Severe Combined Immunodeficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IDF Patient & Family Handbook
Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficiency Diseases This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. FIFTH EDITION COPYRIGHT 1987, 1993, 2001, 2007, 2013 IMMUNE DEFICIENCY FOUNDATION Copyright 2013 by Immune Deficiency Foundation, USA. REPRINT 2015 Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. The Immune Deficiency Foundation Patient & Family Handbook may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA; or by telephone at 800-296-4433. Immune Deficiency Foundation Patient & Family Handbook for Primary Immunodeficency Diseases 5th Edition This publication has been made possible through a generous grant from Baxalta Incorporated Immune Deficiency Foundation 110 West Road, Suite 300 Towson, MD 21204 800-296-4433 www.primaryimmune.org [email protected] EDITORS R. Michael Blaese, MD, Executive Editor Francisco A. Bonilla, MD, PhD Immune Deficiency Foundation Boston Children’s Hospital Towson, MD Boston, MA E. Richard Stiehm, MD M. Elizabeth Younger, CPNP, PhD University of California Los Angeles Johns Hopkins Los Angeles, CA Baltimore, MD CONTRIBUTORS Mark Ballow, MD Joseph Bellanti, MD R. Michael Blaese, MD William Blouin, MSN, ARNP, CPNP State University of New York Georgetown University Hospital Immune Deficiency Foundation Miami Children’s Hospital Buffalo, NY Washington, DC Towson, MD Miami, FL Francisco A. -

Prof.Dr. TÜRKAN PATIROĞLU
Prof.Dr. TÜRKAN PATIROĞLU Kişisel Bilgiler WE-epbo:s that:t pt:u/r/[email protected]/rturkanp/ ETığpitati Yman Bdail gUizlmeranilık, Erciyes Üniversitesi, Dahili Tıp Bil., Çocuk Sağlığı ve Hastalıkları, Türkiye 1998 - 2000 Tıpta UYazmndaanll ıUkz, mEracniylıeks, EÜrnciivyerss Üitnesivi,e Drsaihteilsi iT, Dıpa Bhiilli., TÇıopc Buikl. ,S Çaoğclıuğkı vSea ğHlaığsıt avleık Hlaarsıt, aTlüıkrlkairyı,e T 1ü9r7k7iy e- 11998828 - 1989 Yİnagbiliazcnec, Bı 2D Oilrltea rÜstü Sertifika, Kurs ve Eğitimler Sağlık ve Tıp, DEsesneenyt iHala Cylvinaniclaalr Rı Kesuellaarncıhm & S eGrCtiPfi kfoars ıT, Eriracli yInevse üsntiigvaetrosritse, sIni Hveasytvigaant oDre Anceaydleermi Yye, 2re0l1 E1tik Kurulu, 2008 Yaptığı Tezler STaıpğt.Va eU Hzmsta Andlık, 1, k9r8o2nik enfeksiyonu olan hastalarda glukoz metabolizması, Erciyes Üniversitesi, Tıp Fakültesi, Çocuk ASarğalışk tBırilimmlae rAi, lTaıpn, lDaarhıili Tıp Bilimleri, Çocuk Sağlığı ve Hastalıkları, Pediatrik Hematoloji, Pediatrik İmmünoloji ve Allerji APrkoaf.Ddre.,m Erickiy Uesn Üvnaivnelrasirte /si ,G Töıpr Feavklüeltresi, Çocuk Sağ.Ve Hst Ad, 1995 - Devam Ediyor YDrodç..DDorç., .DErrc.,i yEersc iÜyensiv Üenrsiviteerssii, tTeıspi, FTaıpk üFlateksüil, tÇeosic, uÇko cSuakğ .VSaeğ H.Vset AHdst, 1A9d9, 01 9- 8179 9- 51989 Yönetilen Tezler UPAzmTIaRnOlıĞk,L CU.E TR.,K HAENM(OÖFğrİLeİn Aci )H, A20ST0A6LARINDA F8 GENİ İNT22H BÖLGESİNDEKİ İNVERSİYONUN ARAŞTIRILMASI., Tıpta DPAÜTZIERYOLĞELRUİ VTE., DTİESDSAEMVİİ NETEK İNİNTLRİAĞVİ.,A TSıKptÜaL UEzRm KaOnAlıkG,Ü ML.AKSAYROANK ÜGKELCİÜŞ(TÖİRğrİLenEcNi) H, 2A0Y0V4ANLARDA ADRENOMEDÜLLİN KPARTAINRİOAĞLL RUA TD.,Y UOZTUENR ASPÜİRNEİLNİ EYTAKŞİALYEARNİ, TLıÖpStaE MUzİLmİ aHnAlıSkT, HA.LMAeRhDmAe tE(NÖDğrOeKnRciİ)N, 2F0O0N4KSİYONLARIN DEĞERLENDİRİLMESİ SCI. I, SGSeCneI tvice A AnHalCysIi sİn odf eak Csolehroirnt eo fG 2i7re5n P aDtieerngtisl ewridthe H Yyapyeırn-IlgaEn Saynn Mdraokmaelse laenrd/or Chronic MFruecdoe cNu.,t aRnoejaosu-Rse Cstarnepdoid Ji.,a Csaisballero Garcia de Oteyza A., Buchta M., Huebscher K., Gamez-Diaz L., Proietti M., JSOaUghRaNfAi SL. -

IDF Guide to Hematopoietic Stem Cell Transplantation
Guide to Hematopoietic Stem Cell Transplantation Immune Deficiency Foundation Guide to Hematopoietic Stem Cell Transplantation This publication contains general medical information that cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this publication should not be used as a substitute for professional medical advice. In all cases, patients and caregivers should consult their healthcare providers. Each patient’s condition and treatment are unique. Copyright 2018 by Immune Deficiency Foundation, USA Readers may redistribute this guide to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Immune Deficiency Foundation Guide to Hematopoietic Stem Cell Transplantation may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation (IDF). If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA, or by telephone: 800-296-4433. For more information about IDF, go to: www.primaryimmune.org. This publication has been made possible through the IDF SCID Initiative and the SCID, Angels for Life Foundation. Acknowledgements The Immune Deficiency Foundation would like to thank the organizations and individuals who helped make this publication possible and contributed to the development of the Immune Deficiency Foundation Guide to Hematopoietic Stem -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

Novel Combined Immune Deficiency and Radiation Sensitivity Blended Phenotype in an Adult with Biallelic Variations in ZAP70 and RNF168
CASE REPORT published: 26 May 2017 doi: 10.3389/fimmu.2017.00576 Novel Combined Immune Deficiency and Radiation Sensitivity Blended Phenotype in an Adult with Biallelic Variations in ZAP70 and RNF168 Ivan K. Chinn1,2,3*†, Robert P. Sanders4†, Asbjørg Stray-Pedersen5,6,7, Zeynep H. Coban-Akdemir7,8, Vy Hong-Diep Kim9, Harjit Dadi9,10, Chaim M. Roifman9,10, Troy Quigg4, James R. Lupski1,7,8,11, Jordan S. Orange1,2,3 and I. Celine Hanson1,2 1 Department of Pediatrics, Baylor College of Medicine, Houston, TX, USA, 2 Section of Immunology, Allergy, and Rheumatology, Texas Children’s Hospital, Houston, TX, USA, 3 Center for Human Immunobiology, Texas Children’s Edited by: Hospital, Houston, TX, USA, 4 Texas Transplant Institute, Methodist Hospital, San Antonio, TX, USA, 5 Norwegian National Andrew Gennery, Unit for Newborn Screening, Department of Pediatric and Adolescent Medicine, Oslo University Hospital, Oslo, Norway, Newcastle University, UK 6 Institute of Clinical Medicine, University of Oslo, Oslo, Norway, 7 Baylor-Hopkins Center for Mendelian Genomics, Baylor College of Medicine, Houston, TX, USA, 8 Department of Molecular and Human Genetics, Baylor College of Medicine, Reviewed by: Houston, TX, USA, 9 Division of Immunology and Allergy, Department of Pediatrics, The Hospital for Sick Children, University Filomeen Haerynck, of Toronto, Toronto, ON, Canada, 10 Canadian Centre for Primary Immunodeficiency, The Jeffrey Model Research Laboratory Ghent University, Belgium for the Diagnosis of Primary Immunodeficiency, The Hospital for Sick Children, University of Toronto, Toronto, ON, Canada, Kohsuke Imai, 11 Human Genome Sequencing Center, Baylor College of Medicine, Houston, TX, USA Tokyo Medical and Dental University, Japan *Correspondence: With the advent of high-throughput genomic sequencing techniques, novel genetic Ivan K. -

Host Genetics and Infectious Disease: New Tools, Insights and Translational Opportunities
REVIEWS Host genetics and infectious disease: new tools, insights and translational opportunities Andrew J. Kwok 1, Alex Mentzer 1,2 and Julian C. Knight 1 ✉ Abstract | Understanding how human genetics influence infectious disease susceptibility offers the opportunity for new insights into pathogenesis, potential drug targets, risk stratification, response to therapy and vaccination. As new infectious diseases continue to emerge, together with growing levels of antimicrobial resistance and an increasing awareness of substantial differences between populations in genetic associations, the need for such work is expanding. In this Review, we illustrate how our understanding of the host–pathogen relationship is advancing through holistic approaches, describing current strategies to investigate the role of host genetic variation in established and emerging infections, including COVID-19, the need for wider application to diverse global populations mirroring the burden of disease, the impact of pathogen and vector genetic diversity and a broad array of immune and inflammation phenotypes that can be mapped as traits in health and disease. Insights from study of inborn errors of immunity and multi-omics profiling together with developments in analytical methods are further advancing our knowledge of this important area. Penetrance Disease syndromes caused by infectious agents have A seminal study of adoptees in the 1980s reported 1 The proportion of individuals occurred throughout the history of modern humans . increased risk of death from infectious disease in chil- with a particular genotype As a result of our continued interactions with patho- dren whose biological parents succumbed to an infec- that also has an associated gens, our genomes have been shaped through processes tious disease7, highlighting the significance of human phenotype. -

Blueprint Genetics Severe Combined Immunodeficiency Panel
Severe Combined Immunodeficiency Panel Test code: IM0101 Is a 80 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of combined immunodeficiencies. The genes on this panel are included in the Primary Immunodeficiency Panel. About Severe Combined Immunodeficiency Severe combined immunedeficiencies (SCIDs) are a group of primary immunodeficiencies characterized by specific mutations in genes of T and B-lymphocyte systems and leading to little or no immune response. Different subtypes of SCIDs are characterized and subdivided by the presence of circulating T and B cells. T cells are absent or markedly decreased in the most types, but levels of B cells vary. In addition, both of these disease subgroups (T-B+ and T-B-) can occur with or without NK cells. Patients with SCID are susceptible to recurrent infections that can be fatal. The worldwide prevalence of SCID is estimated to be at least 1:100,000 births, while some genetically more homogenous populations may show markedly increased numbers. Mutations in IL2RG are the most common reason for SCIDs, explaining approximately 50% of all cases and close to 100% of X-linked cases. Availability 4 weeks Gene Set Description Genes in the Severe Combined Immunodeficiency Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ADA Severe combined immunodeficiency due to adenosine deaminase AR 49 93 deficiency AK2 Reticular dysgenesis AR 14 17 ATM Breast cancer, Ataxia-Telangiectasia AD/AR 1047 1109 BCL11B Immunodeficiency -

Patient & Family Handbook
Immune Deficiency Foundation Patient & Family Handbook For Primary Immunodeficiency Diseases This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SIXTH EDITION COPYRIGHT 1987, 1993, 2001, 2007, 2013, 2019 IMMUNE DEFICIENCY FOUNDATION Copyright 2019 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. The Immune Deficiency Foundation Patient & Family Handbook may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from the Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 110 West Road, Suite 300, Towson, MD 21204, USA; or by telephone at 800-296-4433. Immune Deficiency Foundation Patient & Family Handbook For Primary Immunodeficiency Diseases 6th Edition The development of this publication was supported by Shire, now Takeda. 110 West Road, Suite 300 Towson, MD 21204 800.296.4433 www.primaryimmune.org [email protected] Editors Mark Ballow, MD Jennifer Heimall, MD Elena Perez, MD, PhD M. Elizabeth Younger, Executive Editor Children’s Hospital of Philadelphia Allergy Associates of the CRNP, PhD University of South Florida Palm Beaches Johns Hopkins University Jennifer Leiding, -

Primary Immunodeficiency Diseases in Children and Adults
Primary Immunodeficiency Diseases in children and adults Microorganism Primary Immune Deficiency Diseases Disease (PID) Environment Host • Background • Approach to diagnosis of PID • Genetic diagnosis of PID • Lack of focus is good thing • Looks like duck but not a duck Primary Immunodeficiency diseases • Inherited diseases of immune system • Affect different components of the immune system • Clinically heterogeneous Why do we need to diagnose PIDs? • Collective Prevalence of high as 1 in 10000 suggesting a very high burden of disease • Often missed causing significant morbidity and mortality • Multiple family members may get affected leading to financial burden on the family and society • Early diagnosis and adequate management can lead to significant reduction in morbidity and mortality Group Category Group I Combined immunodeficiencies Group II Combined immunodeficiencies with associated or syndromic features. Group III Predominantly antibody deficiencies. Group IV Diseases of immune dysregulation. Group V Congenital defects of phagocyte number, function, or both. Group VI Defects in innate immunity. Group VII Autoinflammatory disorders. Group VIII Complement deficiencies. Group IX Phenocopies of PID • International Union of Immunological Societies (IUIS): • 354 distinct disorders • 344 different gene defects listed (Feb2017) Group I Combined immunodeficiencies Group IV Diseases of immune Group II Combined immunodeficiencies with dysregulation. associated or syndromic features. Group VII Autoinflammatory Group III Predominantly antibody disorders. -

Gastrointestinal Manifestations in Children with Primary Immunodeficiency Diseases
Egypt J Pediatr Allergy Immunol 2017; 15(1):3-8. Review article Gastrointestinal manifestations in children with primary immunodeficiency diseases Shereen M. Reda Professor of Pediatrics, Ain Shams University, Cairo, Egypt Introduction versus-host-disease and veno-occlusive disease post Primary immunodeficiency (PID) diseases are a hematopoietic stem cell transplantation in certain heterogeneous group of rare genetic disorders that PID diseases2,3. affect the development and function of immune This review focuses on the characteristic chronic cells. To date, more than 150 defects have been GI manifestations that are commonly encountered identified and the number is growing. These in some PID diseases (Table 1). disorders are broadly classified into defects affecting the humoral (B cell) immunity, defects of Severe Combined Immunodeficiency (SCID) the cellular (T cell) immunity or both T cell and B SCID is a heterogeneous group of molecular defects cell, neutrophil and macrophage defects, and in both T- cell and B-cell number and function. defects in the innate immunity. The hallmark According to the presence or absence of T cells, B clinical feature is recurrent and/or severe infections. cells and natural killer (NK) cells, this group is However, some type of immune defect may present broadly classified as T-B+NK+, T-B+NK-, T-B- with autoimmune manifestations, and increased risk NK+, and T-B-NK-3. To date, more than 15 genetic of malignancy in association with their underlying mutations result in the SCID phenotype. The mode immunodeficiency1. of inheritance of these mutations is autosomal In PID diseases, the gastrointestinal (GI) tract is recessive (AR) except the defect in the common the second target organ affected after the respiratory gamma chain which is X-linked and is considered tract. -
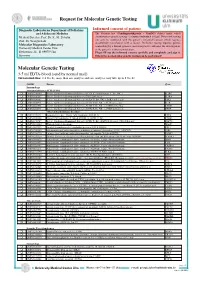
Molecular Genetic Testing
Request for Molecular Genetic Testing Diagnostic Laboratories Department of Pediatrics Informed consent of patient and Adolescent Medicine The German. law (Gendiagnostikgesetz – GenDG) defines under which Medical Director: Prof. Dr. K.-M. Debatin circumstances genetic testing of a human individual is legal. Diagnostic testing Prof. Dr. Georgia Lahr! can only be conducted with the patient’s informed consent which requires documented consultation with a doctor. Predictive testing requires genetic Molecular Diagnostics Laboratory! counselling by a human genetics specialist prior to and after the investigation, University Medical Center Ulm! or the patient’s written renunciation. Eythstrasse 24 - D-89075 Ulm Please fill out the informed consent carefully and completely and sign it. Germany Otherwise no molecular genetic testing can be performed! Molecular Genetic Testing 3-5 ml EDTA-blood (send by normal mail) Turnaround time: 2-4 weeks, more than one analysis and rare analyses may take up to 8 weeks OMIM Disease Gene Immunology Immunodeficiency SCID (T-B+) q OMIM 300400 Severe Combinined Immunodeficiency (SCID, X-chromosomal, T-, B+, NK- ) IL2RG q OMIM 606367 Severe Combinined Immunodeficiency, CD25 deficiency IL2RA q OMIM 600802 Severe Combinined Immunodeficiency (SCID, T-, B+, NK- ), JAK3 deficiency JAK3 q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- B+ NK+ ), IL7R deficiency IL7R q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- B+ NK+ ), CD3D deficiency CD3D q OMIM 608971 Severe Combinined Immunodeficiency (SCID, T- -

Dysregulated Immune System Secondary to Novel Heterozygous Mutation of CIITA Gene Presenting with Recurrent Infections and Syste
Dysregulated immune system secondary to novel heterozygous mutation of CIITA gene presenting with recurrent infections and Systemic lupus erythematosus Aakash Chandran Chidambaram1, Jaikumar Ramamoorthy2, Sriram Krishnamurthy3, Prabhu Manivannan1, and Pediredla Karunakar1 1Jawaharlal Institute of Postgraduate Medical Education and Research 2Jawaharlal Institute of Post Graduate Medical Education 3Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) June 18, 2020 Abstract The expression of Major Histocompatibility Complex (MHC) molecule is essential for homeostasis of the immune system. Tissue-specific expression of MHC-II is regulated at the level of transcription. The master regulator for transcription of the MHC-II gene is CIITA. Homozygous mutations affecting the CIITA gene results in bare lymphocyte syndrome type-II. The clinical manifestations of heterozygous mutations are not well reported. Hence, this case report aims to provide more insight into the clinical features associated with heterozygous mutations of CIITA. We report a 5-year-old child who had presented with recurrent infections in infancy and systemic lupus erythematosus (SLE) in toddler age. Tables: Nil Figures: 2 Abbreviations MHC Major Histocompatibility Complex SLE Systemic lupus erythematosus ELISA Enzyme Linked Immunosorbant Assay HIV Human Immunodeficiency Virus CVID Common Variable Immunodeficiency EULAR/ACR European League Against Rheumatism/American College of Rheumatology HLA Human Leukocyte Antigen NGS Next Generation Sequencing BLS Bare Lymphocyte Syndrome ANA Antinuclear Antibody Abstract The expression of Major Histocompatibility Complex (MHC) molecule is essential for homeostasis of the immune system. Tissue-specific expression of MHC-II is regulated at the level of transcription. The master regulator for transcription of the MHC-II gene is CIITA. Homozygous mutations affecting the CIITA gene results in bare lymphocyte syndrome type-II1.