DA-Dexa-Vs-PDN-En-PTI.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Slip Op. 21-97 UNITED STATES COURT of INTERNATIONAL
Case 1:20-cv-00058-TMR Document 43 Filed 08/05/21 Page 1 of 57 Slip Op. 21-97 UNITED STATES COURT OF INTERNATIONAL TRADE HEZE HUAYI CHEMICAL CO., LTD. AND JUANCHENG KANGTAI CHEMICAL CO., LTD., Plaintiffs, v. Before: Timothy M. Reif, Judge UNITED STATES, Court No. 20-00058 Defendant, BIO-LAB, INC., CLEARON CORP. AND OCCIDENTAL CHEMICAL CORPORATION, Defendant-Intervenors. OPINION [Final Determination sustained.] Dated: August 5, 2021 Gregory S. Menegaz, deKieffer & Horgan PLLC, of Washington, DC, argued for plaintiffs Heze Huayi Chemical Co. and Juancheng Kangtai Chemical Co. With him on the brief were Alexandra H. Salzman and James K. Horgan. Sonia M. Orfield, Trial Attorney, Commercial Litigation Branch, Civil Division, U.S. Department of Justice, of Washington, DC, argued for the defendant United States. Of counsel on the brief was Jesus N. Saenz, Attorney, Office of Chief Counsel for Trade Enforcement and Compliance, U.S. Department of Commerce, of Washington, DC. James R. Cannon, Jr., Cassidy Levy Kent (USA) LLP, of Washington, DC, argued for defendant-intervenors Bio-Lab, Inc., Clearon Corporation and Occidental Chemical Corporation. With him on the brief were Jonathan M. Zielinski and Ulrika Kristin Skitarelic Swanson. Case 1:20-cv-00058-TMR Document 43 Filed 08/05/21 Page 2 of 57 Court No. 20-00058 Page 2 Reif, Judge: This action arises from a challenge by plaintiffs, Heze Huayi Chemical Co., Ltd. (“Heze Huayi”) and Juancheng Kangtai Chemical Co., Ltd. (“Kangtai,” and, collectively, “plaintiffs”) to certain aspects of the final results of an administrative review of the antidumping duty order covering chlorinated isocyanurates (“chlorinated isos”) published by the Department of Commerce (“Commerce”) in the Federal Register on June 20, 2016.1 See Chlorinated Isocyanurates from the People’s Republic of China, 85 Fed. -

Annual Report of Shandong Hi-Speed Co. Ltd. of 2020
Annual Report 2020 Company Code: 600350 Abbreviation of Company: Shangdong Hi-Speed Annual Report of Shandong Hi-Speed Co. Ltd. of 2020 1/265 Annual Report 2020 Notes I. The Board of Directors, Board of Supervisors, directors, supervisors and executives of the Company guarantee the truthfulness, accuracy and completeness without any false or misleading statements or material omissions herein, and shall bear joint and several legal liabilities. II. Absent directors Post of absent director Name of absent director Reason for absence Name of delegate Independent Director Fan Yuejin Because of work Wei Jian III. Shinewing Certified Public Accountants (Special Partnership) has issued an unqualified auditor's report for the Company. IV. Mr. Sai Zhiyi, the head of the Company, Mr. Lyu Sizhong, Chief Accountant who is in charge of accounting affairs, Mr. Zhou Liang, and Chen Fang (accountant in charge) from ShineWing declared to guarantee the truthfulness, accuracy and completeness of the annual report. V. With respect to the profit distribution plan or common reserves capitalizing plan during the reporting period reviewed by the Board of Directors After being audited by Shinewing Certified Public Accountants (Special Partnership), the net profit attributable to owners of the parent company in 2020 after consolidation is CNY 2,038,999,018.13, where: the net profit achieved by the parent company is CNY2,242,060,666.99. After withdrawing the statutory reserves of CNY224,206,066.70 at a ratio of 10% of the achieved net profit of the parent company, the retained earnings is 2,017,854,600.29 . The accumulated distributable profits of parent company in 2020 is CNY16,232,090,812.89. -

JINAN YIPIN CORPORATION, LTD. and SHANDONG HEZE INTERNATIONAL TRADE and DEVELOPING COMPANY
Slip Op. 09-70 UNITED STATES COURT OF INTERNATIONAL TRADE JINAN YIPIN CORPORATION, LTD. and SHANDONG HEZE INTERNATIONAL TRADE AND DEVELOPING COMPANY, Plaintiffs, v. UNITED STATES, Before: Timothy C. Stanceu, Judge Defendant, Consol. Court No. 04-00240 and FRESH GARLIC PRODUCERS ASSOCIATION, CHRISTOPHER RANCH, L.L.C., THE GARLIC COMPANY, VALLEY GARLIC, and VESSEY AND COMPANY, INC., Defendant-Intervenors. OPINION AND ORDER [Affirming in part and remanding the United States Department of Commerce’s remand redetermination in an administrative review of an antidumping duty order on fresh garlic from China] Dated: July 2, 2009 Grunfeld, Desiderio, Lebowitz, Silverman & Klestadt LLP (Bruce M. Mitchell and Mark E. Pardo) for plaintiff Jinan Yipin Corporation, Ltd. Lee & Xiao (Yingchao Xiao) for plaintiff Shandong Heze International Trade and Developing Company. Tony West, Assistant Attorney General, Jeanne E. Davidson, Director, Reginald T. Blades, Jr., Assistant Director, Patricia M. McCarthy, Assistant Director, Commercial Litigation Branch, Civil Division, United States Department of Justice (Richard P. Schroeder and Mark T. Pittman); Evangeline D. Keenan, Scott D. McBride, and Amanda L. Blaurock, Office of Chief Consol. Court No. 04-00240 Page 2 Counsel for Import Administration, United States Department of Commerce, of counsel, for defendant. Kelley Drye & Warren LLP (Michael J. Coursey and John M. Herrmann) for defendant- intervenors Fresh Garlic Producers Association, Christopher Ranch, L.L.C., The Garlic Company, Valley Garlic, and Vessey and Company, Inc. Stanceu, Judge: Before the court is the redetermination made by the International Trade Administration, United States Department of Commerce (“Commerce” or the “Department”) in response to the court’s remand order in Jinan Yipin Corp. -

1 3700/03264 Yantai Taiyuan Foods Co., Ltd. 莱阳 Laiyang Shandongprovince PP 22 A
企业地址 Address No. Approval No. Establishment name / Activities Remarks Town/city Province/Region/State 1 3700/03264 Yantai Taiyuan Foods Co., Ltd. 莱阳 laiyang ShandongProvince PP 22 A Qingdao Chia Tai Co.,Ltd. 2 3700/03291 Qingdao City ShandongProvince PP 22 A Food Processing Plant Shandong Fengxiang - L.D.C. Co. 3 3700/03347 - Liaochen City ShandongProvince PP 22 A Ltd. Meat Product Processing Workshop 4 3700/03355 Weifang City ShandongProvince PP 22 A Of Weifang Legang Food Co.,Ltd. SHANDONG RIYING FOOD 5 3700/03371 zaozhuang ShandongProvince PP 22 A CO.,LTD Anqiu Foreign Trade Foods Co. Ltd. No.2 Processing Workshop Of 6 3700/03392 Weifang City ShandongProvince PP 22 A Heat-Processed Poultry Meat And Its Products No.2 Meat Product Processing 7 3700/03408 Workshop Of Shandong Weifang Weifang City ShandongProvince PP 22 A Meicheng Broiler Co.Ltd. Meat Product Processing Workshop 8 3700/03409 Weifang City ShandongProvince PP 22 A Of Shandong Delicate Food Co.,Ltd. Qingdao Nine-Alliance Group 9 3700/03414 Co.,Ltd. Fucun Cooked Food Qingdao City ShandongProvince PP 22 A Processing Plant Meat Products Processing Factory 10 3700/03431 Weifang City ShandongProvince PP 22 A Of Weifang Jinhe Food Co.,Ltd. No.2 Meat Products Processing Plant 11 3700/03435 Weifang City ShandongProvince PP 22 A Of Weifang Legang Food Co.,Ltd. 12 3700/03439 Qingyun Ruifeng Food Co., Ltd. Dezhou City ShandongProvince PP 22 A Qingdao Nine-alliance Group 13 3700/03447 Qingdao City ShandongProvince PP 22 A Co.,Ltd Changguang Food Plant 14 3700/03450 Yanzhou Lvyuan Food Co., Ltd Yanzhou ShandongProvince PP 22 A 15 3700/03457 Heze Huayun Food Co., Ltd. -

ABSTRACT “The First City to Enjoy the Sunshine with the Sunrise”, Hence the Name Rizhao
ABSTRACT “The first city to enjoy the sunshine with the sunrise”, hence the name Rizhao. Located in the southern end of Shandong Peninsula, neighbouring Qingdao in the north, and facing Japan and Korea across the Yellow Sea in the east, Rizhao is a rising city with unique oceanic features. It covers a total area of 5,310 square kilometers with a population of 2.84 million of which 560,000 live in urban areas. Rizhao possesses the clearest blue sky, blue sea and golden sand beach in China’s eastern coastal areas. Rizhao was upgraded from a county to a city in 1989. At the beginning, the city faced many problems such as weak comprehensive strength, lagged planning, insufficient infrastructure facilities, inappropriate ecological protection in the coastal areas and poor living conditions of the residents. Accelerating urbanization and industrialization intensely competed with the protection of the ecological environment. After the city was upgraded, starting from the view of sustainable development for a future city and aiming at the goal of building an ecological and livable city, we worked out the strategy of “Building an Eco-City” and a series of planning including the Eco-City Building Plan of Rizhao and General Plan for Developing Circular Economy in Rizhao. We began to vigorously carry out practices on eco-city building; improve urban infrastructure; restore damaged ecological area; actively develop circular economy; popularize the utilization of cleaning energies; set up a multi-level housing security system so as to maintain the environmental advantages of “blue sky, blue sea and golden beach” and realize the balanced development between economy, society and ecological environment. -
For Personal Use Only Use Personal For
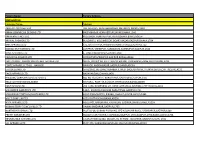
13 July 2012 Norton Rose Australia ABN 32 720 868 049 By e-Lodgement Level 15, RACV Tower 485 Bourke Street Company Announcements MELBOURNE VIC 3000 Australian Securities Exchange Limited AUSTRALIA Level 2 120 King Street Tel +61 3 8686 6000 MELBOURNE VIC 3000 Fax +61 3 8686 6505 GPO Box 4592, Melbourne VIC 3001 DX 445 Melbourne nortonrose.com Direct line +61 3 8686 6710 Our reference Email 2781952 [email protected] Dear Sir/Madam Form 604 – Notice of change of interests of substantial shareholder We act for Linyi Mining Group Co., Ltd. (Linyi), a wholly owned subsidiary of Shandong Energy Group Co., Ltd. (Shandong Energy), in relation to its off-market takeover bid for all of the ordinary shares in Rocklands Richfield Limited ABN 82 057 121 749 (RCI) (Offer) on the terms and conditions set out in Linyi’s bidder’s statement dated 7 June 2012. On behalf of Linyi, Shandong Energy and their related bodies corporate, we enclose a notice of change of interests of substantial shareholder (Form 604) in respect of RCI. A copy of the enclosed Form 604 is being provided to RCI today. Yours faithfully James Stewart Partner Norton Rose Australia Encl. For personal use only APAC-#15206384-v1 Norton Rose Australia is a law firm as defined in the Legal Profession Acts of the Australian states and territory in which it practises. Norton Rose Australia together with Norton Rose LLP, Norton Rose Canada LLP, Norton Rose South Africa (incorporated as Deneys Reitz Inc) and their respective affiliates constitute Norton Rose Group, an international legal practice with offices worldwide, details of which, with certain regulatory information, are at nortonrose.com 604 page 2/2 15 July 2001 Form 604 Corporations Act 2001 Section 671B Notice of change of interests of substantial holder To Company Name/Scheme Rocklands Richfield Limited (RCI) ACN/ARSN ACN 057 121 749 1. -

Assessments of Land Subsidence Along Rizhao-Lankao High-Speed
1 Assessments of land subsidence along Rizhao-Lankao High-speed Railway at Heze, 2 China between 2015 and 2019 with Sentinel-1 data 3 4 Chuanguang Zhu1, Wenhao Wu1, Mahdi Motagh2,3, Liya Zhang1, Zongli Jiang1, and Sichun Long1 5 1Key Laboratory of Coal Resources Clean-utilization & Mine Environment Protection of Hunan Province, Hunan university 6 of Science & Technology, Xiangtan 411201, China 7 2Section of Remote Sensing and Geoinformatics at GFZ German Research Centre for Geosciences in Potsdam, Germany 8 3Institute of Photogrammetry and Geoinformation at Leibniz University Hannover (LUH) in Hannover, Germany 9 10 Correspondence to: Chuanguang Zhu ([email protected]) 11 12 Abstract. The Heze section of Rizhao-Lankao High-speed Railway (RLHR-HZ) has been under 13 construction since 2018 and will be operative by the end of 2021. However, there is a concern that land 14 subsidence in Heze region may affect the regular operation of RLHR-HZ. In this study, we investigate the 15 contemporary ground deformation in the region between 2015 and 2019 by using more than 350 C-band 16 interferograms constructed from two tracks of Sentine-1 data over the region. The Small Baselines Subset 17 (SBAS) technique is adopted to compile the time series displacement. We find that the RLHR-HZ runs 18 through two main subsidence areas: One is located east of Heze region with rates ranging from -4 cm/yr to 19 -1 cm/yr, and another one is located in the coalfield with rates ranging from -8 cm/yr to -2 cm/yr. A total 20 length of 35 km of RLSR-HZ is affected by the two subsidence basins. -
Factory Name
Factory Name Factory Address BANGLADESH Company Name Address AKH ECO APPARELS LTD 495, BALITHA, SHAH BELISHWER, DHAMRAI, DHAKA-1800 AMAN GRAPHICS & DESIGNS LTD NAZIMNAGAR HEMAYETPUR,SAVAR,DHAKA,1340 AMAN KNITTINGS LTD KULASHUR, HEMAYETPUR,SAVAR,DHAKA,BANGLADESH ARRIVAL FASHION LTD BUILDING 1, KOLOMESSOR, BOARD BAZAR,GAZIPUR,DHAKA,1704 BHIS APPARELS LTD 671, DATTA PARA, HOSSAIN MARKET,TONGI,GAZIPUR,1712 BONIAN KNIT FASHION LTD LATIFPUR, SHREEPUR, SARDAGONI,KASHIMPUR,GAZIPUR,1346 BOVS APPARELS LTD BORKAN,1, JAMUR MONIPURMUCHIPARA,DHAKA,1340 HOTAPARA, MIRZAPUR UNION, PS : CASSIOPEA FASHION LTD JOYDEVPUR,MIRZAPUR,GAZIPUR,BANGLADESH CHITTAGONG FASHION SPECIALISED TEXTILES LTD NO 26, ROAD # 04, CHITTAGONG EXPORT PROCESSING ZONE,CHITTAGONG,4223 CORTZ APPARELS LTD (1) - NAWJOR NAWJOR, KADDA BAZAR,GAZIPUR,BANGLADESH ETTADE JEANS LTD A-127-131,135-138,142-145,B-501-503,1670/2091, BUILDING NUMBER 3, WEST BSCIC SHOLASHAHAR, HOSIERY IND. ATURAR ESTATE, DEPOT,CHITTAGONG,4211 SHASAN,FATULLAH, FAKIR APPARELS LTD NARAYANGANJ,DHAKA,1400 HAESONG CORPORATION LTD. UNIT-2 NO, NO HIZAL HATI, BAROI PARA, KALIAKOIR,GAZIPUR,1705 HELA CLOTHING BANGLADESH SECTOR:1, PLOT: 53,54,66,67,CHITTAGONG,BANGLADESH KDS FASHION LTD 253 / 254, NASIRABAD I/A, AMIN JUTE MILLS, BAYEZID, CHITTAGONG,4211 MAJUMDER GARMENTS LTD. 113/1, MUDAFA PASCHIM PARA,TONGI,GAZIPUR,1711 MILLENNIUM TEXTILES (SOUTHERN) LTD PLOTBARA #RANGAMATIA, 29-32, SECTOR ZIRABO, # 3, EXPORT ASHULIA,SAVAR,DHAKA,1341 PROCESSING ZONE, CHITTAGONG- MULTI SHAF LIMITED 4223,CHITTAGONG,BANGLADESH NAFA APPARELS LTD HIJOLHATI, -

Shop Direct Factory List Dec 17
FTE No. Factory Name Factory Address Country Sector % M workers (BSQ) BAISHIQING CLOTHING First and Second Area, Donghaian Industrial Zone, Shenhu Town, Jinjiang China CHINA Garments 148 35% (UNITED) ZHUCHENG TIANYAO GARMENTS CO., LTD Zangkejia Road, Textile & Garment Industrial Park, Longdu Subdistrict, Zhucheng City, Shandong Province, China CHINA Garments 332 19% ABHIASMI INTERNATIONAL PVT. LTD Plot No. 186, Sector 25 Part II, Huda, Panipat-132103, Haryana India INDIA Home Textiles 336 94% ABHITEX INTERNATIONAL Pasina Kalan, GT Road Painpat, 132103, Panipat, Haryana, India INDIA Homewares 435 99% ABLE JEWELLERY MFG. LTD Flat A9, West Lianbang Industrial District, Yu Shan xi Road, Panyu, Guangdong Province, China CHINA Jewellery 178 40% ABLE JEWELLERY MFG. LTD Flat A9, West Lianbang Industrial District, Yu Shan xi Road, Panyu, Guangdong Province, China HONG KONG Jewellery 178 40% AFROZE BEDDING UNIT LA-7, Block 22, Federal B Area, Karachi, Pakistan PAKISTAN Home Textiles 980 97% AFROZE TOWEL UNIT Plot No. C-8, Scheme 33, S. I. T.E, Karachi, Sindh, Pakistan PAKISTAN Home Textiles 960 97% AGEME TEKSTIL KONFEKSIYON INS LTD STI (1) Sari Hamazli Mah, 47083 Sok No. 3/2A, Seyhan, Adana, Turkey TURKEY Garments 350 41% AGRA PRODUCTS LTD Plot 94, 99 NSEZ, Phase 2, Noida 201305, U. P., India INDIA Jewellery 377 100% AIRSPRUNG BEDS LTD Canal Road, Canal Road Industrial Estate, Trowbridge, Wiltshire, BA14 8RQ, United Kingdom UK Furniture 398 83% AKH ECO APPARELS LTD 495 Balitha, Shah Belishwer, Dhaamrai, Dhaka, Bangladesh BANGLADESH Garments 5305 56% AL RAHIM Plot A-188, Site Nooriabad, Pakistan PAKISTAN Home Textiles 1350 100% AL-KARAM TEXTILE MILLS PVT LTD Ht-11, Landhi Industrial Area, Karachi. -

Annual Report (A Joint Stock Limited Company Incorporated in the People’S Republic of China with Limited Liability) (A Joint Stock Limited Company Incorporated
(a joint stock limited company incorporated in the People’s Republic of China with limited liability) 2014 Annual Report Annual Report 2014 Important Notice The Board, Supervisory Committee and the Directors, Supervisors and senior management of the Company warrant the authenticity, accuracy and completeness of the information contained in the annual report and there are no any misrepresentations, misleading statements contained in or material omissions from the annual report for which they shall assume joint and several responsibilities. The 2014 Annual Report of Yanzhou Coal Mining Company Limited has been approved by the seventh meeting of the sixth session of the Board. All ten directors attended the meeting. The seventh meeting of the sixth session of the Board of the Company approved the 2014 profit distribution plan, which allowed the Company to distribute an aggregate cash dividends of RMB98.368 million (tax inclusive) to the Shareholders, representing a dividend of RMB0.02 per share (tax inclusive). There was no appropriation of funds of the Company by the Controlling Shareholder or its subsidiaries for non-operational activities. There were no guarantees granted to external parties by the Company without complying with the prescribed decision-making procedures. Mr. Li Xiyong, Chairman of the Board, Mr. Wu Yuxiang, Chief Financial Officer, and Mr. Zhao Qingchun, Assistant General Manager and Head of Finance Management Department, hereby warrant the authenticity and completeness of the financial statements contained in this annual report. The forward-looking statements contained in this annual report regarding the Company’s future plans do not constitute any substantive commitment to investors and investors are reminded of the investment risks and to exercise caution in their investment. -

Distribution, Genetic Diversity and Population Structure of Aegilops Tauschii Coss. in Major Whea
Supplementary materials Title: Distribution, Genetic Diversity and Population Structure of Aegilops tauschii Coss. in Major Wheat Growing Regions in China Table S1. The geographic locations of 192 Aegilops tauschii Coss. populations used in the genetic diversity analysis. Population Location code Qianyuan Village Kongzhongguo Town Yancheng County Luohe City 1 Henan Privince Guandao Village Houzhen Town Liantian County Weinan City Shaanxi 2 Province Bawang Village Gushi Town Linwei County Weinan City Shaanxi Prov- 3 ince Su Village Jinchengban Town Hancheng County Weinan City Shaanxi 4 Province Dongwu Village Wenkou Town Daiyue County Taian City Shandong 5 Privince Shiwu Village Liuwang Town Ningyang County Taian City Shandong 6 Privince Hongmiao Village Chengguan Town Renping County Liaocheng City 7 Shandong Province Xiwang Village Liangjia Town Henjin County Yuncheng City Shanxi 8 Province Xiqu Village Gujiao Town Xinjiang County Yuncheng City Shanxi 9 Province Shishi Village Ganting Town Hongtong County Linfen City Shanxi 10 Province 11 Xin Village Sansi Town Nanhe County Xingtai City Hebei Province Beichangbao Village Caohe Town Xushui County Baoding City Hebei 12 Province Nanguan Village Longyao Town Longyap County Xingtai City Hebei 13 Province Didi Village Longyao Town Longyao County Xingtai City Hebei Prov- 14 ince 15 Beixingzhuang Town Xingtai County Xingtai City Hebei Province Donghan Village Heyang Town Nanhe County Xingtai City Hebei Prov- 16 ince 17 Yan Village Luyi Town Guantao County Handan City Hebei Province Shanqiao Village Liucun Town Yaodu District Linfen City Shanxi Prov- 18 ince Sabxiaoying Village Huqiao Town Hui County Xingxiang City Henan 19 Province 20 Fanzhong Village Gaosi Town Xiangcheng City Henan Province Agriculture 2021, 11, 311. -

Minimum Wage Standards in China August 11, 2020
Minimum Wage Standards in China August 11, 2020 Contents Heilongjiang ................................................................................................................................................. 3 Jilin ............................................................................................................................................................... 3 Liaoning ........................................................................................................................................................ 4 Inner Mongolia Autonomous Region ........................................................................................................... 7 Beijing......................................................................................................................................................... 10 Hebei ........................................................................................................................................................... 11 Henan .......................................................................................................................................................... 13 Shandong .................................................................................................................................................... 14 Shanxi ......................................................................................................................................................... 16 Shaanxi ......................................................................................................................................................