AGENDA Part 1 1.0 INTRODUCTION
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Buses from Finchley South 326 Barnet N20 Spires Shopping Centre Barnet Church BARNET High Barnet
Buses from Finchley South 326 Barnet N20 Spires Shopping Centre Barnet Church BARNET High Barnet Barnet Underhill Hail & Ride section Great North Road Dollis Valley Way Barnet Odeon New Barnet Great North Road New Barnet Dinsdale Gardens East Barnet Sainsburys Longmore Avenue Route finder Great North Road Lyonsdown Road Whetstone High Road Whetstone Day buses *ULIÀQ for Totteridge & Whetstone Bus route Towards Bus stops Totteridge & Whetstone North Finchley High Road Totteridge Lane Hail & Ride section 82 North Finchley c d TOTTERIDGE Longland Drive 82 Woodside Park 460 Victoria a l Northiam N13 Woodside i j k Sussex Ring North Finchley 143 Archway Tally Ho Corner West Finchley Ballards Lane Brent Cross e f g l Woodberry Grove Ballards Lane 326 Barnet i j k Nether Street Granville Road NORTH FINCHLEY Ballards Lane Brent Cross e f g l Essex Park Finchley Central Ballards Lane North Finchley c d Regents Park Road Long Lane 460 The yellow tinted area includes every Dollis Park bus stop up to about one-and-a-half Regents Park Road Long Lane Willesden a l miles from Finchley South. Main stops Ballards Lane Hendon Lane Long Lane are shown in the white area outside. Vines Avenue Night buses Squires Lane HE ND Long Lane ON A Bus route Towards Bus stops VE GR k SP ST. MARY’S A EN VENUE A C V Hail & Ride section E E j L R HILL l C Avenue D L Manor View Aldwych a l R N13 CYPRUS AVENUE H House T e E R N f O Grounds East Finchley East End Road A W S m L E c d B A East End Road Cemetery Trinity Avenue North Finchley N I ` ST B E O d NT D R D O WINDSOR -

London Golders Green Finchley Road
On the Instructions of TSB Bank LEASEHOLD AVAILABLE LONDON, 762 Finchley Road, Golders Green NW11 7TH Location The available property occupies a position on the eastern side of Finchley Road between Golders Green and Temple Fortune, approximately 6 miles north of Central London within Zone 3 of the London Underground network. Nearby occupiers include a Mercedes Benz car garage with Waitrose, M&S Simply Food, WH Smith and Boots all situated to the north in Temple Fortune. A street traders plan is on the reverse of these particulars. Description The property comprises a former Banking Hall accommodation over ground floor only, providing the following net approximate area: Accommodation Viewing Ground Floor 164 sq m 1,769 sq ft By appointment via this office: Total 164 sq m 1, 769 sq ft Matt Gillson Tenure t: + 44 20 7182 2103 m: + 44 7769 202 757 The property is held on a lease due to expire on 19th February 2022. The e: [email protected] lease includes a break clause in favour of the tenant and a final rent review on 19 th February 2019. CBRE Limited The lease is granted inside the Security of Tenure provisions of the Henrietta House, Henrietta Place Landlord and Tenant Act 1954. London W1G 0NB Terms www.cbre.co.uk/retail Date of Issue 27-Mar-2017 Assignment of TSB’s existing lease. Alternatively, the property may be available on a new lease. Terms to be agreed. Rent £27,500 per annum. Rates We are verbally informed by the Local Rating Authority that the Draft 2017 Rateable Value of the shop is £45,500 and the rates payable are £22,613.50 pa. -

SHABBAT SHALOM: the WARMTH of JEWISH CARE WORLD WAR ONE for FRIENDS and SUPPORTERS of CENTENARY ISSUE Contents
ISSUE 72 | WINTER 2014/5775 SHABBAT SHALOM: THE WARMTH OF JEWISH CARE WORLD WAR ONE FOR FRIENDS AND SUPPORTERS OF CENTENARY ISSUE Contents News and features Editorial enquiries: 020 8922 2809 News in photos ............................................................................................................................................3 Email: [email protected] Ask us a question Common helpline questions..........................................................10 Editor Joy Sable Wars and remembrance Looking back to the war years......................................................12 Design & production by Home front food Tasty meals to cook ..................................................................................14 Jewish Care’s in-house design studio to keep costs to a minimum. Shabbat shalom Jewish Care’s celebrations ................................................................16 Cover photo Hardy perennial A survivor’s story..........................................................................................17 Megan Taylor Pictures at an exhibition A special museum ......................................................................................18 The cover shows Jewish Care client Fay Armstrong with staff Our valuable volunteers Giving your time to help us..............................................................20 member Santa Jogeeah Legacies Making it count ............................................................................................22 Contributing writers Natalie Kennard, Simon -

Stunning One Bedroom Apartment with Unique Charters Finished with Exquisite Design and Taste
Stunning one bedroom apartment with unique charters finished with exquisite design and taste. Temple Fortune Lane, London, NW11 £450 pw (£1,950 pcm) plus fees apply, Furnished, Part Furnished, Unfurnished Available from 23.09.2020 • Amazing Dome shaped reception room • Great location right next to the high-street • Brand new build • Fully fitted bespoke German kitchen • Modern styling and well thought design Local Information Set in the heart of Temple Fortune, the property benefits from the large high street moments away from the properties doorstep. Amenities include restaurants, cafes, supermarkets including Waitrose and Marks and Spencer's and boutique shopping. You are also a short walk away from Golders Green Underground Station (Northern Line) and multiple bus routes leading to Finchley and the West end. The Heath extension is also very close by as is Brent Cross. About this property This impressive well-proportioned and contemporary apartment. Arranged on the 3rd floor, the property benefits from, lots of natural light, brand new appliances throughout and a unique domed ceiling. The property comprises of 1 double bedroom with fully fitted bespoke bedroom storage, a study, underfloor heating, double glazing throughout, utility room, intercom entry system, a fully fitted kitchen, beautiful bathroom and a circular reception room with a domed roof. The property has rain sensor windows, Neff appliances throughout, fitted with a Bespoke German made kitchen. Permission for residential parking. Furnishing Furnished, Part Furnished, Unfurnished Local Authority London Borough of Barnet Council Tax Band = Council Tax Energy Performance EPC Rating = B Viewing All viewings will be accompanied and are strictly by prior arrangement through Savills Hampstead Lettings Office. -

Lgoc ('General') Bus Routes
LGOC (‘GENERAL’) BUS ROUTES ROUTE 2. NORTH FINCHLEY (SWAN & PYRAMIDS) – CATFORD via Golders Green station, Finchley Road, Park Lane, Victoria, Vauxhall, Brixton, Herne Hill, West Norwood, Crystal Palace, Sydenham Introduced 16 February 1913 Extended weekday peak hours to Arnos Grove Station via High Road, Oakleigh Road North, Oakleigh Road South On Mondays – Saturdays route ran in two sections North Finchley – Norwood and Golders Green – Catford Withdrawn between Golders Green Station and Arnos Grove Station 12 February 1946 ROUTE 29B. NORTH FINCHLEY (SWAN & PYRAMIDS) – VICTORIA via Woodhouse Road, Friern Barnet Road, Bounds Green Road, Wood Green, Green Lanes, Seven Sisters Road, Camden Road, Charing Cross Road Introduced 12 September 1923 Withdrawn 29 November 1924 Route renumbered 129 from 1 December 1924 Last day of operation 8 April 1930 ROUTE 34. WHETSTONE (THE GRIFFIN) – STRATFORD BROADWAY via Oakleigh Road North, Oakleigh Road South, Arnos Grove, Palmers Green, Edmonton, North Circular Road, Walthamstow, Leyton High Road, Crownfield Road, Maryland Point Introduced 3 October 1934 ROUTE 43. FRIERN BARNET (ORANGE TREE) – LONDON BRIDGE STATION via Hampden Road, Muswell Hill Broadway, Highgate Archway, Kingsdown Road, Angel Islington Introduced 7 December 1921 ROUTE 43A. COLNEY HATCH LANE (WILTON ROAD) – LONDON BRIDGE STATION via Muswell Hill Broadway, Fortis Green, East Finchley, Highgate, Holloway, Highbury, Islington, Moorgate Introduced 7 December 1914 (up to then it had only run as far as Muswell Hill) Last day of operation 21 March 1937 Friern Barnet & District Local History Society ROUTE 43B. ARKLEY HOTEL – SOUTH CROYDON (SWAN & SUGAR LOAF) via Wood Street, High Barnet, Barnet Hill, Great North Road, Whetstone, North Finchley, East Finchley, Highgate Archway, Holloway, Islington, City Road, Moorgate, Bank, London Bridge, Elephant & Castle, Kennington, Brixton, Streatham, Norbury, Croydon Sundays only Introduced 1 December 1924 Last day of operation 30 September 1934 ROUTE 43C. -

Trolleybus Routes
TROLLEYBUS ROUTES ROUTE 517. NORTH FINCHLEY – HOLBORN CIRCUS via East Finchley, Archway Road, Highgate Archway, Holloway, Caledonian Road, King’s Cross, Gray’s Inn Road (on northbound journeys via Farringdon Road) ROUTE 617. NORTH FINCHLEY – HOLBORN CIRCUS via East Finchley, Archway Road, Highgate Archway, Holloway, Caledonian Road, King’s Cross, Farringdon Road (on northbound journeys via Gray’s Inn Road) Introduced Monday 7 March 1938. Replaced tram route 17 (Archway – Farringdon Street) Journey time 43 minutes, frequency every 3-6 minutes Operated by Finchley Depot Last day of operation Tuesday 31 Jan 1961 Replaced by bus route 17 ROUTE 521. NORTH FINCHLEY – HOLBORN CIRCUS via New Southgate, Bounds Green Station, Wood Green Station, Turnpike Lane Station, Green Lanes, Manor House Station, Finsbury Park Station, Holloway Road, Nag’s Head, Caledonian Road, King’s Cross, Gray’s Inn Road (on northbound journeys via Farringdon Road) ROUTE 621. NORTH FINCHLEY – HOLBORN CIRCUS via New Southgate, Bounds Green Station, Wood Green Station, Turnpike Lane Station, Green Lanes, Manor House Station, Finsbury Park Station, Holloway Road, Nag’s Head, Caledonian Road, King’s Cross, Farringdon Road (on northbound journeys via Gray’s Inn Road) Introduced Sunday 6 March 1938. Replaced tram route 21 Journey time 55 minutes, frequency every 3-6 minutes Operated by Finchley Depot Last day of operation Tuesday 7 November 1961 Replaced by bus route 221 ROUTE 609. BARNET CHURCH - MOORGATE via Whetstone, North Finchley, East Finchley Station, Highgate Archway, Holloway Nag’s Head, Highbury, Islington, Angel, City Road Introduced Sunday 6 March 1938. Replaced tram route 9 Journey time 59 minutes, frequency every 4-8 minutes Operated by Finchley Depot and Holloway/Highgate Depots Last day of operation Tuesday 7 November 1961 Replaced by bus route 104 Friern Barnet & District Local History Society ROUTE 645. -

Uniform List 2015 Belmont Mill Hill Preparatory School •
Belmont Mill Hill Preparatory School Boys Clothes List 2015 – 2016 = only available from School outfitters Anorak (navy) (regulation) Plain dark coat Year 8 only School Blazer (regulation) Shorts (mid grey) Lower School (optional) Trousers (charcoal) Upper School (regulation) Pullover (regulation) Socks (dark grey/black) Best shirt (white) Best tie (regulation) Tie (plain blue) Upper School (regulation) Shirts (light blue, long sleeved) Lower School (regulation) Shirts (grey) Upper School Shoes, black, plain leather, laced up (not loafers). Lower School shoes may have Velcro fastening Cagoule (plain navy) (regulation) Rucksack (plain black) Scarf (optional) (regulation) Scarf - plain dark colour Year 8 only (optional) Sports Kit Lower School Swimming Trunks ‘Speedo’ style, navy or navy quick dry ‘boxer’ style (regulation) Upper School Swimming Shorts – navy quick dry ‘boxer’ style with mesh inner - gym short length (regulation) Sports towel & shower gel (compulsory) Polo Shirt (House colours) (regulation) Gym shorts (navy) (regulation) Rugby shorts (navy) (regulation) Rugby jersey (regulation) Track top Years 3 - 8 (regulation) Track bottoms Years 3 – 8 (regulation) Games socks (navy) (regulation) Socks (short white) (2 pairs) Trainers (mainly white) - for indoor use Trainers (mainly white) - for outdoor use Football boots - Velcro football boots are recommended for Yr 3 –4 for safety and ease of use School sports bag (with or without wheels) (regulation) Swimming bag (regulation) Shin pads/Football Mouth guard/Rugby Large Nametapes Uniform List 2015 Summer Term only Short sleeved shirt with crest (blue) all years (regulation) Cricket sweater (trimmed) Years 5,6,7,8 (regulation) Cricket shirt Years 5,6,7,8 Cricket trousers Years 5,6,7,8 Protective box White trainers Regulation Summer/Winter hats are available from the School Office Notes on Uniform for Boys & Girls The School Outfitters are: Howard Bros. -

Tram Services
TRAM SERVICES Services were provided by Metropolitan Electric Tramways (MET). From 1 July 1933 they were taken over by London Passenger Transport Board (LPTB) and thereafter carried the fleet name ‘London Transport’ NO NUMBER. HIGHGATE (ARCHWAY BRIDGE) – WHETSTONE via Archway Road, North Finchley • Introduced Wednesday 7 June 1905 • Extended to Archway Tavern on Friday 22 December 1905 • Extended to Barnet County Boundary on Saturday 4 August 1906 • Extended to Barnet Church on Thursday 28 March 1907 • Service numbered 38 from 1913 NO NUMBER. NORTH FINCHLEY – FINSBURY PARK via Friern Barnet Road, New Southgate Station, Bounds Green Road, Wood Green, Turnpike Lane, Manor House • Introduced Thursday 8 April 1909 • Service numbered 34 in 1913 NO NUMBER. NORTH FINCHLEY – GOLDERS GREEN via Ballards Lane, Finchley Church End, Temple Fortune • Introduced Thursday 16 December 1909 • Extended to Cricklewood Broadway via Cricklewood Lane on Monday 21 February 1910 • Service numbered 46 in 1912 SERVICE 9. BARNET CHURCH - MOORGATE via Finchley Church End, East Finchley Station, Archway Road, Archway Tavern, Holloway Road, Nag’s Head, Highbury Station, Upper Street, Cross Street, Islington Angel, Canal Bridge, City Road, Old Street • Introduced Thursday 24 September 1914 • Journey time 50 minutes, frequency every 8 minutes • Joint service operated by both MET and LCC cars • Curtailed at North Finchley on Tuesday 1 December 1914 • Last day of operation Saturday 5 March 1938 • Replaced by trolleybus route 609 Friern Barnet & District Local History Society -

London Finchley Road 802 Temple Fortune
On the Instruction of Barclays Bank LEASEHOLD INTEREST ONLY LONDON, 802 Finchley Road, Temple Fortune, NW11 6XJ Location Temple Fortune, situated in North West London, is close to Hendon and Mill Hill, both affluent areas of London. The subject property is located within the central pitch of Finchley Road, the main shopping street in Temple Fortune, which comprises of both local and national retailers, including Costa, WH Smith, Boots, Waitrose and M&S . Description The property is ground floor only, comprising of ancillary space formerly occupied by a local optician. Accommodation Ground Floor 55.93 sq m 602 sq ft Total 55.93 sq m 60 2 sq ft Tenure KEY FEATURES • Prominent Location The property is available on a new sub-lease. Terms available on request. • Sub -lease only available Rent Available on request. Viewing By appointment via this office: Rates Adam Caplan We are verbally informed by the Local Rating Authority that the current t: + 44 20 7182 2650 m: + 44 77530 300 982 Rateable Value for the whole building is £56,000 and the rates payable are e: [email protected] £27,608 pa. The UBR for 2018/2019 is 49.3p. Interested parties are advised to make their own enquiries with the Local Authority for verification purposes. CBRE Limited Henrietta House, Henrietta Place EPC London W1G 0NB www.cbre.co.uk/retail An EPC can be made available upon request. Date of Issue 12-Sept-2018 On the Instruction of Barclays Bank LEASEHOLD INTEREST ONLY LONDON, 802 Finchley Road, Temple Fortune, NW11 6XJ Not to scale. -

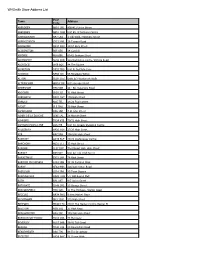
Abbey View Mill Hill London U a Abbots Gardens East Finchley
Street Name Locality Town Road Class Adoption Status Part Adoption Comments Abbey View Mill Hill London U A Abbots Gardens East Finchley London U A Footpath From Abbots Gardens to Deansway East Finchley London U A Footpath From Abbots Gardens to Brim Hill East Finchley London U A Abbots Road Burnt Oak Edgware U A Abbotts Road New Barnet Barnet U A Abercorn Close Mill Hill London U A Abercorn Road Mill Hill London U A Aberdare Gardens Mill Hill London U A Abingdon Road Finchley London U A Accommodation Road Golders Green London U U Acklington Drive Colindale London U A Acton Walk Whetstone London U U Footpath from Acklington Drive to Valiant Walk Colindale London U U Footpath From Acklington Drive side of No12 to Valiant Path Colindale London U A Ada Close New Southgate London U U Adam Close Mill Hill London U U Adams Close Finchley London U U Addington Drive North Finchley London U A Addison Way Golders Green London U A Footpath from Addison Way to Littlewood Open Space Golders Green London U A Adrian Avenue Cricklewood London U U Adrian Close Underhill Barnet U U Aerodrome Road Colindale London U A Footpath from Aerodrome Road to Colindeep Lane Colindale London U A Aeroville Colindale London U U Agnesfield Close North Finchley London U A Agnesfield Close Private Part North Finchley London U U Aitken Road Underhill Barnet U A Footpath from Aitken Road to Well Road Underhill Barnet U A Ajax Avenue Colindale London U A Alan Drive Underhill Barnet U A Alba Gardens Golders Green London U A Albemarle Road East Barnet Barnet U A Alberon Gardens -
Whsmith Store Address List
WHSmith Store Address List Post Town Address Code ABERDEEN AB10 1PD 408/412 Union Street ABERDEEN AB10 1HW Unit E5, St Nicholas Centre ABERGAVENNY NP7 5AG 1 Cibi Walk, Frogmore Street ABERYSTWYTH SY23 2AB 36 Terrace Road ABINGDON OX14 3QX 13/14 Bury Street ACCRINGTON BB5 1EX 14 Cornhill AIRDRIE ML6 6BU 60-62 Graham Street ALDERSHOT GU11 1DB 12a Wellington centre, Victoria Road ALDRIDGE WS9 8QS 44 The Square ALFRETON DE55 7BQ Unit B, Institute Lane ALNWICK NE66 1JD 56 Bondgate Within ALTON GU34 1HZ Units 6/7 Westbrook Walk ALTRINCHAM WA14 1SF 8/12 George Street AMERSHAM HP6 5DR 48 - 50, Sycamore Road ANDOVER SP10 1LJ 31 High Street ARBROATH DD11 1HY 196 High Street ARNOLD NG5 7EL 24/26 Front Street ASCOT SL5 7HG 39 High Street ASHBOURNE DE6 1GH 4 St John Street ASHBY DE LA ZOUCHE LE65 1AL 28 Market Street ASHFORD TN24 8TB 70/72 High Street ASHTON-UNDER-LYNE OL6 7JE Unit 30, Arcade Shopping Centre AYLESBURY HP20 1SH 27/29 High Street AYR KA7 1RH 198/200 High Street BANBURY OX16 5UE 23/24 Castle Quay Centre BANCHORY AB31 5TJ 33 High Street BANGOR LL57 1NY The Market Hall, High Street BARNET EN5 5XY Unit 22 111 High Street BARNSTAPLE EX31 1HP 76 High Street BARROW-IN-FURNESS LA14 1DB 38-42 Portland Walk BARRY CF63 4HH 126/128 Holton Road BASILDON SS14 1BA 29 Town Square BASINGSTOKE RG21 7AW 5/7 Old Basing Mall BATH BA1 1RT 6/7 Union Street BATHGATE EH48 1PG 23 George Street BEACONSFIELD HP9 1QD 11 The Highway, Station Road BECCLES NR34 9HQ 9 New Market Place BECKENHAM BR3 1EW 172 High Street BEDFORD MK40 1TG 29/31 The Harpur Centre, Harpur -

Buses from Golders Green Golders from Buses WEMBLEY Sudbury &Harrowsudbury Road North Wembley
Buses from Golders Green 102 North Finchley 460 Edmonton Green Route finder Edgware Bus Station 13 Bus Station 240 N5 Finchley Central Upper Edmonton Angel Corner for H3 Silver Street Bus route Towards Bus stops Hale Lane FINCHLEY Ossulton Way 13 North Finchley μ¨ Regents Park Road Brookland Hill Brim Hill North Middlesex Hospital Hendon Lane Hilltop Victoria ¬√ Mill Hill Broadway Regents Park Road Hail & Ride Alperton Palmers Green 83 ˙∑ 183 East End Road section East End Road Pinner East Finchley North Circular Road 102 Brent Cross Shopping Centre ø√ Regents Park Road Falloden Way Burnt Oak Falloden Way High Road Daws Lane Mountfield Road Hail & Ride section Midholm Bounds Green Edmonton Green G Beaufort Drive μ¨ North Harrow MILL HILL Regents Park Road Muswell Hill 139 Waterloo ƒ¬ Allandale Avenue Falloden Way Lyttelton Road Brookland Rise Market Broadway Hammers Lane Blandford Close 183 Pinner ˙∑ Henlys Corner Place Harrow Bus Station for East Finchley Harrow-on-the-Hill 210 Brent Cross Shopping Centre ˚∑ Northway HAMPSTEAD Kingsley Way Lyttelton Road The Ridgeway Finchley Road Thornton Way Market Place Belvedere Court Finsbury Park Δ† Harrow Addison Way HARROW Northway GARDEN The Bishops Avenue Town Centre Kingsley Way 226 Ealing Broadway [ ø Central Square Aylmer Road Finchley Road Linden Lea SUBURB 240 Edgware ∫∑ Northwick Park Mill Hill East Childs Way Asmuns Hill for University of Westminster, Linden Lea Finchley Road Erskine Hill The Bishops Avenue 245 Alperton [¬ Harrow campus H2 H2 Lyttelton Road Temple Fortune Lane Willifield