 92-kilobase plasmid harbouring the CTX-M-15 extended spectrum b-lactamase involved in an outbreak in long-term-care facilities in Toronto, Canada. Cystic fibrosis (CF) is an autosomal recessive Antimicrob Agents Chemother 2004; 48: 3758–3764. disease, characterised by defective chloride ion channels that result in multi-organ dysfunction, most notably affecting the respiratory tract. The RESEARCH NOTE alteration in the pulmonary environment is asso- ciated with increased susceptibility to bacterial infection. Recent advances in bacterial taxonomy and improved microbial identification systems Identification of Bordetella spp. in have led to an increasing recognition of the respiratory specimens from individuals diversity of bacterial species involved in CF lung with cystic fibrosis infection. Many such species are opportunistic T. Spilker, A. A. Liwienski and J. J. LiPuma human pathogens, some of which are rarely found in other human infections [1]. Processing Department of Pediatrics and Communicable of CF respiratory cultures therefore employs Diseases, University of Michigan Medical selective media and focuses on detection of School, Ann Arbor, MI, USA uncommon human pathogens. -

1 Is Helicobacter Pylori Good for You?
University of Maryland School of Medicine A Third Century Is Helicobacter pylori Good for You? To Treat or Not to Treat, That is the Question Steven J. Czinn, M.D. Professor and Chair University of Maryland School of Medicine Department of Pediatrics Baltimore, Maryland America’s Oldest Public Medical School - USA Where Discovery Transforms Medicine Learning Objectives Disclosure • To demonstrate that H. pylori is responsible In the past 12 months, I have had no relevant for a significant portion of gastroduodenal financial relationships with the disease. manufacturer(s) of any commercial product(s) • To understand how the host immune response and/or provider(s) of commercial services contributes to Helicobacter associated discussed in this CME activity. disease. • To understand how the host immune response to Helicobacter infection might prevent asthma. • To understand which patient populations should be treated. H. pylori is an Important Human Pathogen World-Wide Prevalence of H. pylori • H. pylori is a gram negative microaerophilic bacterium that selectively colonizes the stomach. 70% 80% • It infects about 50% of the world’s population. 30% 70% 30% 50% • It is classically considered a non-invasive organism, 40% 50% 70% 70% • There is a vigorous innate and adaptive immune 70% 90% response and inflammation that is Th1 predominant 70% and includes (chronic) lymphocyte and (active) 90% 80% 80% 70% neutrophil components. 20% • Despite this response the bacterium generally persists for the life of the host. Marshall, 1995 JAMA 274:1064 1 Natural History of H. pylori infection Eradicating H. pylori Treats or Prevents: Colon Gastric cancer??? Initial infection (in childhood) Adenocarcinoma Nonulcer Chronic gastritis (universal) Dyspepsia H. -

Helicobacter Spp. — Food- Or Waterborne Pathogens?
FRI FOOD SAFETY REVIEWS Helicobacter spp. — Food- or Waterborne Pathogens? M. Ellin Doyle Food Research Institute University of Wisconsin–Madison Madison WI 53706 Contents34B Introduction....................................................................................................................................1 Virulence Factors ...........................................................................................................................2 Associated Diseases .......................................................................................................................2 Gastrointestinal Disease .........................................................................................................2 Neurological Disease..............................................................................................................3 Other Diseases........................................................................................................................4 Epidemiology.................................................................................................................................4 Prevalence..............................................................................................................................4 Transmission ..........................................................................................................................4 Summary .......................................................................................................................................5 -

Screening Practices for Infectious Diseases Among Burmese Refugees in Australia Nadia J
Screening Practices for Infectious Diseases among Burmese Refugees in Australia Nadia J. Chaves,1 Katherine B. Gibney,1 Karin Leder, Daniel P. O’Brien, Caroline Marshall, and Beverley-Ann Biggs Increasing numbers of refugees from Burma (Myan- eases Service outpatient clinics at the Royal Melbourne mar) are resettling in Western countries. We performed a Hospital, Australia, during January 1, 2004–December retrospective study of 156 Burmese refugees at an Austra- 31, 2008. Patients were identifi ed through the hospital lian teaching hospital. Of those tested, Helicobacter pylori registration database, and medical, pathologic, radiolog- infection affected 80%, latent tuberculosis 70%, vitamin D ic, and pharmacologic records were reviewed. Screening defi ciency 37%, and strongyloidiasis 26%. Treating these tests audited included those suggested by the Australasian diseases can prevent long-term illness. Society for Infectious Diseases refugee screening guide- lines (5), along with vitamin D and hematologic studies. urma (Myanmar) has been the most common country These latter tests included full blood count, mean corpus- Bof origin for refugees who have recently resettled in cular volume, and platelet count. Investigations were per- the United States and Australia (1,2). Before resettling in formed at the discretion of the treating doctor, and not all Australia, most refugees undergo testing for HIV, have a tests were performed for each patient. Time was calculated chest radiograph to exclude active tuberculosis (TB), and from time of arrival in Australia to fi rst clinic attendance. may undergo other testing, depending on exposure risk. The results of serologic tests and QuantiFERON-TB Gold Many refugees also receive a health check and treatment tests (QFT-G; Cellestis Limited, Carnegie, Victoria, Aus- for malaria and stool parasites within 72 hours of departure tralia), were interpreted according to the manufacturers’ for Australia (3,4). -

Metagenomics Analysis Reveals the Microbial Communities
diversity Article Metagenomics Analysis Reveals the Microbial Communities, Antimicrobial Resistance Gene Diversity and Potential Pathogen Transmission Risk of Two Different Landfills in China Shan Wan 1,†, Min Xia 2,†, Jie Tao 1, Yanjun Pang 1, Fugen Yu 1,* , Jun Wu 3,* and Shanping Chen 2,* 1 State Key Laboratory of Pharmaceutical Biotechnology, School of Life Sciences, Nanjing University, Nanjing 210023, China; [email protected] (S.W.); [email protected] (J.T.); [email protected] (Y.P.) 2 Shanghai Environmental Sanitation Engineering Design Institute Co., Ltd., Shanghai 200232, China; [email protected] 3 State Key Laboratory of Pollution Control and Resource Reuse, School of Environment, Nanjing University, Nanjing 210023, China * Correspondence: [email protected] (F.Y.); [email protected] (J.W.); [email protected] (S.C.) † There authors contribute equally to this work. Abstract: In this study, we used a metagenomic approach to analyze microbial communities, antibiotic resistance gene diversity, and human pathogenic bacterium composition in two typical Citation: Wan, S.; Xia, M.; Tao, J.; landfills in China. Results showed that the phyla Proteobacteria, Bacteroidetes, and Actinobacte- Pang, Y.; Yu, F.; Wu, J.; Chen, S. ria were predominant in the two landfills, and archaea and fungi were also detected. The genera Metagenomics Analysis Reveals the Methanoculleus, Lysobacter, and Pseudomonas were predominantly present in all samples. sul2, sul1, Microbial Communities, tetX, and adeF were the four most abundant antibiotic resistance genes. Sixty-nine bacterial pathogens Antimicrobial Resistance Gene were identified from the two landfills, with Klebsiella pneumoniae, Bordetella pertussis, Pseudomonas Diversity and Potential Pathogen aeruginosa, and Bacillus cereus as the major pathogenic microorganisms, indicating the existence of Transmission Risk of Two Different potential environmental risk in landfills.