A Case Report on Delayed Sleep Phase Disorder in an Adolescent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Importance of Healthy Sleep
THE IMPORTANCE OF HEALTHY SLEEP Disorders like Sleep Apnea, Periodic Limb Movement Disorder, Narcolepsy and Insomnia negatively impact your health. It is estimated that Sleep Apnea affects approximately 40 million people, with 90% going undiagnosed. TABLE OF CONTENTS Are you at risk?- Sleep Disorders Questionnaire • Epworth Sleepiness Scale • STOP BANG- Sleep Apnea Screening Questionnaire Sleep Disorders • Sleep Apnea • Narcolepsy • Restless Leg Syndrome/Periodic Limb Movement Disorder • Insomnia • Snoring Testing • Polysomnography • Portable Home Sleep Study • Split night • CPAP titration • MSLT- Multiple Sleep Latency Study • High Resolution Pulse Oximetry Screening Types of Treatment • CPAP • Oral Appliances • Surgical Interventions Sleep Health/Good Sleep Hygiene Sleep Lab at Wayne HealthCare Resources and References 3 DID YOU KNOW? According to the National Heart, Lung, and Blood Institute: • Approximately 42 million American adults suffer from sleep-disordered breathing (SDB) • 1 in 5 adults has mild OSA (Obstructive Sleep Apnea) • 1 in 15 has moderate to severe OSA (75% to 90% of severe SDB cases remain undiagnosed) • 9% of middle-aged women suffer from OSA • 25% of middle-aged men suffer from OSA For more information visit www.nhlbi.nih.gov. Sleep apnea that goes untreated can worsen conditions such as: • Coronary Artery Disease • Hypertension • Atrial Fibrillation • Type-2 Diabetes • Congestive Heart Failure • Obesity • Stroke • Glacoma 4 ARE YOU AT RISK? The Epworth Sleepiness Scale How likely are you to doze off or fall asleep in the following situations in contrast to feeling just tired? This refers to your usual way of life in recent times. Even if you have not done some of these things recently try to work out how they would have affected you. -

2021 Magellan Clinical Guidelines for Medical Necessity Review
National Imaging Associates, Inc.* 2021 Magellan Clinical Guidelines For Medical Necessity Review SLEEP STUDY GUIDELINES Effective January 1, 2021 – December 31, 2021 *National Imaging Associates, Inc. (NIA) is a subsidiary of Magellan Healthcare, Inc. Copyright © 2019-2021 National Imaging Associates, Inc., All Rights Reserved Guidelines for Clinical Review Determination Preamble Magellan is committed to the philosophy of supporting safe and effective treatment for patients. The medical necessity criteria that follow are guidelines for the provision of diagnostic imaging. These criteria are designed to guide both providers and reviewers to the most appropriate diagnostic tests based on a patient’s unique circumstances. In all cases, clinical judgment consistent with the standards of good medical practice will be used when applying the guidelines. Determinations are made based on both the guideline and clinical information provided at the time of the request. It is expected that medical necessity decisions may change as new evidence-based information is provided or based on unique aspects of the patient’s condition. The treating clinician has final authority and responsibility for treatment decisions regarding the care of the patient. 2021 Magellan Clinical Guidelines-SLEEP STUDY 2 Guideline Development Process These medical necessity criteria were developed by Magellan Healthcare for the purpose of making clinical review determinations for requests for therapies and diagnostic procedures. The developers of the criteria sets included representatives from the disciplines of radiology, internal medicine, nursing, cardiology, and other specialty groups. Magellan’s guidelines are reviewed yearly and modified when necessary following a literature search of pertinent and established clinical guidelines and accepted diagnostic imaging practices. -
Evaluating and Managing Sleep Disorders
Evaluating & Managing Sleep Disorders Julia Aziz, M.D. Daniel Lewin, Ph.D., D.ABSM Division of Pediatric Pulmonology and Sleep Medicine Children’s National Health System Washington, D.C. Future of Pediatrics, 2019 Topics • Basics about sleep • Effects of insufficient sleep • Common sleep problems and disorders: signs symptoms and treatment Awake Drowsy Stage 1 Stage 2 Stage 3 Stage REM Hypnogram Sleep Stage Distribution Wake REM Stage 1 Stage 2 Stage 3 Time 2200 2400 200 400 600 800 NonREM Stage 3 is dominant during the first half of night Sleep stage REM is dominant during the second half of night Process S Sleep Homeostatic Process C Circadian Sleep Academic Award, Gerald Rosen Process S Sleep drive Homeostatic Reduced Sleep drive 1st sleep 2nd sleep Process C Circadian Sleep Academic Award, Gerald Rosen Sleep Time and Timing Sleep and Circadian Health Effects • Metabolism regulation and energy expenditure • Physical restoration • Tissue repair • Neuronal recalibration • Memory consolidation The Sleep Habits Assessment Bedtime EDS Awakenings Regularity Snoring (Excessive Daytime Somnolence) .Routine .Hyperactivity .Call outs .Schedule .Volume .Resistance .Irritability .Partial Arousal .Age .Pauses .Fears .Difficulty waking .Restlessness .Periodicity Adapted from: Mindel, JA, & Owens. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. Lippincott, Williams & Wilkins. Philadelpha (2003) Outline I. Evaluating & Managing obstructive sleep apnea (OSA) – Clinical assessment of OSA – Who, when, where and how to -

THE SLEEP CENTER at BACHARACH Treating Sleep Problems in Adults and Children in the Region's Most Advanced
Our sleep center has been designed to make you feel relaxed and comfortable, with amenities you’d find at a luxury hotel: • Flat screen TV in every sleep suite • Extended-tier cable • Individually decorated suites • Private bathroom with shower • Wireless high-speed Internet access THE SLEEP CENTER • Continental breakfast AT BACHARACH • Individual room temperature control 54 West Jimmie Leeds Road Pomona, NJ 08240 Advanced sleep medicine in a luxurious setting The Sleep Center. It’s one more reason we are recommended by our peers. Honored by our profession. Applauded by our patients. The Sleep Center is open Monday–Friday, 8:30 a.m. - 4:30 p.m. Testing is available 24/7. THE SLEEP CENTER AT BACHARACH Treating sleep problems in adults and children in the region’s most advanced (and comfortable) setting. bacharach.org • (609) 748-5405 bacharach.org • (609) 748-5405 THE BACHARACH SLEEP PROBLEMS IN CHILDREN Does the thought of falling SLEEP TEAM CAN HELP In children, a sleep disorder may be the culprit in cases Normal sleep follows a predictable structure, moving of obesity, bedwetting, sleepwalking, nightmares and asleep fill you with worry? in stages from drowsiness to deep sleep. Sleep disorders difficulty in school. Bacharach is proud to be the only disrupt this cycle, robbing your body of the rest it needs pediatric sleep center in the region. Do you spend your nights to function. But don’t despair, our Sleep Center is fully equipped to diagnose sleep problems with a variety of A PLAN THAT WILL snoring or gasping for testing options. LET YOU REST EASY First, you’ll meet with a physician — board-certified in The sleep team brings together advanced diagnostic tools breath? Do you awake Sleep Medicine — who will perform a physical exam and and years of experience to develop a care plan that’s take a comprehensive history. -
WHO Technical Meeting on Sleep and Health
WHO technical meeting on sleep and health Bonn Germany, 22-24 January 2004 World Health Organization Regional Office for Europe European Centre for Environment and Health Bonn Office ABSTRACT Twenty-one world experts on sleep medicine and epidemiologists met to review the effects on health of disturbed sleep. Invited experts reviewed the state of the art in sleep parameters, sleep medicine and, long-term effects on health of disturbed sleep in order to define a position on the secondary and long- term effects of noise on sleep for adults, children and other risk groups. This report gives definitions of normal sleep, of indicators of disturbance (arousals, awakenings, sleep deficiency and fragmentation); it describes the main sleep pathologies and disorders and recommends that when evaluating the health impact of chronic long-term sleep disturbance caused by noise exposure, a useful model is the health impact of chronic insomnia. Keywords SLEEP ENVIRONMENTAL HEALTH NOISE Address requests about publications of the WHO Regional Office to: • by e-mail [email protected] (for copies of publications) [email protected] (for permission to reproduce them) [email protected] (for permission to translate them) • by post Publications WHO Regional Office for Europe Scherfigsvej 8 DK-2100 Copenhagen Ø, Denmark © World Health Organization 2004 All rights reserved. The Regional Office for Europe of the World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Sleep Services: Sleep Study, Insomnia
Sleep Services: Sleep Study, Insomnia POLICY INITIATED: 06/30/2019 MOST RECENT REVIEW: 06/30/2019 POLICY # HH-4826 Overview Statement The purpose of these clinical guidelines is to assist healthcare professionals in selecting the medical service that may be appropriate and supported by evidence to improve patient outcomes. These clinical guidelines neither preempt clinical judgment of trained professionals nor advise anyone on how to practice medicine. The healthcare professionals are responsible for all clinical decisions based on their assessment. These clinical guidelines do not provide authorization, certification, explanation of benefits, or guarantee of payment, nor do they substitute for, or constitute, medical advice. Federal and State law, as well as member benefit contract language, including definitions and specific contract provisions/exclusions, take precedence over clinical guidelines and must be considered first when determining eligibility for coverage. All final determinations on coverage and payment are the responsibility of the health plan. Nothing contained within this document can be interpreted to mean otherwise. Medical information is constantly evolving, and HealthHelp reserves the right to review and update these clinical guidelines periodically. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, or otherwise, without permission from HealthHelp. All trademarks, product names, logos, and brand names are the -

Understanding Your Sleep Study Results
UNDERSTANDING YOUR SLEEP STUDY RESULTS Lights Out/Lights On Times – “Lights Out” means the time that the lights are first turned out and you are attempting to sleep. The time that the study ends is termed “Lights On”. At this time, you are awakened, the lights are turned on and the study is over. TRT (Total Recording Time) – Total time of study from “lights out” to “lights on”. TST (Total Sleep Time) – Total time asleep after lights out. Sleep Latency- How long it takes you to fall asleep after “lights out”. 15-20 minutes is a normal sleep latency. A shorter sleep latency could mean you are sleep-deprived and/or have a sleep disorder. WASO (Wake after Sleep Onset) – This is the total amount of time that you spend awake during the night after you first fall asleep. Being awake during the night affects your sleep quality and is often associated with some type of sleep disorder. Stages of Sleep: During sleep, you cycle between Non-REM (NREM) and REM Sleep (4 total stages). You should move through NREM and REM several times throughout the night and each stage of sleep is important to your overall health. Obstructive Sleep Apnea can cause some of these stages to be shortened or absent. NREM sleep (Non-REM sleep): There are 3 stages –each stage is deeper than the last. Stage N1 (NREM 1) - The first stage of sleep. This is the transition from awake to asleep. During this time, your breathing becomes more regular and your heart rate begins to slow down, but you can be easily awakened. -
Attended Polysomnography for Evaluation of Sleep Disorders
UnitedHealthcare® Commercial Medical Policy Attended Polysomnography for Evaluation of Sleep Disorders Policy Number: 2021T0334GG Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policies Coverage Rationale ....................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Documentation Requirements ...................................................... 3 Supplies and Repairs/ Replacements Definitions ...................................................................................... 3 • Obstructive Sleep Apnea Treatment Applicable Codes .......................................................................... 7 Description of Services ................................................................. 7 Community Plan Policy Clinical Evidence ........................................................................... 9 • Attended Polysomnography for Evaluation of Sleep U.S. Food and Drug Administration ........................................... 14 Disorders References ................................................................................... 14 Medicare Advantage Coverage Summary Policy History/Revision Information ........................................... 16 • Sleep Apnea: Diagnosis and Treatment Instructions for Use ..................................................................... 16 Coverage Rationale Home Sleep Apnea Testing Home Sleep Apnea Testing (HSAT), using a portable monitor, is medically necessary for evaluating -

Shift-Work Disorder
SUPPLEMENT TO Support for the publication of this supplement was provided by Cephalon, Inc. It has been edited and peer reviewed by The Journal of Family Practice. Available at jfponline.com VOL 59, NO 1 / JANUARY 2010 Shift-work disorder The social and economic burden of shift-work disorder } Larry Culpepper, MD, MPH The characterization and pathology of circadian rhythm sleep disorders } Christopher L. Drake, PhD Recognition of shift-work disorder in primary care } Jonathan R. L. Schwartz, MD Managing the patient with shift-work disorder } Michael J. Thorpy, MD Disclosures Dr Culpepper reports that he serves as a con- sultant to AstraZeneca, Eli Lilly and Company, Shift-work disorder Pfizer Inc, Wyeth, sanofi-aventis, and Takeda Pharmaceuticals North America, Inc, and on the speakers bureau of Wyeth. CONTENts AND FACUltY Dr Drake reports that he has received research support from Cephalon, Inc., Takeda Pharma- ceuticals North America, Inc, and Zeo, Inc., and has served on the speakers bureaus of The social and economic Cephalon, Inc., and as a consultant to sanofi- aventis. burden of shift-work disorder ......................... S3 Dr Schwartz reports that he serves as a Larry Culpepper, MD, MPH consultant to and on the speakers bureaus of Department of Family Medicine AstraZeneca, Boehringer Ingelheim Phar- Boston University Medical Center maceuticals, Inc., Cephalon, Inc., Pfizer Inc, Boston, Massachusetts Sepracor Inc., Takeda Pharmaceuticals North America, Inc, and GlaxoSmithKline. Dr Thorpy reports that he serves as a The characterization and pathology consultant to and on the speakers bureaus of Cephalon, Inc., and Jazz Pharmaceuticals, Inc. of circadian rhythm sleep disorders ......... S12 Christopher L. -

Sleep Studies)
PRINT-FRIENDLY VERSION FACT SHEET PROVIDER COMPLIANCE TIPS FOR POLYSOMNOGRAPHY (SLEEP STUDIES) UPDATES • Replaced the earlier year’s data with 2019 • Updated the Background section • Updated “Reasons for Denials” INTRODUCTION This publication is meant to educate providers on coverage and proper billing for polysomnography (sleep studies). Page 1 of 3 ICN MLN4013531 August 2020 Provider Compliance Tips for Polysomnography (Sleep Studies) MLN Fact Sheet PROVIDER TYPES AFFECTED Physicians and other practitioners who write prescriptions for polysomnography. BACKGROUND In a study done by the Office of the Inspector General (OIG), U.S. Department of Health and Human Services, published in June of 2019, it was found that from January 1, 2014 through December 31, 2015, MACs nation- wide paid freestanding facilities, facilities affiliated with hospitals, and physicians approximately $800 million for selected polysomnography (a type of sleep study to diagnose and evaluate sleep disorders) services. REASONS FOR DENIALS Previous OIG reviews for polysomnography services found that Medicare paid for services that did not meet Medicare requirements. These reviews identified payments for services with inappropriate diagnosis codes, without the required supporting documentation, and to providers that exhibited patterns of questionable billing. Through their audit, the OIG estimated that Medicare made overpayments of $269 million for polysomnography services during the audit period. These errors occurred because the CMS oversight of polysomnography services was insufficient to ensure that providers complied with Medicare requirements and to prevent payment of claims that didn’t meet those requirements. DOCUMENTATION REQUIREMENTS CMS requires an order from the provider who treats the beneficiary for all diagnostic tests, including polysomnography. -
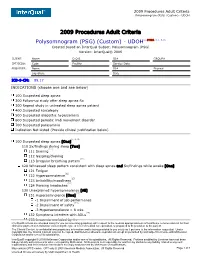
Polysomnogram (PSG) (Custom) - UDOH
2009 Procedures Adult Criteria Polysomnogram (PSG) (Custom) - UDOH 2009 Procedures Adult Criteria Polysomnogram (PSG) (Custom) - UDOH(1, 2*MDR, 3, 4, 5, 6) Created based on InterQual Subset: Polysomnogram (PSG) Version: InterQual® 2009 CLIENT: Name D.O.B. ID# GROUP# CPT/ICD9: Code Facility Service Date PROVIDER: Name ID# Phone# Signature Date ICD-9-CM: 89.17 INDICATIONS (choose one and see below) 100 Suspected sleep apnea 200 Follow-up study after sleep apnea Rx 300 Repeat study in untreated sleep apnea patient 400 Suspected narcolepsy 500 Suspected idiopathic hypersomnia 600 Suspected periodic limb movement disorder 700 Suspected parasomnia Indication Not Listed (Provide clinical justification below) (7, 8, 9) 100 Suspected sleep apnea [One] 110 Sx/findings during sleep [Two] (10) 111 Snoring 112 Gasping/choking (11) 113 Irregular breathing pattern 120 Witnessed sleep pattern consistent with sleep apnea and Sx/findings while awake [One] 121 Fatigue (12) 122 Hypersomnolence (13) 123 Irritability/moodiness (14) 124 Morning headaches 130 Unexplained hypersomnolence [All] (12) 131 Hypersomnolence [One] -1 Impairment of job performance (15) -2 Impairment of safety -3 Hypersomnolence > 8 wks (16) 132 Symptoms interfere with ADLs 133 Insomnia excluded by Hx InterQual® criteria are intended solely for use as screening guidelines with respect to the medical appropriateness of healthcare services and not for final clinical or payment determination concerning the type or level of medical care provided, or proposed to be provided, to the patient. The Clinical Content is confidential and proprietary information and is being provided to you solely as it pertains to the information requested. Under copyright law, the Clinical Content may not be copied, distributed or otherwise reproduced except as permitted by and subject to license with McKesson Corporation and/or one of its subsidiaries. -

Helpful Hints for Filing Polysomnography and Home Sleep Testing (HST) for Diagnosing Obstructive Sleep Apnea (OSA)
Helpful hints for filing Polysomnography and Home Sleep Testing (HST) for diagnosing obstructive sleep apnea (OSA) Mary Coughlin RN, MS, NNP, Global Clinical Services Managers, Children’s Medical Ventures Sleep tests must include sleep staging, which is defined to include a Coverage of a PAP device for the treatment of OSA is 1-4 lead electroencephalogram (EEG), electrooculogram limited to claims where the diagnosis of OSA is based (EOG), submental electromyogram (EMG) and upon a Medicare-covered sleep test (Type I, II, III, or IV). electrocardiogram (ECG). It must also include at least the A Medicare-covered sleep test must be either a following additional parameters of sleep: polysomnogram performed in a facility-based laboratory • Airflow (Type I study) or a home sleep test (HST) (Types II, III, or • Respiratory effort IV).The test must be ordered by the beneficiary’s treating • Oxygen saturation by oximetry physician and conducted by an entity that qualifies as a • Performed as either a whole night study for diagnosis Medicare provider of sleep tests and is in compliance with only or a split night study to diagnose and initially all applicable state regulatory requirements. evaluate treatment Facility-based sleep test Home Sleep Test (HST) A Type I sleep test is the continuous and simultaneous A HST is performed unattended in the beneficiary’s home monitoring and recording of various physiological and using a portable monitoring device.A portable monitoring pathophysiological parameters of sleep with physician device for conducting