Aging Physiology, Pharmacokinetics & Pharmacodynamics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -

Parenteral Dilantin® (Phenytoin Sodium Injection, USP) WARNING
1 Parenteral Dilantin (Phenytoin Sodium Injection, USP) WARNING: CARDIOVASCULAR RISK ASSOCIATED WITH RAPID INFUSION The rate of intravenous Dilantin administration should not exceed 50 mg per minute in adults and 1-3 mg/kg/min (or 50 mg per minute, whichever is slower) in pediatric patients because of the risk of severe hypotension and cardiac arrhythmias. Careful cardiac monitoring is needed during and after administering intravenous Dilantin. Although the risk of cardiovascular toxicity increases with infusion rates above the recommended infusion rate, these events have also been reported at or below the recommended infusion rate. Reduction in rate of administration or discontinuation of dosing may be needed (see WARNINGS and DOSAGE AND ADMINISTRATION). DESCRIPTION Dilantin (phenytoin sodium injection, USP) is a ready-mixed solution of phenytoin sodium in a vehicle containing 40% propylene glycol and 10% alcohol in water for injection, adjusted to pH 12 with sodium hydroxide. Phenytoin sodium is related to the barbiturates in chemical structure, but has a five-membered ring. The chemical name is sodium 5,5-diphenyl-2, 4- imidazolidinedione represented by the following structural formula: CLINICAL PHARMACOLOGY Mechanism of Action Phenytoin is an anticonvulsant which may be useful in the treatment of generalized tonic clonic status epilepticus. The primary site of action appears to be the motor cortex where spread of seizure activity is inhibited. Possibly by promoting sodium efflux from neurons, phenytoin tends to stabilize the threshold against hyperexcitability caused by excessive stimulation or environmental changes capable of reducing membrane sodium gradient. This includes the reduction of posttetanic potentiation at synapses. Loss of posttetanic potentiation prevents cortical seizure foci from detonating adjacent cortical areas. -

Dilantin (Phenytoin Sodium) Extended Oral Capsule Three Times Daily and the Dosage Then Adjusted to Suit Individual Requirements
Dilantin® (Phenytoin Sodium) 100 mg Extended Oral Capsule DESCRIPTION Phenytoin sodium is an antiepileptic drug. Phenytoin sodium is related to the barbiturates in chemical structure, but has a five-membered ring. The chemical name is sodium 5,5-diphenyl-2, 4-imidazolidinedione, having the following structural formula: Each Dilantin— 100 mg Extended Oral Capsule—contains 100 mg phenytoin sodium. Also contains lactose monohydrate, NF; confectioner’s sugar, NF; talc, USP; and magnesium stearate, NF. The capsule body contains titanium dioxide, USP and gelatin, NF. The capsule cap contains FD&C red No. 28; FD&C yellow No. 6; and gelatin NF. Product in vivo performance is characterized by a slow and extended rate of absorption with peak blood concentrations expected in 4 to 12 hours as contrasted to Prompt Phenytoin Sodium Capsules, USP with a rapid rate of absorption with peak blood concentration expected in 1½ to 3 hours. CLINICAL PHARMACOLOGY Phenytoin is an antiepileptic drug which can be used in the treatment of epilepsy. The primary site of action appears to be the motor cortex where spread of seizure activity is inhibited. Possibly by promoting sodium efflux from neurons, phenytoin tends to stabilize the threshold against hyperexcitability caused by excessive stimulation or environmental changes capable of reducing membrane sodium gradient. This includes the reduction of posttetanic potentiation at synapses. Loss of posttetanic potentiation prevents cortical seizure foci from detonating adjacent cortical areas. Phenytoin reduces the maximal activity of brain stem centers responsible for the tonic phase of tonic-clonic (grand mal) seizures. The plasma half-life in man after oral administration of phenytoin averages 22 hours, with a range of 7 to 42 hours. -

Drug Therapy in Older Adults
Interprofessional Geriatrics Training Program Drug Therapy in Older Adults HRSA GERIATRIC WORKFORCE ENHANCEMENT FUNDED PROGRAM Grant #U1QHP2870 EngageIL.com Acknowledgements Author: Michael Koronkowski, PharmD, CGP Contributor: Joseph T. Hanlon, PharmD, MS Editors: Valerie Gruss, PhD, APN, CNP-BC Memoona Hasnain, MD, MHPE, PhD Expert Interviewee: Todd Semla, MS, PharmD, BCPS, FCCP, AGSF Case: Medication Therapy in Older Adults • Mrs. Roberts is a 77-year-old widow who lives alone • She has multiple medical problems, which include: chronic obstructive pulmonary disease (COPD), hypertension (HTN), diabetes (DM), coronary artery disease (CAD), cerebral vascular accident (CVA), osteoporosis, osteoarthritis, gastroesophageal reflux disease (GERD), anxiety, insomnia, allergic rhinitis, glaucoma, multiple falls at home, and currently smokes 4 cigarettes/day • Though she has prescription insurance (Medicare Part D), she has difficulty affording her monthly copayments • She tries to take her medications as prescribed, but she misses doses Case: Medication Therapy in Older Adults • She is currently taking 21 medications, which include: • Budesonide/formoterol, albuterol, amlodipine, insulin glargine, insulin aspart, sitagliptin, alendronate, acetaminophen, diclofenac gel, glucosamine, meclizine, omeprazole, mirtazapine, zolpidem, trazodone, diphenhydramine, fluticasone, estrogen vaginal cream, triamcinolone cream, and timolol eye drops Learning Objectives Upon completion of this module, learners will be able to: 1. Recognize the common consequences of inappropriate medication use and polypharmacy 2. Describe the key principles of pharmacology and the effects of age on medication use 3. Summarize the main approaches to improve medication prescribing and monitoring 4. Describe a stepwise approach to integrating into practice a process for prescribing and monitoring medications 5. Identify provider and patient resources to support drug prescribing and monitoring medications Case: Medication Therapy in Older Adults Mrs. -

Potentially Harmful Drugs in the Elderly: Beers List
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− March 2019 ~ Resource #350301 Potentially Harmful Drugs in the Elderly: Beers List In 1991, Dr. Mark Beers and colleagues published a methods paper describing the development of a consensus list of medicines considered to be inappropriate for long-term care facility residents.12 The “Beers list” is now in its sixth permutation.1 It is intended for use by clinicians in outpatient as well as inpatient settings (but not hospice or palliative care) to improve the care of patients 65 years of age and older.1 It includes medications that should generally be avoided in all elderly, used with caution, or used with caution or avoided in certain elderly.1 There is also a list of potentially harmful drug-drug interactions in seniors, as well as a list of medications that may need to be avoided or have their dosage reduced based on renal function.1 This information is not comprehensive; medications and interactions were chosen for inclusion based on potential harm in relation to benefit in the elderly, and availability of alternatives with a more favorable risk/benefit ratio.1 The criteria no longer address drugs to avoid in patients with seizures or insomnia because these concerns are not unique to the elderly.1 Another notable deletion is H2 blockers as a concern in dementia; evidence of cognitive impairment is weak, and long-term PPIs pose risks.1 Glimepiride has been added as a drug to avoid. Some drugs have been added with cautions (dextromethorphan/quinidine, trimethoprim/sulfamethoxazole), and some have had cautions added (rivaroxaban, tramadol, SNRIs). -

Effect of Beers Criteria on Healthcare Utilization and Cost in Community-Dwelling Elderly Patients
Medical University of South Carolina MEDICA MUSC Theses and Dissertations 2018 Effect of Beers Criteria on Healthcare Utilization and Cost in Community-Dwelling Elderly Patients Courtney O'Neill Roldan Medical University of South Carolina Follow this and additional works at: https://medica-musc.researchcommons.org/theses Recommended Citation Roldan, Courtney O'Neill, "Effect of Beers Criteria on Healthcare Utilization and Cost in Community- Dwelling Elderly Patients" (2018). MUSC Theses and Dissertations. 294. https://medica-musc.researchcommons.org/theses/294 This Dissertation is brought to you for free and open access by MEDICA. It has been accepted for inclusion in MUSC Theses and Dissertations by an authorized administrator of MEDICA. For more information, please contact [email protected]. EFFECT OF BEERS CRITERIA ON HEALTHCARE UTILIZATION AND COST IN COMMUNITY-DWELLING ELDERLY PATIENTS by Courtney O’Neill Roldan, MHA A dissertation submitted to the faculty of the Medical University of South Carolina in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the College of Health Professions © Courtney O’Neill Roldan 2018 All Rights Reserved Acknowledgments I would like to acknowledge my dissertation committee chair Dr. Kit Simpson, and committee members Dr. Annie Simpson, Dr. William Moran, and Dr. David Taber for their guidance throughout this study. Without their unending service and expertise this project would not have been successful. Not only did Dr. Kit Simpson provide the data for this study, but she also introduced me to Beers Criteria many months before this project came to fruition. I am especially grateful for Dr. Kit Simpson’s mentorship that enabled me to preserve through this project, Dr. -

Management of Alcohol Withdrawal
Management of alcohol withdrawal Q2: What interventions are safe and effective for the management of alcohol withdrawal, including treatment for alcohol withdrawal seizures and prevention and treatment for acute Wernicke's encephalopathy? Background Alcohol withdrawal can be uncomfortable and occasionally life threatening. Pharmacological management of alcohol withdrawal is an essential component of alcohol dependence. Benzodiazepines (BZDs), non-sedating anticonvulsants and antipsychotics are commonly used in the treatment of alcohol withdrawal. Given that they are all potentially toxic medications, what is the evidence that the benefits of their use justify the risks? Which is more effective? Population/Intervention(s)/Comparison/Outcome(s) (PICO) Population: people with alcohol dependence commencing alcohol withdrawal Interventions: benzodiazepines anticonvulsants (non sedating i.e. non barbiturates and not chlormethiazole) antipsychotics Comparison: placebo and/or active treatment Outcomes: severity of withdrawal complications of withdrawal (seizures, delirium) completion of withdrawal death 1 Management of alcohol withdrawal List of the systematic reviews identified by the search process INCLUDED IN GRADE TABLES OR FOOTNOTES Ntais C et al (2005). Benzodiazepines for alcohol withdrawal. Cochrane Database of Systematic Review, (3):CD005063. Polycarpou A et al (2005). Anticonvulsants for alcohol withdrawal. Cochrane Database of Systematic Reviews, (3):CD005064. Mayo-Smith MF (1997). Pharmacological management of alcohol withdrawal. A -

Jp Xvii the Japanese Pharmacopoeia
JP XVII THE JAPANESE PHARMACOPOEIA SEVENTEENTH EDITION Official from April 1, 2016 English Version THE MINISTRY OF HEALTH, LABOUR AND WELFARE Notice: This English Version of the Japanese Pharmacopoeia is published for the convenience of users unfamiliar with the Japanese language. When and if any discrepancy arises between the Japanese original and its English translation, the former is authentic. The Ministry of Health, Labour and Welfare Ministerial Notification No. 64 Pursuant to Paragraph 1, Article 41 of the Law on Securing Quality, Efficacy and Safety of Products including Pharmaceuticals and Medical Devices (Law No. 145, 1960), the Japanese Pharmacopoeia (Ministerial Notification No. 65, 2011), which has been established as follows*, shall be applied on April 1, 2016. However, in the case of drugs which are listed in the Pharmacopoeia (hereinafter referred to as ``previ- ous Pharmacopoeia'') [limited to those listed in the Japanese Pharmacopoeia whose standards are changed in accordance with this notification (hereinafter referred to as ``new Pharmacopoeia'')] and have been approved as of April 1, 2016 as prescribed under Paragraph 1, Article 14 of the same law [including drugs the Minister of Health, Labour and Welfare specifies (the Ministry of Health and Welfare Ministerial Notification No. 104, 1994) as of March 31, 2016 as those exempted from marketing approval pursuant to Paragraph 1, Article 14 of the Same Law (hereinafter referred to as ``drugs exempted from approval'')], the Name and Standards established in the previous Pharmacopoeia (limited to part of the Name and Standards for the drugs concerned) may be accepted to conform to the Name and Standards established in the new Pharmacopoeia before and on September 30, 2017. -

NSG0315 CE Insomnia Yogesh.Indd
2.5 2.5 ANCC PHARM CONTACT CONTACT HOURS HOURS 38 l Nursing2015 l March www.Nursing2015.com Copyright © 2015 Wolters Kluwer Health, Inc. All rights reserved. Pharmacology for insomnia: Consider the options By Jamie M. Rosini, PharmD, BCPS, and Pooja Dogra, PharmD, BCACP, CDE INSOMNIA IS POOR SLEEP quality, defined as difficulty initiating and/ or maintaining sleep or waking up too early despite adequate sleep op- portunity, which then interferes with daytime functioning.1,2 Consid- ered the most common sleep disorder, insomnia affects approximately 60 million Americans annually.3 To care for patients suffering from insomnia, clinicians must first thoroughly assess their sleep habits, identifying and addressing under- lying conditions that may contribute to insomnia such as depression, emotional stress, sleep apnea, or substance abuse. Patients should also be counseled about sleep hygiene, stimulus control, and behavioral approaches to improving the quality of sleep. (See Helping improve a patient’s sleep hygiene.) If indicated, the healthcare provider may then add a medication to the treatment regimen for a limited period. The choice of medication is based on many factors, including the type of insomnia (difficulty falling asleep, staying asleep, or both).3,4 (See Classifying insomnia types.) This article provides an overview of agents commonly used to treat insomnia, including prescription drugs, over-the-counter (OTC) medi- cations, and herbal or dietary products. By understanding how and why certain medications help treat insomnia, nurses can help patients use them safely to get a good night’s sleep. Unless otherwise specified, the following information applies to adults, not children. -

Assessment Report for Zytiga (Abiraterone) Procedure
21 July 2011 EMA/CHMP/542871/2011 Committee for Medicinal Products for Human Use (CHMP) Assessment Report For Zytiga (abiraterone) Procedure No.: EMEA/H/C/002321 Assessment Report as adopted by the CHMP with all information of a commercially confidential nature deleted 7 Westferry Circus ● Canary Wharf ● London E14 4HB ● United Kingdom Telephone +44 (0)20 7418 8400 Facsimle +44 (0)20 7523 7455 E-mail [email protected] Website www.ema.europa.eu An agency of the European Union TABLE OF CONTENTS 1. Background information on the procedure .............................................. 5 1.1. Submission of the dossier .................................................................................... 5 1.2. Steps taken for the assessment of the product........................................................ 5 2. Scientific discussion................................................................................ 6 2.1. Introduction....................................................................................................... 6 2.2. Quality aspects .................................................................................................. 8 2.2.1. Introduction.................................................................................................... 8 2.2.2. Active Substance ............................................................................................. 9 2.2.3. Finished Medicinal Product .............................................................................. 10 2.2.4. Discussion on chemical, pharmaceutical -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO -
Beers Criteria for Potentially Inappropriate Medication Use in Older Adults
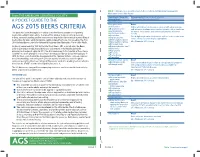
TABLE 1. 2015 American Geriatrics Society Beers Criteria for Potentially Inappropriate Medication Use in Older Adults From THE AMERICAN GERIATRICS SOCIETY Organ System, Therapeutic Recommendation, Rationale, Quality of Evidence Category, Drug(s) (QE), Strength of Recommendation (SR) A POCKET GUIDE TO THE Anticholinergics First-generation Avoid antihistamines: Highly anticholinergic; clearance reduced with advanced age, AGS 2015 BEERS CRITERIA ■ Brompheniramine and tolerance develops when used as hypnotic; risk of confusion, ■ Carbinoxamine This guide has been developed as a tool to assist healthcare providers in improving dry mouth, constipation, and other anticholinergic effects or ■ Chlorpheniramine toxicity medication safety in older adults. The role of this guide is to inform clinical decision- ■ Clemastine Use of diphenhydramine in situations such as acute treatment of ■ making, research, training, quality measures and regulations concerning the prescribing of Cyproheptadine severe allergic reaction may be appropriate medications for older adults to improve safety and quality of care. It is based on The AGS ■ Dexbrompheniramine QE = Moderate; SR = Strong 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. ■ Dexchlorpheniramine ■ Dimenhydrinate Originally conceived of in 1991 by the late Mark Beers, MD, a geriatrician, the Beers ■ Diphenhydramine (oral) Criteria catalogues medications that cause side effects in the elderly due to the ■ Doxylamine physiologic changes of aging. In 2011, the AGS