State of Florida Division of Administrative Hearings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2017 Annual Report
Annual Report 2017 Message from the Executive Director The accomplishments of the Plan Hillsborough staff in 2017 are many! We have much to be proud of and through this report offer just some of the highlights. Throughout the year, I have seen our staff continue to exemplify our agency values as we serve the Planning Commission, River Board, and Metropolitan Planning Organization as well as the four local governments. Integrity and Trust –Several projects illustrate the goal of meeting the needs of the community while building relationships and trust. Vision Zero required numerous partnerships to create and begin to implement an action plan. Redistricting for the City of Tampa likewise necessitated building trust as we identified important needs within our community. Innovation – We strive to think out of the box and have used technology to our Melissa Zornitta, AICP advantage by creating an eCeptionist to replace our retiring receptionist and a Executive Director Community Health Atlas to provide planners and citizens with a baseline profile of community health. Transparency – Getting the community involved and having a clear understanding of our projects is vital to creating successful plans. This was illustrated throughout the transparent process and open communication we had in projects like the Brandon East-West Corridor Study and the Plant City Road Extension Studies. Stewardship – With the aim of improving our existing plan amendment review process, we undertook an outside review by students at the University of South Florida to look for opportunities to do things more efficiently and to make better use of our resources. Servant Leadership – We added on-site office hours at each of the three cities to better meet the needs of the jurisdiction and clients who seek our services. -

Die Sonnenkueste
Sunshine Mini Road Rally . PAGE 7 April-May-June 2013 Agent Orange . PAGE 4 PRESIDENTS MESSAGE . PAGE 8 BMW Die Sonnenkueste NEWS FROM THE FLORIDA SUNCOAST CHAPTER OF THE BMW CAR CLUB OF AMERICA Tour to Yalaha, Antiques, and German Food By Jim Ringold This driving tour was organized by our Florida Sun- From Yalaha, Bob lead us on a tour to the Renninger’s coast Chapter president Bob Ziegler. He stated that Antique Center, an antique and collectible mall on U.S. the tour was primarily for the ladies, but one that the 441 in Mount Dora. It has a large air conditioned building guys could enjoy too. The meeting point was the with about any type of antique/collectible you can imagine. wonderful German Yalaha Bakery in Yalaha, Florida. In addition to the inside booths there were outside build- Some members stopped first at our traditional tour ings featuring an even larger variety of interesting stuff; breakfast spot, the Cracker Barrel at I-75 and S.H. even a toy store with lots of model cars! 50. Those who did not eat at the Cracker Barrel found plenty of German pastries to carb up on at the bak- ery. There were shaded picnic tables outside to sit at while eating the treats and listen to some live Continued on page 3 Mexican music. Beer and bratwurst were also avail- able outside at an outside concession. Yalaha Bakery Member’s Only parking area PAGE 2 DIE SONNENKUESTE Chapter And CCA Information Officers / Board Members Chairpersons / Directors Inside This Issue Bob Ziegler [email protected] Angela Carlascio Yalaha / Renningers…………...…...1 -

2016-17 Staff
The Menorah , Vol 17 Issue 2 April, 2017 Temple Emanuel 600 Lake Hollingsworth Dr. Lakeland, FL 33803 Service Times Volume 17, Issue 2 Volume 17, Issue 2 April, 2017 Friday evenings - 7:30 p.m. April, 2017 Saturday mornings at 9:30 a.m. Sunday School at 9:45 a.m. Note from Rabbi Goldstein, Temple Emanuel Office Hours 600 Lake Hollingsworth Dr. Monday - Thursday: 9 - 2pm Dear Members and Friends, Lakeland, FL 33803 Friday: 9 - Noon (863) 682-8616 March 15th marked the end of my first five months [email protected] here at Temple Emanuel. It has been a busy five Rabbi Goldstein's email: months filled with all of the normal processes of [email protected] www.TempleEmanuelLakeland.com getting to know one another. From my personal perspective it has been a rewarding and productive time, and I look forward to continuing to learn more about our community and the extended family it encompasses. In the days ahead we will be celebrating Pesuch together. There are several www.Facebook.com/Temple Emanuel Lakeland adult education courses on the schedule and there will be continued in- reach and out-reach to the members of our community. Inside this issue: There is a story I want to share with you. I am not sure of the source, Rabbi Goldstein's Letter 1-2 nor can I vouch for it being true, but it contains a powerful message for all of us. The story goes like this – Presidents Corner 2-3 His name was Josh. He has wild hair, wears a t-shirt with Schedule of Up-coming 3 holes in it, jeans and no shoes. -

Remembering Mike Joffee by Gerry Curts Although Zonefest Was Brought Back a Few Years Ago, It Has Never Been the Same
PORSCHE CLUB OF AMERICA • SUNCOAST REGION PORSCHE Profile Photo by Norm Sippel NOVEMBER 2015 PORSCHE NOVEMBER 2015 ProfileAlso available at: www.SuncoastPCA.org 2015 Officers & Board of Directors Officers President – Jill Perry 727-244-5137, [email protected] Past President – Page Obenshain 727-430-6532, [email protected] Vice President – Mike Mackenzie 727-510-5079, [email protected] Secretary – Pamela Richard 727-385-6606, [email protected] 17 19 Treasurer – Charles Neilson 727-595-7578, [email protected] Elected Directors Social – Missy Teasley 727-480-0355, [email protected] Safety – John Vita 941-714-7915, [email protected] Competition – Brian West 727-510-9252, [email protected] Membership Chair – Larry Mendez 813-695-7093, [email protected] Board Members at Large Ryan Johnson 941-773-7922, [email protected] 22 INSIDE THIS ISSUE PORSCHE CLUB OF AMERICA • SUNCOAST REGION Tori Lewis PORSCHE 727-424-1686, [email protected] The President’s Message ............................. 5 Don Mattran Profile In the Corners, Event Schedule ................. 7 941-365-5151, [email protected] The Membership Starting Line .................. 9 President Appointed Tech Tidbits .................................................11 Webmaster – Paul Bienick “Look!” ........................................................12 941-544-2775, [email protected] Rennsport Reunion V ................................17 Web Content & Email Blasts – Christian Rava 727-278-5991, [email protected] TRSS Teen Driving ....................................18 -

Suncoast Suncoast
a Tourism for 25 y Florid ears! Celebrating 25 years! Serving Florida Tourism since 1985! • Over 1 million copies printed annually. • Only Local Publication currently translated into three languages, German, Spanish & Portuguese (no extra charge). • Premium ad space available. • 1500 West Central Florida Locations receiving premium positioning in our brochure TheThe OfficialOfficial displays and special Attractions Map displays! • Encourages visitors to take advantage of the local sources of entertainment and points of SUNCOASTSUNCOAST interest. • Locations serviced as often as AttractionsAttractions MapMap 4 days per week. • Distributed at the I-75 & I-95 ow in its twenty-first year of publication, the Attractions Map continues to Florida Welcome Centers. N be recognized as one of the most effective, profit-driving advertising vehicles for this region. With its distribution to 1,500 locations in Pinellas, Hillsborough, • One rate covers entire West Central Pasco, Manatee and Sarasota Counties, it consistently provides outstanding visibility Florida area and their Gulf of Mexico Beaches for all of its featured establishments. Locations include shopping malls, museums, chambers of commerce, car rental agencies, • Attraction Maps also available hotels, restaurants, and attractions. The busiest of these locations at AAA offices statewide. are serviced as often as four days a week. In addition, these maps are passed out at local conventions and conferences and are also used Contact us for by large companies for business travelers. The Attractions Map also current pricing! welcomes international guests with its foreign language editions (757) 544-1212 currently available in German, Spanish and Portuguese. Visitors [email protected] and residents alike find its format and coupon savings a resourceful guide when planning vacations or weekend getaways. -

A Recreational Boating Characterization for Tampa and Sarasota Bays
This is a publication of the Florida Sea Grant Program and the Florida Fish and Wildlife Conservation Commission, supported by the National Sea Grant College Program of the United States Department of Commerce, National Oceanic and Atmospheric Administration under NOAA Grant #NA16RG-2195, and the Florida Department of Environmental Protection, Florida Coastal Management Program, pursuant to NOAA award number NA17OZ2330, with additional support from the Federal Aid in Sport Fish Restoration Program. The views expressed herein are those of the authors and do not necessarily reflect the views of these agencies. Additional copies are available for $30.00 from Florida Sea Grant, University of Florida, PO Box 110409, Gainesville, FL, 32611-0409, (352) 392-5870. August 2004 A Recreational Boating Characterization for Tampa and Sarasota Bays by Charles Sidman Coastal Planning Specialist Florida Sea Grant University of Florida Timothy Fik Associate Professor Department of Geography University of Florida Bill Sargent Research Scientist Florida Fish and Wildlife Conservation Commission Florida Marine Research Institute St. Petersburg, Florida Table of Contents LIST OF FIGURES ..................................................................................................................... iv LIST OF TABLES....................................................................................................................... v ACKNOWLEDGMENTS .......................................................................................................... -

CMP Must Be Adopted Into Local Government’S Comprehensive Plans
Suncoast Scenic Parkway Florida Scenic Highways Program Designation Application “Gateway to the Nature Coast” 2005 Florida Scenic Highways Program Designation Application for Suncoast Scenic Parkway: “Gateway to the Nature Coast” Submitted to: Florida Department of Transportation, Florida Scenic Highways Program Submitted by: Suncoast Parkway Corridor Advocacy Group i Endorsement by the Florida Department of Transportation Secretary As Secretary of the Florida Department of Transportation, the signature below indicates the approval and endorsement of this Corridor Management Plan and this corridor for designation as a Florida Scenic Highway. Florida Department of Transportation approval of this management plan represents our agreement to serve in a partnership with the Corridor Management Entity to preserve, enhance and maintain the designated scenic highway corridor. We recognize the grass roots initiative and strong local support for this corridor demonstrated by the communities involved in the preparation of this management plan. This corridor management plan acknowledges that the designated corridor will be subject to the requirements of the Section 1046© of the ISTEA which added a new subsection (s) to 23 USC 131 precluding outdoor advertising on designated scenic highways, and the requirements of the Uniform Relocation Act. I hereby designate this corridor as a Florida Scenic Highway. Denver J. Stutler Jr., P.E. Date Secretary, Florida Department of Transportation ii Potential Letter from the Secretary Confirming Designation Ms. Kathryn Starkey Ms. Diane Jones CAG Vice Chair Communications Manager Scenic Pasco Pasco Tourism 10928 Alico Pass 7530 Little Road, Suite 340 New Port Richey, Florida 34655 New Port Richey, Florida 34654 Ms. Lucie Ayers Mr. Joe Alpine Executive Director Executive Director Hillsborough County MPO West Pasco Chamber of Commerce 601 E. -

Hospice of the Florida Suncoast, Inc. (Suncoast) for Those Medicare Beneficiaries That Did’Not Meet the Medicare Reimbursement Requirements
DEPARTMENT OF HEALTH & HUMAN SERVICES Office Of InsPector General AU6I 6 1996 Memorandur Subject OPERATION RESTORE TRUST--Review of Hos@e Eligibility at the Hospice of the Florida Sun~ast, Inc. (GIN: A-04-95-02111) ‘To Bruce C. Vladeck Administrator .Health Care Financing .Administratio~ This memorandum is to alert you to t& issuance On August 19, 19 9 6- - - of our final report. A copy is attached. The objective of OUTreview was to evaluate hospice eligibility ~etermin&tions for beneficiaries that remained in hospice care for more than 210 @ys. We also determined the amount of payments made to the Hospice of the Florida Suncoast, Inc. (Suncoast) for those Medicare beneficiaries that did’not meet the Medicare reimbursement requirements. Our review included a medical evaIuation of Suncoast’s eligibility detern&ations for 364 beneficiaries who had been in hospice care for more than 210 days. Of the 364 cases, 237 were active in hospice at the time of our review and represented 26 percent of the total active Medicare hospice beneficiaries at Suncoast as of April 30, 1995. The review showed that: o 176 of the beneficiaries were not eligible for hospice coverage; and, o for 118 beneficiaries, we were unable to conclusively determine their terminal illness. Our medical determinations were made by physicians employed by or under contract with the Medicare peer review organization (PRO) for Florida. In addition, 30 cases reviewed by the PRO were also reviewed by fiscal intermediary (FI) kedical staff as part of their initial review of all the cases. The FI agreed with all 30 of the PRO’s decisions. -

Rainy Season 2004 Story
Rainy Season 2004 Story Fourth Summer in Row with Above Normal Rainfall A Review of Summer 2004 in West Central and Southwest Florida One of many flood scenes on Florida's Suncoast during September 2004. This photograph was taken on the State Road 54 bridge over the Anclote River (Pasco County) just north of Elfers, a day after Frances exited the area. Overview Few Suncoasters will soon forget the summer of 2004, which began in typical fashion with a spate of strong to severe thunderstorms, was followed by a relatively dry and hot period toward the middle, and finished with a six week blitz of tropical cyclones. Through mid July, areal rainfall was actually running below normal, though given the nature of Florida thunderstorms, some areas were quite wet while others were becoming parched. Conditions began to change thereafter, as general rainfall increased between mid July and early August, especially in the Tampa Bay metropolitan area. Then came the hammer. From August 12th through September 27th, the Suncoast was affected directly or indirectly by five tropical cyclones, which produced some type of weather hazard for all residents. Each system had its own "calling card". Tropical Storm Bonnie, making landfall outside of the Suncoast, nonetheless caused overwash and minor coastal flooding along the Nature Coast. Hurricane Charley was the worst windstorm to rip Florida since Andrew. Hurricanes Frances and Jeanne were sister acts, fairly large systems tracking east to west across the peninsula from the Treasure Coast to the Nature Coast. Frances will be remembered for two days of torrential rains and wind; Jeanne's faster movement held its similar effects to one day. -

Medicare Hospice Provider Compliance Audit: Suncoast Hospice
Department of Health and Human Services OFFICE OF INSPECTOR GENERAL MEDICARE HOSPICE PROVIDER COMPLIANCE AUDIT: SUNCOAST HOSPICE Inquiries about this report may be addressed to the Office of Public Affairs at [email protected]. Amy J. Frontz Deputy Inspector General for Audit Services May 2021 A-02-18-01001 Office of Inspector General https://oig.hhs.gov The mission of the Office of Inspector General (OIG), as mandated by Public Law 95-452, as amended, is to protect the integrity of the Department of Health and Human Services (HHS) programs, as well as the health and welfare of beneficiaries served by those programs. This statutory mission is carried out through a nationwide network of audits, investigations, and inspections conducted by the following operating components: Office of Audit Services The Office of Audit Services (OAS) provides auditing services for HHS, either by conducting audits with its own audit resources or by overseeing audit work done by others. Audits examine the performance of HHS programs and/or its grantees and contractors in carrying out their respective responsibilities and are intended to provide independent assessments of HHS programs and operations. These audits help reduce waste, abuse, and mismanagement and promote economy and efficiency throughout HHS. Office of Evaluation and Inspections The Office of Evaluation and Inspections (OEI) conducts national evaluations to provide HHS, Congress, and the public with timely, useful, and reliable information on significant issues. These evaluations focus on preventing fraud, waste, or abuse and promoting economy, efficiency, and effectiveness of departmental programs. To promote impact, OEI reports also present practical recommendations for improving program operations. -
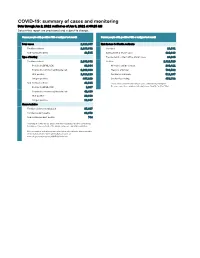
COVID-19: Summary of Cases and Monitoring Data Through Jun 2, 2021 Verified As of Jun 3, 2021 at 09:25 AM Data in This Report Are Provisional and Subject to Change
COVID-19: summary of cases and monitoring Data through Jun 2, 2021 verified as of Jun 3, 2021 at 09:25 AM Data in this report are provisional and subject to change. Cases: people with positive PCR or antigen test result Cases: people with positive PCR or antigen test result Total cases 2,329,867 Risk factors for Florida residents 2,286,332 Florida residents 2,286,332 Traveled 18,931 Non-Florida residents 43,535 Contact with a known case 920,896 Type of testing Traveled and contact with a known case 24,985 Florida residents 2,286,332 Neither 1,321,520 Positive by BPHL/CDC 83,364 No travel and no contact 280,411 Positive by commercial/hospital lab 2,202,968 Travel is unknown 733,532 PCR positive 1,819,119 Contact is unknown 511,267 Antigen positive 467,213 Contact is pending 459,732 Non-Florida residents 43,535 Travel can be unknown and contact can be unknown or pending for Positive by BPHL/CDC 1,037 the same case, these numbers will sum to more than the "neither" total. Positive by commercial/hospital lab 42,498 PCR positive 29,688 Antigen positive 13,847 Characteristics Florida residents hospitalized 95,607 Florida resident deaths 36,973 Non-Florida resident deaths 744 Hospitalized counts include anyone who was hospitalized at some point during their illness. It does not reflect the number of people currently hospitalized. More information on deaths identified through death certificate data is available on the National Center for Health Statistics website at www.cdc.gov/nchs/nvss/vsrr/COVID19/index.htm. -

Diesonnenküeste
aril – may 201 DieSonnen Küeste A quarterly publication from the Suncoast Chapter of the BMW Car Club of America I n this ssue “Hop-On – Hop-Off” – Carolina’s Driving Tour BMW CCA...The Next 50 Years. ADMINISTRATION Stan Dale (305) 218-1104 [email protected] Frank Mann (727) 254-9723 [email protected] Post Office Box 172215 Tampa, Florida 33618 Stella Metz [email protected] Carol Villar (813) 568-3572 [email protected] Michael Clark [email protected] Christopher Gandees [email protected] Russ Garvey (813) 230-5705 President [email protected] Steve Johnson Exec Vice President Dave Uman [email protected] Eddy Funahashi South Atlantic Region VP Dennis Johnston J. Dwayne Mosley [email protected] Die Sonnen Küeste is the official newsletter of the BMW Car Club of America – Suncoast Chapter. It is a quarterly publication intended to Dave Uman / Russ Garvey serve as a means of communication highlighting events and members of [email protected] the chapter. No portion in part or whole may be reproduced without the written permission of the Florida Suncoast BMW CCA Board of Directors. (Temp) Stan Dale All submissions are subject to editing for space constraints, style, and [email protected] editorial consistency and must include name and phone number for consideration. All photos, articles and letters should be submitted to Carol Villar the Newsletter Editor at [email protected] [email protected] (813)586-3572 Any address or email changes should be