Traumatic Injuries: Imaging of Peripheral Muskuloskeletal Injuries 2.11
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Defining the Morphometrics of the First Metacarpal for the Development of an Osseointegrated Prosthesis
Defining the Morphometrics of the First Metacarpal for the Development of an Osseointegrated Prosthesis Authors: JJ Vaux OMS-IV1, RR Hugate, M.D.2, JW Hills3, RF Grzybowski, D.O.4, CK Funk. Ph.D.1 Affiliations: 1Rocky Vista University College of Osteopathic Medicine, 2Colorado Limb Consultants, 3Dept of Materials and Mechanical Engineering, Denver University, 4Diversified Radiology Objective: Amputation of the thumb presents a serious insult to the hand and can result in up to a 22% loss of functionality in that limb (2,3). To date, several different techniques have been explored for reconstruction of the thumb, however none seem to be incredibly successful (1,4). We believe the answer lies in an osseointegrated prosthesis within the first metacarpal. In order to successfully create an osseointegrated prosthesis, the morphometrics of the first metacarpal are needed. The aim of this study was to define the geometry of the first metacarpal in order to help create a standardized set of stems and prostheses to treat patients who have suffered amputation of the thumb at the level of the first metacarpal phalangeal joint (MCPJ). Methods: A total of eighty first metacarpals from forty-one cadavers were studied. All soft tissues were removed and the first metacarpals were imaged by computed tomography (CT). Three-dimensional models were constructed using cuts from the coronal, sagittal, and axial planes. Using a HyperMesh software, the individual first metacarpals were analyzed and measurements were taken for overall length, radius of curvature, medullary canal diameter, cortical thickness, and distance from the distal end to the center of the isthmus. -

Orthopaedics Essentials
Frykman Classification of Distal Fracture of base of the first Neer classification of proximal humeral head # Radial # metacarpal bone 1-part 2-part 3-part 4-part GT GT+SN “CLASSIC” SN LT+SN (RARE) “VALGUS IMPACTED” Galeazzi Fracture LN (RARE) Impression # Head split Gartland’s classification of supracondylar Fracture shaft of ulnar, together with distal third of radius with fracture of humerus disruption of the proximal radioulnar dislocation or subluxation of distal joint and dislocation of radiocapitallar radio-ulnar joint joint Salter–Harris fracture = Fracture that involves the epiphyseal plate or growth plate of a bone Type I: undisplaced or minimally displaced fractures. Type II: displaced with posterior cortex intact Type III: displaced with no cortical intact Gustillo Anderson Classification of Open Fracture I – open fracture with a wound <1cm and clean II – open fracture with wound > 1cm with extensive soft tissue damage and avulsion of flaps IIIa – open fracture with adequate soft tissue coverage of bone in • Galeazzi fracture - a fracture of the radius spite of extensive soft tissue laceration or flaps or high energy with dislocation of the distal radioulnar joint trauma irrespective of size of wound • Colles' fracture - a distal fracture of the IIIb – open fracture with extensive soft tissue loss, periosteal radius with dorsal (posterior) displacement of the wrist and hand stripping and exposure of bone • Smith's fracture - a distal fracture of the IIIc – open fracture associated with an arterial injury which requires radius with volar (ventral) displacement of the I II IIIa IIIb IIIc repair wrist and hand • Barton's fracture - an intra-articular fracture of the distal radius with dislocation of Irrigation: 3L 6L 9L ORTHOPAEDICS CLASSIFICATION the radiocarpal joint • Essex-Lopresti fracture - a fracture of PART 1 (UPPER LIMB) the radial head with concomitant dislocation HTARW5B/GKS2013/3- of the distal radio-ulnar joint with disruption of Together In Delivering Excellence (T.I.D.E.) the interosseous membrane Contributors: Dr. -

CASE REPORT Injuries Following Segway Personal
UC Irvine Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health Title Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature Permalink https://escholarship.org/uc/item/37r4387d Journal Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health, 16(5) ISSN 1936-900X Authors Ashurst, John Wagner, Benjamin Publication Date 2015 DOI 10.5811/westjem.2015.7.26549 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California CASE REPORT Injuries Following Segway Personal Transporter Accidents: Case Report and Review of the Literature John Ashurst DO, MSc Conemaugh Memorial Medical Center, Department of Emergency Medicine, Benjamin Wagner, DO Johnstown, Pennsylvania Section Editor: Rick A. McPheeters, DO Submission history: Submitted April 20, 2015; Accepted July 9, 2015 Electronically published October 20, 2015 Full text available through open access at http://escholarship.org/uc/uciem_westjem DOI: 10.5811/westjem.2015.7.26549 The Segway® self-balancing personal transporter has been used as a means of transport for sightseeing tourists, military, police and emergency medical personnel. Only recently have reports been published about serious injuries that have been sustained while operating this device. This case describes a 67-year-old male who sustained an oblique fracture of the shaft of the femur while using the Segway® for transportation around his community. We also present a review of the literature. [West J Emerg Med. 2015;16(5):693-695.] INTRODUCTION no parasthesia was noted. In 2001, Dean Kamen developed a self-balancing, zero Radiograph of the right femur demonstrated an oblique emissions personal transportation vehicle, known as the fracture of the proximal shaft of the femur with severe Segway® Personal Transporter (PT).1 The Segway’s® top displacement and angulation (Figure). -

The Carpometacarpal Joint of the Thumb: MR Appearance in Asymptomatic Volunteers
Skeletal Radiol (2013) 42:1105–1112 DOI 10.1007/s00256-013-1633-4 SCIENTIFIC ARTICLE The carpometacarpal joint of the thumb: MR appearance in asymptomatic volunteers Anna Hirschmann & Reto Sutter & Andreas Schweizer & Christian W. A. Pfirrmann Received: 23 January 2013 /Revised: 1 April 2013 /Accepted: 21 April 2013 /Published online: 15 May 2013 # ISS 2013 Abstract subjects. The AOL showed a variable SI (36 %/42 % low, Purpose To prospectively characterize the MR appearance 27 %/27 % increased, 36 %/30 % striated). The IML was the of the carpometacarpal (CMC) joint of the thumb in asymp- thickest ligament with a mean of 2.9 mm/3.1 mm and the tomatic volunteers. DRL the thinnest (1.2 mm/1.4 mm). There was a mean Materials and methods Thirty-four asymptomatic volun- dorsal subluxation of 1.8 mm/2.0 mm and radial subluxation teers (17 women, 17 men, mean age, 33.9±9.2 years) of 2.8 mm/3.4 mm of the metacarpal base. The AOL was underwent MR imaging of the thumb after approval by the significantly thicker in men (1.7 mm) than in women local ethical committee. Two musculoskeletal radiologists (1.2 mm; p=0.02). Radial subluxation was significantly independently classified visibility and signal intensity (SI) larger in men (3.4 mm) than in women (2.2 mm; p=0.02). characteristics of the anterior oblique (AOL/beak ligament), No subluxation in palmar or ulnar direction was seen. the posterior oblique (POL), the intermetacarpal (IML), and Conclusions Radial and dorsal subluxation of the CMC the dorsoradial ligaments (DRL) on a three-point Likert joint can be a normal finding in a resting position at MR scale. -

Body Mass Index As a Predictor for Diagnosis of Associated Injuries in Femoral Head Fracture Patients: a Retrospective Study Edem GAP*, Zhijun P, Jiaqi W and Jiang L
Research iMedPub Journals ARCHIVES OF MEDICINE 2018 www.imedpub.com Vol.10 No.6:3 ISSN 1989-5216 DOI: 10.21767/1989-5216.1000290 Body Mass Index as a Predictor for Diagnosis of Associated Injuries in Femoral Head Fracture Patients: A Retrospective Study Edem GAP*, Zhijun P, Jiaqi W and Jiang L Department of Orthopedic Surgery, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, Zhejiang Province, China *Corresponding author: Ghamor-Amegavi Prince Edem, Department of Orthopedic Surgery, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, Zhejiang Province, China, Tel: +8613588064446; E-mail: [email protected] Received date: October 29, 2018; Accepted date: November 20, 2018; Published date: November 23, 2018 Citation: Edem GAP, Zhijun P, Jiaqi W, Jiang L (2018) Body Mass Index as a Predictor for Diagnosis of Associated Injuries in Femoral Head Fracture Patients: A Retrospective Study. Arch Med Vol No:10 Iss No:6:3 Copyright: ©2018 Edem GAP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction Abstract In 1895, an autopsy was performed on a 35-year-old woman who had fallen from 2nd floor story building by John [1]. He Purpose: To investigate the relationship between observed prior to the procedure that the left leg was inverted associated injuries (AI) suffered at time of accident in and slightly shorter than the right leg. This was the first report femoral head fracture (FHF) patients with age, sex, of femoral head fracture (FHF) in history. -

Hand Rehabilitation Current Awareness Bulletin NOVEMBER 2015
1 Hand Rehabilitation Current Awareness Bulletin NOVEMBER 2015 2 Lunchtime Drop-in Sessions The Library and Information Service provides free specialist information skills training for all UHBristol staff and students. To book a place, email: [email protected] If you’re unable to attend we also provide one-to-one or small group sessions. Contact library@ or katie.barnard@ to arrange a session. Literature Searching October (12pm) An in -depth guide on how to search Thurs 8th Statistics the evidence base, including an introduction to UpToDate and Fri 16th Literature Searching Anatomy.tv. Mon 19th Understanding articles Tues 27th Statistics Useful for anybody who wants to find the best and quickest way to source articles. November (1pm) Weds 4th Literature Searching Thurs 12th Understanding articles How to understand an article Fri 20th Statistics How to assess the strengths and Mon 23rd Literature Searching weaknesses of published articles. Examining bias and validity. December (12pm) Tues 1st Understanding articles Weds 9th Statistics Medi cal Statistics Thurs 17th Literature Searching A basic introduction to the key statistics in medical articles. Giving an overview of statistics that compare risk, test confidence, analyse clinical investigations, and test difference. 3 Contents Contents .................................................................................................................................................. 3 New from Cochrane Database of Systematic Reviews .......................................................................... -

Lag Screw Fixation for Treatment of an Ulnar Styloid Process Fracture with Antebrachiocarpal Joint Luxation in a Cat
Published online: 2019-06-04 THIEME e32 Case Report Lag Screw Fixation for Treatment of an Ulnar Styloid Process Fracture with Antebrachiocarpal Joint Luxation in a Cat Lindsay A. Parker1 Amy S. Kapatkin2 Mark C. Fuller3 1 Department of Companion Animals, Atlantic Veterinary College, Address for correspondence Lindsay A. Parker, DVM, Atlantic University of Prince Edward Island, Charlottetown, Canada Veterinary College, University of Prince Edward Island, 550 University 2 Department of Surgical and Radiological Sciences, University of Avenue, Charlottetown, PEI, C1A 4P3, Canada California, Davis, CA, United States (e-mail: [email protected]). 3 Fuller Animal Specialty Surgery, Airdrie, AB, Canada VCOT Open 2019;2:e32–e35. Abstract Fracture of the ulnar styloid process can result in clinically debilitating antebrachio- carpal instability. Previously described repair methods include Kirschner wire and figure Keywords of eight tension band wire and/or intramedullary pinning. This case report describes ► feline ulnar styloid surgical repair of a short oblique ulnar styloid process fracture in a cat using two fracture cortical screws placed in lag fashion. Recheck evaluation confirmed lameness-free full ► osteosynthesis return to function with anatomical fracture healing. Introduction acic limb and, on examination under sedation, was found to Lateral styloid process fractures generally require surgical have a marked soft tissue swelling associated with the distal stabilization to avoid carpal instability and to act as a right antebrachium and increased lateral carpal laxity. physical buttress to provide normal joint function.1 Due to Radiographs revealed an antebrachiocarpal joint luxa- the small diameter of the feline distal ulna, these types of tion with an oblique ulnar styloid process fracture (►Fig. -

Radial Head Fractures Treated with Open Reduction and Internal Fixation
Moghaddam et al. Trauma Cases Rev 2016, 2:028 Volume 2 | Issue 1 ISSN: 2469-5777 Trauma Cases and Reviews Research Article: Open Access Radial Head Fractures Treated with Open Reduction and Internal Fixation Moghaddam A1*, Raven TF1, Kaghazian P1, Studier-Fischer S2, Swing T1, Grützner PA2 and Biglari B2 1Trauma & Reconstructive Surgery, University hospital Heidelberg, Germany 2BG Unfallklinik, Ludwigshafen, Germany *Corresponding author: Prof. Dr. med. Arash Moghaddam, Consultant Orthopaedic & Trauma Surgeon Center of Trauma, Orthopaedics & Paraplegiology, Division of Trauma & Reconstructive Surgery, University hospital Heidelberg, Schlierbacher Landstraße 200a, 69118 Heidelberg, Germany, Tel: 0049-6221-5626263, Fax: 0049- 6221-26298, E-mail: [email protected] to a high percentage of associated injuries [6]. The combination of a Abstract dislocated fracture and unstable joint makes operative treatment as Background: Radial head fractures are responsible for 2 to 5% of well as early mobilization difficult. Other treatment options include adult fractures. Especially problematic is the treatment of dislocated the implantation of a radial head prosthesis and resection of the and unstable fractures which often have a worst prognosis. The radial head. The radial head prosthesis has become established as the purpose of this study was to evaluate the results of open reduction choice of treatment for multi-fragmented radial head fractures with and internal fixation (ORIF) in the treatment of radial head fractures. associated injuries, while resection of the radial head has increasingly Materials and Methods: Between June 2001 and January 2006, fallen out of use and is now reserved for isolated fractures of the 41 reconstructive surgical procedures were executed. Thirty-seven radial head without associated injuries [7]. -

Del Vecchio Upper Extremity Injury
UPPER EXTREMITY INJURIES Jeff Del Vecchio MPAS, PA-C, DFAAPA Mercy Clinic Orthopedics Springfield, Missouri OBJECTIVES IDENTIFY COMMON UPPER EXTREMITY INJURIES AND FRACTURES REVIEW EXAMINATION TECHNIQUES FOR COMMON UPPER EXTREMITY INJURIES DISCUSS AND REVIEW RADIOGRAPHIC FINDINGS OF UPPER EXTREMITY FRACTURES DISCUSS AND REVIEW TREATMENT OPTIONS FOR COMMON UPPER EXTREMITY INJURIES LATERAL EPICONDYLITIS Tennis elbow Definition Pain about lateral aspect of elbow Involves extensor musculature Rotation of arm and wrist extension Secondary to repetitive overuse or injury Microtears to tendon⇒ inflammation⇒fibrosis⇒degeneration Affects pt’s 30-60 yrs Clinical symptoms Outside elbow and back of upper forearm pain Pain lifting with palm facing down Holding lightweight objects difficult Physical Examination Lateral epicondylar area tender to palpation Tennis elbow test- elbow 90 deg, extend wrist against resistance. +pain at lateral epicondaylar area Radiographs Obtain to rule out osteoarthritis or calcifications Treatment NSAID’s (10-14 days) Avoid activities causing pain Heat or ice Corticosteroid injection Stretching and gradual strengthening program Tennis elbow strap MEDIAL EPICONDYLITIS Golfer’s elbow Definition Inflammation of flexor-pronator’s Less common than lateral epicondylitis Clinical Symptoms Medial elbow pain Physical Examination Pain with palpation over medial condyle Pain with flexion and pronation of wrist against resistance Rule out ulnar neuropathy Treatment Same as lateral epicondylitis CLAVICLE FRACTURE Most common bone injury -

Clinical Medical Policy
CLINICAL MEDICAL POLICY Noninvasive Electrical Bone Growth Stimulators Policy Name: (osteogenesis stimulators) Policy Number: MP-070-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 12/15/2018 Issue Date: 01/15/2019 Effective Date: 01/15/2019 Annual Approval Date: 10/17/2019 Revision Date: N/A Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 78 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ may provide coverage under the medical-surgical and DME benefits of the Company’s Medicaid products for medically necessary noninvasive electrical bone growth stimulators as treatment of nonunion long bone fractures or congenital pseudarthrosis. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-070-MD-PA Page 1 of 78 DEFINITIONS Prior Authorization Review Panel - A panel of representatives from within the PA Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Non-invasive (Osteogenic) Electrical Bone Growth Stimulator – A device that uses pulsed- electromagnetic fields, capacitative coupling or combined magnetic fields to generate a weak electric current through the target site. -

Ipsilateral Intertrochanteric and Pipkin Fractures
Case Report & Literature Review Ipsilateral Intertrochanteric and Pipkin The Role of Fractures: An Unusual Case Aspirin Mustafa H. Khan, MD, Vonda J. Wright, MD, and Michael J. Prayson, MD racture-dislocation of the femoral head most com- and internal fixation (ORIF). He was returned to the operat- Keith R monly results from high-energy trauma, such as that ing room on postoperative day 5. The anterior approach was sustained in falls and motor vehicle accidents. This used to remove several small loose osteochondral fragments injury may be associated with ipsilateral femoral from the hip, and the femoral head fracture fragment was Fneck and acetabular fractures. However, femoral head frac- reduced and fixed with 2 countersunk 4.0-mm cancellous ture-dislocation with an ipsilateral intertrochanteric fracture screws. Intraoperative fluoroscopy showed that the hip had is an extremely rare injury, with only 2 previous cases full, smooth range of motion without fracture displacement. reported in the literature.1,2 Postoperative x-rays showed successful reduction and fixa- In the present report, we describe a case of this unusual tion of the fracture (Figure 3). fracture pattern and briefly review the relevant literature, anatomy, and treatment options. CASE REPORT A man in his early 40s sustained injuries in a car acci- dent. At presentation he was awake and alert and com- plained of pain in the chest, right hip, and right leg. The evaluation and treatment of his orthopedic injuries are described in this case report. Orthopedic evaluation revealed a right posterior hip dislocation with an associated femoral head fracture, a right femoral intertrochanteric fracture, right superior and inferior pelvic rami fractures (Figure 1), and an open type IIIA right tibia fracture. -
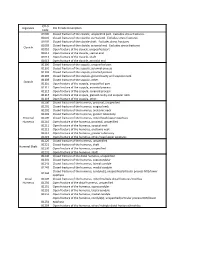
ICD*9, Diganosis ICD*9,Code,Description Code 81000 Closed,Fracture,Of,The,Clavicle,,Unspecified,Part.,,Excludes,Stress,Fractures
ICD*9, Diganosis ICD*9,Code,Description Code 81000 Closed,fracture,of,the,clavicle,,unspecified,part.,,Excludes,stress,fractures. 81001 Closed,fracture,of,the,clavicle,,sternal,end.,,Excludes,stress,fractures. 81002 Closed,fracture,of,the,clavicle,shaft.,,Excludes,stress,fractures. 81003 Closed,fracture,of,the,clavicle,,acromial,end.,,Excludes,stress,fractures. Clavicle 81010 Open,fracture,of,the,clavicle,,unspecified,part 81011 Open,fracture,of,the,clavicle,,sternal,end 81012 Open,fracture,of,the,clavicle,,shaft 81013 Open,fracture,of,the,clavicle,,acromial,end 81100 Closed,fracture,of,the,scapula,,unspecified,part 81101 Closed,fracture,of,the,scapula,,acromial,process 81102 Closed,fracture,of,the,scapula,,coracoid,process 81103 Closed,fracture,of,the,scapula,,glenoid,cavity,and,scapular,neck 81109 Closed,fracture,of,the,scapula,,other. Scapula 81110 Open,fracture,of,the,scapula,,unspecified,part 81111 Open,fracture,of,the,scapula,,acromial,process 81112 Open,fracture,of,the,scapula,,coracoid,process 81113 Open,fracture,of,the,scapula,,glenoid,cavity,and,scapular,neck 81119 Open,fracture,of,the,scapula,,other. 81200 Closed,fracture,of,the,humerus,,proximal,,unspecified 81201 Closed,fracture,of,the,humerus,,surgical,neck 81202 Closed,fracture,of,the,humerus,,anatomic,neck 81203 Closed,fracture,of,the,humerus,,greater,tuberosity Proximal, 81209 Closed,fracture,of,the,humerus,,other/head/upper,epiphysis Humerus 81210 Open,fracture,of,the,humerus,,proximal,,unspecified 81211 Open,fracture,of,the,humerus,,surgical,neck 81212 Open,fracture,of,the,humerus,,anatomic,neck