Standing Committee on Defence (2005-06)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nagar Nigam Rajnandgaon
Rajnandgaon is the quality city of Rajnandgaon District, in the state of Chhattisgarh, India. As of the 2011 census the population of the city was 163,122.[2] Rajnandgaon district came into existence on 26 January 1973, as a result of the division of Durg district.[3] Rajnandgaon City of Chhattisgarh Nickname(s): Nandgaon Rajnandgaon Location in Chhattisgarh, India Coordinates: 21.10°N 81.03°ECoordinates: 21.10°N 81.03°E Country India State Chhattisgarh District Rajnandgaon Government • Type Democratic • Body Nagar Nigam • Mayor Madhusudan yadav Elevation 307 m (1,007 ft) Population (2011)[1] • Total 163,122 • Rank 7th in State Time zone IST (UTC+5:30) PIN 491441 Telephone code 07744 Vehicle registration CG-08 Sex ratio 1023 ♂/♀ History[edit] Main article: Nandgaon State Originally known as Nandgram, Rajnandgaon State was ruled by Somvanshis, Kalachuris of Tripuri and Marathas.[4] The palaces in the town of Rajnandgaon reveal their own tale of the rulers, their society and culture, and the traditions of those times.[3] The city was ruled by a dynasty of Hindu caretakers (mahants), who bore the title Vaishnav and Gond rajas (chiefs). Succession was by adoption. Its foundation is traced to a religious celibate, who came from the Punjab towards the end of the 18th century. From the founder it passed through a succession of chosen disciples until 1879, when the British government recognized the ruler as an hereditary chief and it came to be known as princely state of Raj Nandgaon. Afterwards conferred upon his son the title of Raja Bahadur. The first ruler Ghasi Das Mahant, was recognized as a feudal chief by the British government in 1865 and was granted a sanad of adoption. -

Who's Who – India As on 29.04.2010
Who's Who – India as on 29.04.2010 President of India Smt. Pratibha Devisingh Patil Vice President of India Shri Mohd. Hamid Ansari Prime Minister of India Dr. Manmohan Singh Cabinet Ministers Serial Portfolio Name of Minister Number Prime Minister and also In‐Charge of the Ministries/Departments viz: Ministry of Personnel, Public Grievances & Pensions; 1. Ministry of Planning; Dr. Manmohan Singh Ministry of Water Resources; Department of Atomic Energy; and Department of Space 2. Minister of Finance Shri Pranab Mukherjee Minister of Agriculture and Minister of Consumer Affairs, Food 3. Shri Sharad Pawar & Public Distribution 4. Minister of Defence Shri A.K. Antony 5. Minister of Home Affairs Shri P. Chidambaram 6. Minister of Railways Km. Mamata Banerjee 7. Minister of External Affairs Shri S.M. Krishna 8. Minister of Steel Shri Virbhadra Singh Shri Vilasrao 9. Minister of Heavy Industries and Public Enterprises Deshmukh 10. Minister of Health and Family Welfare Shri Ghulam Nabi Azad Shri Sushil Kumar 11. Minister of Power Shinde Shri M. Veerappa 12. Minister of Law and Justice Moily 13. Minister of New and Renewable Energy Dr. Farooq Abdullah 14. Minister of Urban Development Shri S. Jaipal Reddy 15. Minister of Road Transport and Highways Shri Kamal Nath 16. Minister of Overseas Indian Affairs Shri Vayalar Ravi 17. Minister of Textiles Shri Dayanidhi Maran 18. Minister of Communications and Information Technology Shri A. Raja 19. Minister of Petroleum and Natural Gas Shri Murli Deora 20. Minister of Information and Broadcasting Smt. Ambika Soni Shri Mallikarjun 21. Minister of Labour and Employment Kharge 22. -

T He Indian Army Is Well Equipped with Modern
Annual Report 2007-08 Ministry of Defence Government of India CONTENTS 1 The Security Environment 1 2 Organisation and Functions of The Ministry of Defence 7 3 Indian Army 15 4 Indian Navy 27 5 Indian Air Force 37 6 Coast Guard 45 7 Defence Production 51 8 Defence Research and Development 75 9 Inter-Service Organisations 101 10 Recruitment and Training 115 11 Resettlement and Welfare of Ex-Servicemen 139 12 Cooperation Between the Armed Forces and Civil Authorities 153 13 National Cadet Corps 159 14 Defence Cooperaton with Foreign Countries 171 15 Ceremonial and Other Activities 181 16 Activities of Vigilance Units 193 17. Empowerment and Welfare of Women 199 Appendices I Matters Dealt with by the Departments of the Ministry of Defence 205 II Ministers, Chiefs of Staff and Secretaries who were in position from April 1, 2007 onwards 209 III Summary of latest Comptroller & Auditor General (C&AG) Report on the working of Ministry of Defence 210 1 THE SECURITY ENVIRONMENT Troops deployed along the Line of Control 1 s the world continues to shrink and get more and more A interdependent due to globalisation and advent of modern day technologies, peace and development remain the central agenda for India.i 1.1 India’s security environment the deteriorating situation in Pakistan and continued to be infl uenced by developments the continued unrest in Afghanistan and in our immediate neighbourhood where Sri Lanka. Stability and peace in West Asia rising instability remains a matter of deep and the Gulf, which host several million concern. Global attention is shifting to the sub-continent for a variety of reasons, people of Indian origin and which is the ranging from fast track economic growth, primary source of India’s energy supplies, growing population and markets, the is of continuing importance to India. -

Union Defence Services Air Force
Report of the Comptroller and Auditor General of India for the year ended March 2015 Union Government (Defence Services) Air Force No. 18 of 2016 Report No. 18 of 2016 (Air Force) CONTENTS Paragraph Description Page Number Number Preface iii Overview v Glossary ix CHAPTER I: Introduction 1.1 Profile of the audited entities 1 1.2 Authority for audit 2 1.3 Audit methodology and procedure 2 1.4 Defence budget 3 1.5 Budget and expenditure of Indian Air Force 4 1.6 Response to Audit 9 1.7 Recoveries at the instance of Audit 10 CHAPTER-II: Audit of Air HQ Communication 15 Squadron (AHCS) CHAPTER-III: Audit Paragraphs relating to Contract Management 3.1 Acquisition and operation of C-17 Globemaster 25 III aircraft 3.2 Procurement of 14 additional Dornier aircraft 31 3.3 Refurbishment of ‘X’ system 33 CHAPTER-IV: Audit Paragraphs relating to Works Services 4.1 Excess provision of hangars resulting in 39 avoidable expenditure of `24.28 crore i Report No. 18 of 2016 (Air Force) 4.2 Irregularities in drafting tender resulting in 42 excess payment 4.3 Excess provision of 200 seats capacity in an 44 Auditorium 4.4 Avoidable creation of permanent assets at a cost 46 of `1.10 crore CHAPTER-V: Audit Paragraphs on other issues 5.1 In-effective usage of Access Control System 49 5.2 Irregular payment of Transport Allowance 52 5.3 Avoidable expenditure of `131.45 lakh due to 53 payment of Electricity tax 5.4 Avoidable expenditure of ```80.07 lakh on repair 56 of an aero engine ANNEX 59 to 64 Photographs : Courtesy IAF ii Report No. -

The Gazette of India
REGD. N0. D-222 The Gazette of India PUBLISHED BY AUTHORITY No. 38] NEW DELHI, SATURDAY, SEPTEMBER 21, 1963/BHADRA 30, 1885 PART I—SECTION 4 Notifications regarding Appointments, Promotions, Leave, etc. of Officers issued by the Ministry of Defence MINISTRY OF DEFENCE No. 2042, dated 4th Sep. 1963.—Shri Sunil Kumar Khas- MINISTRY OF DEFENCE nobis, offg. Jr. Scientific Officer, Defence Metallurgical Research New Delhi, 21st September 1963 Laboratory, Ichapur relinquished charge of his post on 6th No. 2037, dated 6th Sep. 1963.—The President is pleased July 1963 (AN.) consequent on acceptance of his resignation. to appoint Shri K. Ramanujam, IAS, Under Secy., M. of D. G. JAYARAMAN, Under Secy. as Dy. Secy, in the Ministry, w.e.f. 4th Sep. 1963 (F.N.). YATINDRA SINGH, Under Secy INDIAN ORDNANCE FACTORIES SERVICE No. 2041, dated 6th Sep. 1963.—The President is pleased DEFENCE PRODUCTION ORGANISATION to appoint the following as Assistant Manager (on probn.) No. 2038, dated 1th Sep. 1963.—The President is pleased from the dates noted against each, until further orders :— to make the following promotion : — Shri Vilapakkam Natesapillai Pattabiraman, 16th Nov. 1962. Defence Science Service Shri Sankaran Narayanaswamy, 1st Dec. 1962. Shri Prabudh Kumar Bhasker Prasad MEHTA, permit. Sr. Shri Musuvathy Hananandan Jeyachandran, 11th Dec. 1962. Scientific Asstt., Inspectorate of General Stores, West India, No. 2044, dated 5th Sep. 1963,—The President is pleased BOMBAY to be oftg. Jr. Scientific Officer, Inspectorate of to appoint Shri Laxmi Chand KALIA, offg. Foreman (permt, General Stores, Central India, KANPUR, 13th May 1963 Asstt. Foreman), as offg. Asstt. -

Supplement to the London Gazette, 3 June, 1925. 3775
SUPPLEMENT TO THE LONDON GAZETTE, 3 JUNE, 1925. 3775 Major-General Cecil Francis Romer, C.B., Major D'Arcy John Francis, 23rd (London) G.M.G., Director of Staff Duties, War Armoured Car Company, Territorial Army. Office. •Lieutenant (Temporary Major) Ernest Edward Gawthorn, D.C.M., Postal Section, Royal To- be Commanders of the Military Division of Engineers. the said Most Excellent Order:— Major Cecil Courtney Godwin, The Green Howards. Lieutenant-Colonel and Brevet Colonel Ernest 1 Robinson, O.B.E., T.D., Tyne Electrical Major Harold James Huxford, Sth/Oih Engineers, Territorial Army. Rajputana Rifles (Napiers), Indian Army. Captain Charles Norman Jervelund, The Green Major (Temporary Lieutenant-Colonel) Francis Howards. David Alexander, Inspector of Remounts. Major Edgar Montague Jones, T.D., St\ Colonel William Henniker Anderson, Indian Alban's School Contingent, Officers Training Army. Corps, General List, Territorial Army. Major and Brevet Lieutenant-Colonel Charles Ordnance Executive Officer, 1st Class, and Reginald Barko, T.D., 5th Battalion, The Major John Henry Keyes, M.C., Royal Army North Staffordshire Regiment, Territorial Ordnance Corps. Army, Commanding 3rd Battalion, Iraq Staff Paymaster and Lieutenant-Colonel Levies.. William Shand Mackenzie, Royal Army Pay Colonel James Molesworbh Blair, C.M.G., Corps. D.S.O., Late Military Attache, Belgrade. Major Thomas Moss, 16th Punjab Regiment, Major and Brevet Lieutenant-Colonel (Tem- Indian Army. porary Colonel Commandant) Herbert Major and Brevet Lieutenant-Colonel David Thomas Dobbin, D.S.O., The Duke of Ogilvy, D.S 0 , Royal Engineers. Cornwall's Light Infantry, Commandant, Accountant Officer, 2nd Class, and Lieutenant- Iraq Levies. Colonel Vernon Ivon Robins, Corps of Colonel John Cavendish Freeland, Indian Military Accountants. -

Report of the Comptroller and Auditor General of India for the Year Ended March 2014
Report of the Comptroller and Auditor General of India for the year ended March 2014 Union Government (Defence Services) Air Force No. 38 of 2015 Report of the Comptroller and Auditor General of India for the year ended March 2014 Union Government (Defence Services) Air Force No. 38 of 2015 CONTENTS Paragraph Page Preface iii Overview iv CHAPTER I: INTRODUCTION About the Report 1.1 1 Authority for audit 1.2 2 Planning and conduct of audit 1.3 2 Profile of audited entities 1.4 2 Budget and Expenditure of Air Force 1.5 4 Response to Audit 1.6 7 CHAPTER II: AIR FORCE Operation and maintenance of ‘AA’ 2.1 9 Operational works in IAF 2.2 33 Operation and maintenance of ‘C’ aircraft 2.3 56 Upgradation and maintenance of ‘DD’ aircraft 2.4 67 Inappropriate procurement of tent based medical shelter 2.5 85 Excess procurement of Speech Secrecy equipment 2.6 89 Procurement of Intelligence System 2.7 92 Arbitrary planning in the resurfacing of extended portion of runways 2.8 95 Incorrect procurement of compressor working fluid 2.9 99 Inordinate delay in commissioning of Low Level Transportable Radar 2.10 103 Savings at the instance of Audit 2.11 107 _________________________________________________________________________________________________ i CHAPTER III: DEFENCE RESEARCH AND DEVELOPMENT ORGANISATION (AIR FORCE) Execution of Mission Mode projects and delivery of systems by DRDO 3.1 109 CHAPTER IV: HINDUSTAN AERONAUTICS LIMITED Estate management in Hindustan Aeronautics Limited, Bengaluru 4.1 141 Investment in Joint Venture Companies by Hindustan Aeronautics 4.2 151 Limited Acceptance of contract for DARIN-III with fixed delivery schedule led 4.3 168 to liquidated damages ANNEXURE 172 to 205 _________________________________________________________________________________________________ ii PREFACE This Report for the year ended March 2014 has been prepared for submission to the President under Article 151 of the Constitution. -

The Journal of Parliamentary Information
The Journal of Parliamentary Information VOLUME LVII NO. 1 MARCH 2011 LOK SABHA SECRETARIAT NEW DELHI CBS Publishers & Distributors Pvt. Ltd. 24, Ansari Road, Darya Ganj, New Delhi-2 2009 issue, EDITORIAL BOARD Editor : T.K. Viswanathan Secretary-General Lok Sabha Associate Editor : P.K. Misra Joint Secretary Lok Sabha Secretariat Assistant Editors : Kalpana Sharma Director Lok Sabha Secretariat Pulin B. Bhutia Joint Director Lok Sabha Secretariat Sanjeev Sachdeva Joint Director Lok Sabha Secretariat © Lok Sabha Secretariat, New Delhi for approval. THE JOURNAL OF PARLIAMENTARY INFORMATION VOLUME LVII NO. 1 MARCH 2011 CONTENTS PAGE EDITORIAL NOTE 1 ADDRESSES Inaugural Address by the Speaker, Lok Sabha, Smt. Meira Kumar at the Fourth Conference of CPA India and Asia Regions, Raipur, 25-29 October 2010 3 Address by His Excellency, Mr. Barack H. Obama, President of the United States of America, to members of Parliament 8 PARLIAMENTARY EVENTS AND ACTIVITIES Conferences and Symposia 21 Birth Anniversaries of National Leaders 25 Exchange of Parliamentary Delegations 27 Bureau of Parliamentary Studies and Training 29 PARLIAMENTARY AND CONSTITUTIONAL DEVELOPMENTS 31 SESSIONAL REVIEW Lok Sabha 43 Rajya Sabha 52 State Legislatures 54 RECENT LITERATURE OF PARLIAMENTARY INTEREST 60 APPENDICES I. Statement showing the work transacted during the Sixth Session of the Fifteenth Lok Sabha 64 II. Statement showing the work transacted during the Two Hundred and Twenty-first Session of the Rajya Sabha 70 (iv) III. Statement showing the activities of the Legislatures of the States and Union Territories during the period 1 October to 31 December 2010 75 IV. List of Bills passed by the Houses of Parliament and assented to by the President during the period 1 October to 31 December 2010 82 V. -

Selina John, (NR 18466-L) Wife of Maj
1 AFR Reserved Court No.3 ARMED FORCES TRIBUNAL, REGIONAL BENCH, LUCKNOW TRANSFERRED APPLICATION No. 39 of 2012 Wednesday, this the 2nd day of Mar 2016 Hon’ble Mr. Justice D.P. Singh, Member (J) Hon’ble Air Marshal Anil Chopra, Member (A) Ex Lt (Mrs) Selina John, (NR 18466-L) wife of Maj. Vinod Raghwan R/O 3/379, Vishwas Khand, Gomti Nagar, Lucknow. Petitioner Ld. Counsel for : Maj (Retd) R.D. Singh, the Petitioner Advocate Versus 1. Union of India, through its Secretary, Ministry of Defence, DHQ, PO, New Delhi. 2. Chief of the Army Staff, Army Headquarters, DHQ PO, New Delhi. 3. DGAFMS, Army Headquarters, DHQ, PO, New Delhi. 4. DG (MNS) (AG Branch) Army Headquarters, DHQ PO, New Delhi. 5. Commanding Officer, Military Hospital, Danapore. 6. GOC-in-C through DDMS, Central Command, Lucknow Cantt. Respondents Ld. Counsel for the : Shri D.K. Pandey, Advocate Respondents assisted by Lt Col Subodh Verma, OIC Legal Cell. T.A No. 39 of 2012 Mrs Selina John 2 (Per. Justice Devi Prasad Singh, J.) 1. Petitioner being aggrieved with the order of release from service had preferred a Writ Petition No 967 (S/B) of 1999 in the High Court of Judicature at Allahabad which has been transferred to this Tribunal in pursuance to powers conferred by Section 34 of the Armed Forces Tribunal Act, 2007 and has been re-numbered as T.A. No 39 of 2012. 2. We have heard Ld. Counsel for the parties and perused the records. 3. Substantial question of law involved in the present T.A. -
Master Corrected 27.12.2018
2 0 1 9 15/1, CUBBON ROAD, BANGALORE - 560 091. C O N T E N T S Board of Directors…………………………..………..……………….……VI CORPORATE OFFICE Corporate Office………………..…………………………………………. 1 HAL Management Academy…………………………..…………………15 BANGALORE COMPLEX Office of CEO (BC)………………….…………………………………..…17 Aircraft Division…………………….………………………………………18 LCA Production Group…………………………………………………….21 IJT/LSP Production Group………………………………………………..23 Airport Services Centre…………………………………...………………24 Aerospace Division………………...………………………………………26 Engine Division…………………………..…………………………………29 IMGT Division………………………..……………………………………..32 Medical & Health Unit……………………………………………………..34 Overhaul Division……………………………..………………………..35 Facilities Management Division……………………….………………….38 Foundry &Forge Division………………………………………………….40 DESIGN COMPLEX Director (Engg. and R&D)'s Office..……………………………………42 Aircraft Research & Design Centre………………………….…….43 RWR & DC………………………..…………………………………48 AERDC…..…………………………………………………………………54 MCSR & D C……….………………..………………………………56 Aircraft Upgrade Research & Design Centre, Nasik…………….58 ASERDC, Lucknow…………………………………………………59 SLR & DC, Hyderabad…………………………..…………………60 HELICOPTER COMPLEX Office of CEO (HC)…………………………………………….……61 Helicopter Division……………..……………………………………62 Flight Operations (Rotary Wing)………………………………………….65 Helicopter MRO Division………………………………………...…67 Aerospace Composite Division……………………………………70 Barrackpore Division………………………………………………..71 OTHER IMPORTANT TELEPHONE NUMBERS BANGALORE Welfare and Other Organisations – HAL…………………………73 Govt Organisations & PSUs in Bangalore………………………..74 -
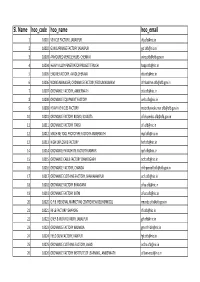
Sl. Name Hoo Code Hoo Name Hoo Email
Sl. Name hoo_code hoo_name hoo_email 1 10001 VEHICLE FACTORY, JABALPUR [email protected] 2 10002 GUN CARRIAGE FACTORY JABALPUR [email protected] 3 10003 ARMOURED VEHICLE HQRS. CHENNAI [email protected] 4 10004 HEAVY ALLOY PENETRATOR PROJECT TIRUCHI [email protected] 5 10005 ENGINE FACTORY, AVADI,CHENNAI [email protected] 6 10006 WORKS MANAGER, ORDNANCE FACTORY,YEDDUMAILARAM [email protected] 7 10007 ORDNANCE FACTORY, AMBERNATH [email protected] 8 10008 ORDNANCE EQUIPMENT FACTORY [email protected] 9 10009 HEAVY VEHICLES FACTORY [email protected] 10 10010 ORDNANCE FACTORY BOARD, KOLKATA [email protected] 11 10011 ORDNANCE FACTORY ITARSI [email protected] 12 10012 MACHINE TOOL PROTOTYPE FACTORY AMBERNATH [email protected] 13 10013 HIGH EXPLOSIVE FACTORY [email protected] 14 10014 ORDNANCE PARACHUTE FACTORY KANPUR [email protected] 15 10015 ORDNANCE CABLE FACTORY CHANDIGARH [email protected] 16 10016 ORDNANCE FACTORY, CHANDA [email protected] 17 10017 ORDNANCE CLOTHING FACTORY, SHAHJAHANPUR [email protected] 18 10018 ORDNANCE FACTORY BHANDARA [email protected] 19 10019 ORDNANCE FACTORY KATNI [email protected] 20 10020 O.F.B. REGIONAL MARKETING CENTRE NEW DELHI(RMCDL) [email protected] 21 10021 RIFLE FACTORY ISHAPORE [email protected] 22 10022 GREY & IRON FOUNDRY, JABALPUR [email protected] 23 10023 ORDNANCE FACTORY NALANDA gm‐ofn‐[email protected] 24 10024 FIELD GUN FACTORY, KANPUR [email protected] 25 10025 ORDNANCE CLOTHING FACTORY, AVADI [email protected] 26 10026 ORDNANCE FACTORY INSTITUTE OF LEARNING , AMBERNATH ofilam‐[email protected] 27 10027 OFB, -

Sainik Covers
2019 16-31 January Vol 66 No 2 ` 5 SAINIK Samachar Indian Army: Nation Before Self pic: DPR Photo Division pic: DPR Photo Division Annual Press Conference of the Chief of the Army Staff, Gen Bipin Rawat on the occasion of Army Day, 2019 at Manekshaw Centre, New Delhi on January 10, 2019 . pic: DPR Photo Division TheAdmiral President, Sunil ShriLanba, Ram CNS Nath receiving Kovind Admiral at the ‘At Christophe Home’ function, Prazuck, organised Chief of on the the Naval occasion Staff, of 72nd IndependenceFrench Navy Day, at South at Rashtrapati Block lawns, Bhavan, New Delhi in New on DelhiJanuary on August7, 2019. 15, 2018. In This Issue Since 1909 Transforming Indian Army into a 4 more Potent and Adaptive Force (Initially published as FAUJI AKHBAR) Vol. 66 q No 2 26 Pausha– 11 Magha 1940 (Saka) 16-31 January 2019 The journal of India’s Armed Forces published every fortnight in thirteen languages including Hindi & English on behalf of Ministry of Defence. It is not necessarily an organ for the expression of the Government’s defence policy. The published items represent the views of respective writers and correspondents. Editor-in-Chief Ruby Thinda Sharma Senior Editor Manoj Tuli Commands of the 8 Vice President 28 Editor Afaque Ahmad Ehsani Indian Army Inaugurates NCC RD… Sub Editors Sub Maj KC Sahu & Sub Maj Baiju G Coordination Kunal Kumar Business Manager Rajpal Our Correspondents DELHI: Col Chiranjeet Konwer (Offg.); Capt DK Sharma VSM; Gp Capt Anupam Banerjee; Divyanshu Kumar; Photo Editor: K Ramesh; BENGALURU: Guru Prasad HL; CHANDIGARH: