Artificial Nutrition and Hydration for Persons in a State with Disorders of Consciousness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Locker Next 2 Mine
THE LOCKER NEXT 2 MINE __________________________ A full-length drama by Jonathan Dorf This script is for evaluation only. It may not be printed, photocopied or distributed digitally under any circumstances. Possession of this file does not grant the right to perform this play or any portion of it, or to use it for classroom study. www.youthplays.com [email protected] 424-703-5315 The Locker Next 2 Mine © 2013 Jonathan Dorf All rights reserved. ISBN 978-1-62088-412-6. Caution: This play is fully protected under the copyright laws of the United States of America, Canada, the British Commonwealth and all other countries of the copyright union and is subject to royalty for all performances including but not limited to professional, amateur, charity and classroom whether admission is charged or presented free of charge. Reservation of Rights: This play is the property of the author and all rights for its use are strictly reserved and must be licensed by his representative, YouthPLAYS. This prohibition of unauthorized professional and amateur stage presentations extends also to motion pictures, recitation, lecturing, public reading, radio broadcasting, television, video and the rights of adaptation or translation into non-English languages. Performance Licensing and Royalty Payments: Amateur and stock performance rights are administered exclusively by YouthPLAYS. No amateur, stock or educational theatre groups or individuals may perform this play without securing authorization and royalty arrangements in advance from YouthPLAYS. Required royalty fees for performing this play are available online at www.YouthPLAYS.com. Royalty fees are subject to change without notice. Required royalties must be paid each time this play is performed and may not be transferred to any other performance entity. -
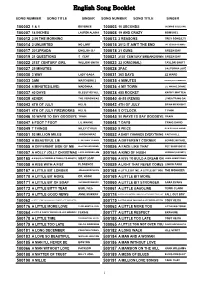
English Song Booklet
English Song Booklet SONG NUMBER SONG TITLE SINGER SONG NUMBER SONG TITLE SINGER 100002 1 & 1 BEYONCE 100003 10 SECONDS JAZMINE SULLIVAN 100007 18 INCHES LAUREN ALAINA 100008 19 AND CRAZY BOMSHEL 100012 2 IN THE MORNING 100013 2 REASONS TREY SONGZ,TI 100014 2 UNLIMITED NO LIMIT 100015 2012 IT AIN'T THE END JAY SEAN,NICKI MINAJ 100017 2012PRADA ENGLISH DJ 100018 21 GUNS GREEN DAY 100019 21 QUESTIONS 5 CENT 100021 21ST CENTURY BREAKDOWN GREEN DAY 100022 21ST CENTURY GIRL WILLOW SMITH 100023 22 (ORIGINAL) TAYLOR SWIFT 100027 25 MINUTES 100028 2PAC CALIFORNIA LOVE 100030 3 WAY LADY GAGA 100031 365 DAYS ZZ WARD 100033 3AM MATCHBOX 2 100035 4 MINUTES MADONNA,JUSTIN TIMBERLAKE 100034 4 MINUTES(LIVE) MADONNA 100036 4 MY TOWN LIL WAYNE,DRAKE 100037 40 DAYS BLESSTHEFALL 100038 455 ROCKET KATHY MATTEA 100039 4EVER THE VERONICAS 100040 4H55 (REMIX) LYNDA TRANG DAI 100043 4TH OF JULY KELIS 100042 4TH OF JULY BRIAN MCKNIGHT 100041 4TH OF JULY FIREWORKS KELIS 100044 5 O'CLOCK T PAIN 100046 50 WAYS TO SAY GOODBYE TRAIN 100045 50 WAYS TO SAY GOODBYE TRAIN 100047 6 FOOT 7 FOOT LIL WAYNE 100048 7 DAYS CRAIG DAVID 100049 7 THINGS MILEY CYRUS 100050 9 PIECE RICK ROSS,LIL WAYNE 100051 93 MILLION MILES JASON MRAZ 100052 A BABY CHANGES EVERYTHING FAITH HILL 100053 A BEAUTIFUL LIE 3 SECONDS TO MARS 100054 A DIFFERENT CORNER GEORGE MICHAEL 100055 A DIFFERENT SIDE OF ME ALLSTAR WEEKEND 100056 A FACE LIKE THAT PET SHOP BOYS 100057 A HOLLY JOLLY CHRISTMAS LADY ANTEBELLUM 500164 A KIND OF HUSH HERMAN'S HERMITS 500165 A KISS IS A TERRIBLE THING (TO WASTE) MEAT LOAF 500166 A KISS TO BUILD A DREAM ON LOUIS ARMSTRONG 100058 A KISS WITH A FIST FLORENCE 100059 A LIGHT THAT NEVER COMES LINKIN PARK 500167 A LITTLE BIT LONGER JONAS BROTHERS 500168 A LITTLE BIT ME, A LITTLE BIT YOU THE MONKEES 500170 A LITTLE BIT MORE DR. -
![Planurile De Viitor Ale Studen]Ilor Se Bat Cap În](https://docslib.b-cdn.net/cover/3287/planurile-de-viitor-ale-studen-ilor-se-bat-cap-%C3%AEn-1113287.webp)
Planurile De Viitor Ale Studen]Ilor Se Bat Cap În
După trei ani în bătaia raidurilor aeriene M\rturia unei românce care a învins Îţi port portul, dar tu nu te legi de ceea ce am învăţat eu în r\zboiul din Siria ” să cred.| PAGINILE 8-9 www.opiniastudenteasca.ro/opiniaveche telefon: (0746) 230 032 e‐mail:[email protected] EDITORIAL Universităţi vs. piaţa muncii (I) Discuția despre absolvenții de facultăți și piața muncii e un subiect nesfîrșit de dezbateri îmbibate de clișee și prejudecăți. Electrocutează pe toată lumea cu sentimente de revoltă și scepti- cism, în virtutea unor opinii insur mon ta - bile despre „cum ar trebui să stea lucru - rile”. Deși încă nu se știe care ar trebui să fie natura relației stat-Minister-universități- studenți-absolvenți-piața-muncii-particulari- stat. Dacă e liniară sau dacă e un șir de bucle întortocheate. Dacă ar trebui să fie l Anul XLII l 25 noiembrie - 1 decembrie 2013 l IAȘI l Nr. 469 l GRATUIT l 5000 de exemplare l apare lunea rigidă sau flexibilă. Însă, fiecare dintre părțile implicate manifestă nemulțumiri profund deznădăjduite. Universitățile ar vrea să rămînă în turnul de fildeș (să insufle valori și maniere de gîndire), dar studenții le cer să coboare Planurile de viitor ale studen]ilor de acolo și să dea mîna cu partenerii eco - no mici, cîtă vreme beneficiază de sprijin finan ciar de la stat. Studenții ar dori ca o facultate să le asigure un loc de muncă se bat cap în cap după terminarea ei, dar se declară susținători ai capitalismului și ai libertății de a alege. Reprezentanții mediului eco - Una dintre organizaţii susţine protestele, în timp ce cealaltă preferă no mic vor absolvenți cu patalama, dar declară că ea nu valorează de fapt nimic. -

Redox DAS Artist List for Period: 01.12.2017
Page: 1 Redox D.A.S. Artist List for period: 01.12.2017 - 31.12.2017 Date time: Number: Title: Artist: Publisher Lang: 01.12.2017 00:00:03 HD 58212 LET'S RUN AWAY TOGETHER ANOUK & JENNIE LENA ANG 01.12.2017 00:02:20 HD 60249 DIM NAD MESTOM LEONART SLO 01.12.2017 00:06:10 HD 45218 WHEN LOVE TAKES OVER (DAVID GUETTAPIXIE LOTTCOVER) ANG 01.12.2017 00:09:33 HD 16145 LIVIN' ON THE EDGE OF THE NIGHT IGGY POP ANG 01.12.2017 00:12:37 HD 47700 JUTRA LYBRA SLO 01.12.2017 00:15:35 HD 07749 MYSTIFY INXS ANG 01.12.2017 00:18:53 HD 07970 CHIHUAHUA DARE ANG 01.12.2017 00:21:47 HD 51501 KAJ SI HOTEL AVTOMOBILI SLO 01.12.2017 00:25:28 HD 58965 THE GETAWAY RED HOT CHILI PEPPERS ANG 01.12.2017 00:29:51 HD 14740 SICK AND TIRED ANASTACIA ANG 01.12.2017 00:33:21 HD 00583 KER VES, DA TE LJUBIM VILI RESNIK SLO 01.12.2017 00:37:12 HD 58734 FEEL MAHMUT ORHAN FEAT SENA SENER ANG 01.12.2017 00:40:06 HD 03818 GENIE IN A BOTTLE CHRISTINA AGUILERA ANG 01.12.2017 00:43:43 HD 44060 SKRIVNOST TABU SLO 01.12.2017 00:47:20 HD 30451 SOMEBODY BRYAN ADAMS ANG 01.12.2017 00:51:53 HD 60364 UN AMORE D'ESTATE VALENTINA GRECO ITA 01.12.2017 00:54:58 HD 56361 ZIVLJENJE GRE NAPREJ LIVE ORLEK SLO 01.12.2017 00:57:42 HD 35970 WEATHER WITH YOU CROWDED HOUSE ANG 01.12.2017 01:01:19 HD 41957 MAGNIFICENT U2 ANG 01.12.2017 01:05:38 HD 56777 TIHO HAMO & TRIBUTE 2 LOVE SLO 01.12.2017 01:09:55 HD 02835 COME UNDONE ROBBIE WILLIAMS ANG 01.12.2017 01:14:24 HD 60975 A L I E N S COLDPLAY ANG 01.12.2017 01:19:00 HD 56640 TERASA PLIS SLO 01.12.2017 01:22:08 HD 01665 OUT OF REACH GABRIELLE ANG 01.12.2017 01:25:22 HD 15247 YOU AND I CELINE DION ANG 01.12.2017 01:29:20 HD 57347 MOJ LAJF DREAMON SLO 01.12.2017 01:33:17 HD 13982 IS IT COS' I'M COOL? MOUSSE T. -

S Sovereign Grace Lead Men Into Sin? Halliman to Macedonia Baptist Church, 2501 North Maplewood 1/1 CHARLES H
l'APercis Mai freeze Reluieen the Oeacher's lips 'will riei,e'r in.elt the hearer's 'heart. MISSIONARY PREMILLENNIAL BIBLICAL BAPTISTIC HERE IS A BRIEF REPORT ON •at Exameam NEW GUINEA MISSIONS We are truly grateful to be ing several hours a day studying PAID CIRCULATION IN ALL STATES AND MANY FOREIGN COUNTRIES able to carry letters and news the language. and information relative to the We feel there has been Consid- To the law and to the testimony; if they speak not according to this word work of Brother Fred Hallman. erable amount of progress made it is because there is no light in them.—Isaiah 8:20 in New Guinea. We consider in this work since we left the him one of God's great men and Mailing Address: Box 910, Ashland, Kentucky are glad to recommend him to our readers. Might it please the RUSSELL, KENTUCKY, AUGUST 6, 1960 WHOLE NUMBER 1150 Lord to raise up many friends in his behalf who will not oxly be financial supporters but pray-warriors as welL Send all offerings for Brother s Sovereign Grace Lead Men Into Sin? Halliman to Macedonia Baptist Church, 2501 North Maplewood 1/1 CHARLES H. SPURGEON you, there never were better men swearing, but to foolish talking Avenue. Chicago, Illinois, or di- in the world than the Puritans, and jesting. They were strict ob- rectly to us and we will for- l'ten'i New York Street Pulpit, and every one of them held fast servers of the Lord's day, spend- ward the same in his behalf. -

Songliste Englisch (Stand OKT 2020)
Sorted By Title Songliste Englisch (Stand OKT 2020) sortiert nach Songtitel (A‐Z) SONGCODE TITEL ARTIST 952335 (BARRY) ISLANDS IN THE STREAM COMIC RELIEF 950058 1,2 Step CIARA 989082 10 SECONDS JAZMINE SULLIVAN 988220 100 LETTERS HALSEY 950068 100 Years FIVE FOR FIGHTING 975699 100% MARIAH CAREY 978399 11 CASSADEE POPE 978329 17 AVRIL LAVIGNE 952336 17 FOREVER METRO STATION 988201 18 ONE DIRECTION 973914 18 INCHES LAUREN ALAINA 982406 1‐800‐273‐8255 ALESSIA CARA/KHALID 979696 1973 JAMES BLUNT 950051 1985 Bowling for Soup 985783 2 BECOME 1SPICE GIRLS 525945 2 BECOME 1Various Artist 951473 2 OUT OF 3 AINT BAD MEATLOAF 975727 2 REASONS T.I/TREY SONGZ 983962 2000 LIGHT YEARS AWAY GREEN DAY 952362 21 CENTURY BREAKDOWN GREEN DAY 952337 21 GUNS GREEN DAY 972729 212 two one two ZAEALIZ BANKS 950295 21ST CENTURY GIRLS Various Artist 952342 22 LILY ALLEN 974139 22 TAYLOR SWIFT 977798 23 MIKE WILL MADE 951554 24 HOURS FROM YOU NEXT OF KIN 975857 24 XMAS TIME 仓木麻衣 981411 24K MAGIC BRUNO MARS 525946 25 MINUTES MLTR 952618 29 PALMS ROBERT PLANT 981656 2U DAVID GUETTA 952359 3 (THREE) BRITNEY SPEARS 574095 3 THREE BRITNEY SPEARS 952361 3 WORDS CHERYL COLE 975708 30 DAYS THE SATURDAYS 952338 30 SECONDS TO MARS KINGS & QUEENS 982137 3005 CHILDISH GAMBINO 977782 365 DAYS ZZ WARD 574113 37 STITCHES DROWNING POOL 951250 4 BUGG O EN COCA‐COLA L ENGBERG 973695 4 EVER THE VERONICAS 988755 4 IN THE MORNING GWEN STEFANI 951976 4 MINUTES AVANT 574538 4 MINUTES MADONNA 986974 4 X 4MILEY CYRUS/NELLY 525317 4:55 Various Artist Seite 1 Sorted By Title SONGCODE TITEL -

Number Song Name 02003 09130 02010 02008 02005 02011 30999
Number Song Name Singer Name 02003 17 Avril Lavigne 09130 22 Taylor Swift 02010 23 Miley Cyrus 02008 212 Azealiz Banks & Lazy Jay 02005 1999 Gloria Estefan 02011 23346 Four Seasons 30999 1 + 1 Beyonce 02000 1 2 3 Gloria Estefan 02001 10,000 Promises Backstreet Boys 02002 100 Phần Trăm Mariah Carey 02004 18 Inches Lauren Alaina 02006 2 Become 1 Rowe 02007 2 Reasons Trey Songz 02012 25 Minutes Jascha Richter 02013 3 Way Lady Gaga 02014 30 Days Saturdays 02015 365 Days Zz Ward 02016 4 Minutes Madonna 02017 4 Seasons of Loneliness Madonna 02018 4, 55 Madonna 02019 40 Days Blessthefall 02021 4th Of July Brian McKnight 02020 4th Of July Fireworks Kelis 02022 5 O'Clock Tpain& Lily Allen 02023 50 Way To Leave Your Love Tpain& Lily Allen 32200 50 Way To Say Goodbye 09138 50 Ways To Say Goodbye Train 02024 50 Ways To Say Goodbye Train 02025 500 Miles 02026 500 Miles Peter Paul 02027 500 Miles Rumba 22343 500 Miles 02028 59 Th Street Bridge Song Peter Paul 02029 6 8 12 Brian 02030 7 Seconds Nench Cherry 02031 7 Years And 50 Days Groove Coverage 02032 9 Piece Rick Ross& Lil Wayne 02033 93 Million Miles Jason Mraz 28902 999 Đóa Hoa Hồng 02034 999 Roses Of Love Jason Mraz 5 TB ‐ K6800 1 EngLish Song List 02035 999,999 Tears Jason Mraz 02036 A Beautiful Lie 30 Second To Mars 02037 A Better Love Next Time Ruise&Pablo 02038 A Certain Smile Ruise&Pablo 02039 A Christmas Carol Jose Mari Chan 02040 A Christmas Greeting Jeremiah 02041 A Day In The Life Beatles 22163 A Dear John Letter 02042 A dear John Letter Lounge Cardwell&Rich 02043 A dear Johns Letter -

Fifth National Assembly
No. 7 of 2010 FIFTH NATIONAL ASSEMBLY PARLIAMENTARY DEBATES (HANSARD) FIRST SESSION TUESDAY 13 JULY 2010 2 CONTENTS PAPERS LAID QUESTIONS (ORAL) MOTION – SUSPENSION OF S.O 10 (2) BILL (PUBLIC) MOTION -- GOVERNMENT PROGRAMME 2010-2015 ADJOURNMENT QUESTIONS (WRITTEN) 3 Members Members THE CABINET (Formed by Dr. the Hon. Navinchandra Ramgoolam) Dr. the Hon. Navinchandra Ramgoolam, GCSK, FRCP Prime Minister, Minister of Defence, Home Affairs and External Communications Dr. the Hon. Ahmed Rashid Beebeejaun, GCSK, FRCP Deputy Prime Minister, Minister of Energy and Public Utilities Hon. Charles Gaëtan Xavier-Luc Duval, GCSK Vice-Prime Minister, Minister of Social Integration and Economic Empowerment Hon. Pravind Kumar Jugnauth Vice-Prime Minister, Minister of Finance and Economic Development Hon. Anil Kumar Bachoo Minister of Public Infrastructure, National Development Unit, Land Transport and Shipping Dr. the Hon. Arvin Boolell Minister of Foreign Affairs, Regional Integration and International Trade Dr. the Hon. Abu Twalib Kasenally, FRCS Minister of Housing and Lands Hon. Mrs Sheilabai Bappoo, GOSK Minister of Gender Equality, Child Development and Family Welfare Hon. Nandcoomar Bodha Minister of Tourism and Leisure Dr. the Hon. Vasant Kumar Bunwaree Minister of Education and Human Resources Hon. Satya Veryash Faugoo Minister of Agro-Industry and Food Security Hon. Showkutally Soodhun Minister of Industry and Commerce Hon. Devanand Virahsawmy, GOSK Minister of Environment and Sustainable Development Dr. the Hon. Rajeshwar Jeetah Minister of Tertiary Education, Science, Research and Technology Hon. Satyaprakash Ritoo Minister of Youth and Sports Hon. Mrs Leela Devi Dookun-Luchoomun Minister of Social Security, National Solidarity and Reform Institutions Hon. Louis Hervé Aimée Minister of Local Government and Outer Islands Hon. -

Number Name Artist
English Songbook Ver 2016_8 By Song Title Number Name Artist 90709 1 Mariah Carey 91558 1 2 3 4 PLAIN WHITE T'S 80001 1 thing AMERIN 87548 1 Thing AMERIE 80002 1,2 step 83807 1+1 BEYONCé 83849 10 seconds JAZMINE SULLIVAN 88625 100 PURE LOVE Crystal Waters 80003 100 years five for fighting 80004 100% pure love CRYSTAL WATERS 84555 1000 faces RANDY MONTANA 80005 10000 promises BACKSTREET BOYS 80006 123 GLORIA ESTEFAN 80007 143 BOBBY BRACKINS&RAY J 80008 16@war KARINA 90024 16WAR KARINA 87676 17 Avril Lavigne 90348 18 Inches Lauren Alaina 88061 19 And Crazy Bomshel 89618 1973 James Blunt 91206 1983 Neon Trees 88094 1985 Bowling For Soup 85358 1994 JASON ALDEAN 80009 2 become 1 SPICE GIRLS 80010 2 in the morning NEW KIDS ON THE BLOC 91216 2 In The Morning New Kids On The Block 80011 2 out of three ain't bad MEATLOAF 90885 2 Out Of Three Ain't Bad Meat Loaf 84513 2 reasons TREY SONGZ&T.I 92756 2 Reasons Trey Songz&T.I. 89712 2012 Jay Sean 89718 2012 It Ain't The End Jay Sean&Nicki Minaj 83841 21 gun GREEN DAY 87274 21 Questions 50 Cent&Nate Dogg 87719 212 Azealiz Banks&Lazy Jay 89419 21st Century Breakdown Green Day 93033 21st Century Girl Willow Smith 91928 21st Century Life Sam Sparro 85359 22 TAYLOR SWIFT 90448 22 Lily Allen 85594 23 MIKE WILL MADE IT&MILEY CYRUS&WIZ KHALIFA&JUICY J 80012 25 minutes MICHAEL LEARNS TO ROCK 80013 3 BRITNEY SPEARS 88975 0.125 Eminem 90327 3 Way Lady Gaga&Justin Timberlake&The Lonely Island 92577 30 Days The Saturdays 85750 3000 miles EMBLEM3 93100 365 Days ZZ Ward www.karaoke4less.com Page 1 of 218 English -

Deutsche Nationalbibliografie
Deutsche Nationalbibliografie Reihe T Musiktonträgerverzeichnis Monatliches Verzeichnis Jahrgang: 2013 T 03 Stand: 20. März 2013 Deutsche Nationalbibliothek (Leipzig, Frankfurt am Main) 2013 ISSN 1613-8945 urn:nbn:de:101-ReiheT03_2013-8 2 Hinweise Die Deutsche Nationalbibliografie erfasst eingesandte Pflichtexemplare in Deutschland veröffentlichter Medienwerke, aber auch im Ausland veröffentlichte deutschsprachige Medienwerke, Übersetzungen deutschsprachiger Medienwerke in andere Sprachen und fremdsprachige Medienwerke über Deutschland im Original. Grundlage für die Anzeige ist das Gesetz über die Deutsche Nationalbibliothek (DNBG) vom 22. Juni 2006 (BGBl. I, S. 1338). Monografien und Periodika (Zeitschriften, zeitschriftenartige Reihen und Loseblattausgaben) werden in ihren unterschiedlichen Erscheinungsformen (z.B. Papierausgabe, Mikroform, Diaserie, AV-Medium, elektronische Offline-Publikationen, Arbeitstransparentsammlung oder Tonträger) angezeigt. Alle verzeichneten Titel enthalten einen Link zur Anzeige im Portalkatalog der Deutschen Nationalbibliothek und alle vorhandenen URLs z.B. von Inhaltsverzeichnissen sind als Link hinterlegt. Die Titelanzeigen der Musiktonträger in Reihe T sind, wie Katalogisierung, Regeln für Musikalien und Musikton-trä- auf der Sachgruppenübersicht angegeben, entsprechend ger (RAK-Musik)“ unter Einbeziehung der „International der Dewey-Dezimalklassifikation (DDC) gegliedert, wo- Standard Bibliographic Description for Printed Music – bei tiefere Ebenen mit bis zu sechs Stellen berücksichtigt ISBD (PM)“ zugrunde. -

English Songbook Ver 2-2017.Xls Song # Name Artist 088975 0.125 Eminem 090055 0.208333333 Katy B 090709 1 Mariah Carey 128001 1
English Songbook Ver 2-2017.xls Song # Name Artist 088975 0.125 Eminem 090055 0.208333333 Katy B 090709 1 Mariah Carey 128001 1 2 3 Gloria Estefan 091558 1 2 3 4 PLAIN WHITE T'S 128002 1 Sweet Day Mariah Carey Boyz Ii M 080001 1 thing AMERIN 087548 1 Thing AMERIE 080002 1,2 step 083807 1+1 BEYONCé 083849 10 seconds JAZMINE SULLIVAN 128003 10,000 Promises Backstreet Boys 088625 100 PURE LOVE Crystal Waters 080003 100 years five for fighting 080004 100% pure love CRYSTAL WATERS 084555 1000 faces RANDY MONTANA 080005 10000 promises BACKSTREET BOYS 080006 123 GLORIA ESTEFAN 080007 143 BOBBY BRACKINS&RAY J 080008 16@war KARINA 090024 16WAR KARINA 087676 17 Avril Lavigne 090348 18 Inches Lauren Alaina 088061 19 And Crazy Bomshel 089618 1973 James Blunt 091206 1983 Neon Trees 088094 1985 Bowling For Soup 085358 1994 JASON ALDEAN 128004 1999 Prince 128005 1everytime I Close My Eyes Backstr 080009 2 become 1 SPICE GIRLS 128006 2 Become 1 Spice Girls 128007 2 Become 1 Unknown 080010 2 in the morning NEW KIDS ON THE BLOC 091216 2 In The Morning New Kids On The Block 080011 2 out of three ain't bad MEATLOAF 090885 2 Out Of Three Ain't Bad Meat Loaf 084513 2 reasons TREY SONGZ&T.I 092756 2 Reasons Trey Songz&T.I. 128008 2 Unlimited No Limit 089712 2012 Jay Sean 089718 2012 It Ain't The End Jay Sean&Nicki Minaj 083841 21 gun GREEN DAY 087274 21 Questions 50 Cent&Nate Dogg 087719 212 Azealiz Banks&Lazy Jay 089419 21st Century Breakdown Green Day Page 1 of 363 English Songbook Ver 2-2017.xls 093033 21st Century Girl Willow Smith 091928 21st Century Life -
Register Analysis and Linguistic Manipulation in the Murderers of the True Crime Series ―I Am a Killer‖ »
Trabajo de Fin de Grado «Register Analysis and Linguistic Manipulation in the Murderers of the true crime series ―I am a killer‖ » Autora: Lucía Elena Cano Gómez Tutora: Mª Carmen Merino Ferrada Grado en Estudios Ingleses Curso académico: 2019/2020 Presentación: 02/09/2020 FACULTAD DE FILOSOFÍA Y LETRAS INDEX ABSTRACT……………………………………………………………………………………1 INTRODUCTION……………………………………………………………………………..2 1. THEORETICAL FRAMEWORK………………………………………………………...3 1.1. DISCOURSE ANALYSIS……………………………………………………………3 1.2.REGISTER…………………………………………………………………………….6 1.3. FORENSIC LINGUISTICS………………………………………………………….10 1.3.1. THE LINGUISTICS OF LYING………………………………………………12 1.3.2. LIES AND DISCOURSE ANALYSIS………………………………………..13 2. METHODOLOGY OF THE ANALYSIS……………………………………………….18 3. PRACTICAL ANALYSIS: REGISTER…………………………………………………19 3.1. SITUATIONAL ANALYSIS...……………………………………………...............19 3.1.1. ACCOMPANIED KILLERS ………..………………………………………27 3.1.2. LONE KILLERS ……………………………………………………………28 3.2. LINGUISTIC ANALYSIS……..……………………………………………………29 3.2.1. ACCOMPANIED KILLERS‘ DATA……………………………………….29 3.2.2. LONE KILLERS‘ DATA……………………………...................................34 3.3. FUNCTIONAL INTERPRETATION………………………………………………..40 3.3.1. ACCOMPANIED KILLERS‘ CORPUS……………………………….……40 3.3.2. LONE KILLERS‘ CORPUS…………………………………………………45 3.4. COMPARATIVE ANALYSIS……………………………………………………….50 3.5. THE LINGUISTIC MANIPULATION OF THE REALITY: RESULTS…………...60 4. CONCLUSIONS………………………………………………………………………….65 BIBLIOGRAPHY…………………………………………………………………………….68 APPENDIX…………………………………………………………………………………...75 5.1 LINGUISTIC FEATURES