Estradiol As a Male Hormone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sex Hormones Related Ocular Dryness in Breast Cancer Women
Journal of Clinical Medicine Review Sex Hormones Related Ocular Dryness in Breast Cancer Women Antonella Grasso 1, Antonio Di Zazzo 2,* , Giuseppe Giannaccare 3 , Jaemyoung Sung 4 , Takenori Inomata 4 , Kendrick Co Shih 5 , Alessandra Micera 6, Daniele Gaudenzi 2, Sara Spelta 2 , Maria Angela Romeo 7, Paolo Orsaria 1, Marco Coassin 2 and Vittorio Altomare 1 1 Breast Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (A.G.); [email protected] (P.O.); [email protected] (V.A.) 2 Ophthalmology Operative Complex Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (D.G.); [email protected] (S.S.); [email protected] (M.C.) 3 Department of Ophthalmology, University Magna Graecia of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of Ophthalmology, School of Medicine, Juntendo University, 1130033 Tokyo, Japan; [email protected] (J.S.); [email protected] (T.I.) 5 Department of Ophthalmology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; [email protected] 6 Research and Development Laboratory for Biochemical, Molecular and Cellular Applications in Ophthalmological Sciences, IRCCS–Fondazione Bietti, 00198 Rome, Italy; [email protected] 7 School of Medicine, Humanitas University, 20089 Milan, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-06225418893; Fax: +39-9622541456 Abstract: Background: Dry eye syndrome (DES) is strictly connected to systemic and topical sex hor- mones. Breast cancer treatment, the subsequent hormonal therapy, the subsequent hyperandrogenism and the early sudden menopause, may be responsible for ocular surface system failure and its clinical Citation: Grasso, A.; Di Zazzo, A.; manifestation as dry eye disease. -
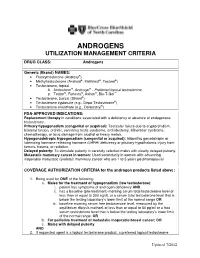
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

Background Briefing Document from the Consortium of Sponsors for The
BRIEFING BOOK FOR Pediatric Advisory Committee (PAC) Prepared by Alan Rogol, M.D., Ph.D. Prepared for Consortium of Sponsors Meeting Date: April 8th, 2019 TABLE OF CONTENTS LIST OF FIGURES ................................................... ERROR! BOOKMARK NOT DEFINED. LIST OF TABLES ...........................................................................................................................4 1. INTRODUCTION AND BACKGROUND FOR THE MEETING .............................6 1.1. INDICATION AND USAGE .......................................................................................6 2. SPONSOR CONSORTIUM PARTICIPANTS ............................................................6 2.1. TIMELINE FOR SPONSOR ENGAGEMENT FOR PEDIATRIC ADVISORY COMMITTEE (PAC): ............................................................................6 3. BACKGROUND AND RATIONALE .........................................................................7 3.1. INTRODUCTION ........................................................................................................7 3.2. PHYSICAL CHANGES OF PUBERTY ......................................................................7 3.2.1. Boys ..............................................................................................................................7 3.2.2. Growth and Pubertal Development ..............................................................................8 3.3. AGE AT ONSET OF PUBERTY.................................................................................9 3.4. -

Serum Androgen Profiles in Women with Premature Ovarian Insufficiency: a Systematic Review and Meta-Analysis
Menopause: The Journal of The North American Menopause Society Vol. 26, No. 1, pp. 78-93 DOI: 10.1097/GME.0000000000001161 ß 2018 The Author(s). Published by Wolters Kluwer Health, Inc. on behalf of The North American Menopause Society. Serum androgen profiles in women with premature ovarian insufficiency: a systematic review and meta-analysis Midhun Soman, MS,1 Li-Cong Huang, MD,1 Wen-Hui Cai, MS,1 Jun-Bi Xu, MS,1 Jun-Yao Chen, MD,1 Ren-Ke He, MS,1 Heng-Chao Ruan, MS,1,2,3 Xiang-Rong Xu, MD,1,2,3 Zhi-Da Qian, MD,1,2,3,4 and Xiao-Ming Zhu, MD, PhD1,2,3 Abstract Objective: This meta-analysis aims to investigate serum androgen profiles (testosterone, dehydroepiandroster- one sulfate, androstenedione, and sex hormone-binding globulin) in women with premature ovarian failure and to establish if there is evidence of diminished androgen levels in these women. Methods: Various Internet sources of PubMed, Cochrane library, and Medline were searched systematically until February, 2018. Out of a pool of 2,461 studies, after applying the inclusion/exclusion criterion, 14, 8, 10, and 9 studies were chosen for testosterone, dehydroepiandrosterone sulfate, androstenedione, and sex hormone-binding globulin, respectively, for this meta-analysis. The effect measure was the standardized mean difference with 95% confidence interval (95% CI) in a random-effects model. Results: The testosterone concentrations in premature ovarian insufficiency were compared with fertile controls: stamdard mean difference (IV, random, 95% CI) À0.73 [À0.99, À0.46], P value < 0.05. The dehydroepiandrosterone sulfate concentrations in premature ovarian insufficiency compared to fertile controls: standard mean difference (IV, random, 95% CI) À0.65 [À0.92, À0.37], P value < 0.05. -

Actions of Vasoactive Intestinal Peptide on the Rat Adrenal Zona Glomerulosa
51 Actions of vasoactive intestinal peptide on the rat adrenal zona glomerulosa J P Hinson, J R Puddefoot and S Kapas1 Molecular and Cellular Biology Section, Division of Biomedical Sciences, St Bartholomew’s and The Royal London School of Medicine and Dentistry, Queen Mary and Westfield College, Mile End Road, London E1 4NS, UK 1Oral Diseases Research Centre, St Bartholomew’s and The Royal London School of Medicine and Dentistry, 2 Newark Street, London E1 2AT, UK (Requests for offprints should be addressed to J P Hinson) Abstract Previous studies, by this group and others, have shown that The response to VIP in adrenals obtained from rats fed vasoactive intestinal peptide (VIP) stimulates aldosterone a low sodium diet was also investigated. Previous studies secretion, and that the actions of VIP on aldosterone have found that adrenals from animals on a low sodium secretion by the rat adrenal cortex are blocked by â diet exhibit increased responsiveness to VIP. Specific VIP adrenergic antagonists, suggesting that VIP may act by binding sites were identified, although the concentration the local release of catecholamines. The present studies or affinity of binding sites in the low sodium group was not were designed to test this hypothesis further, by measur- significantly different from the controls. In the low sodium ing catecholamine release by adrenal capsular tissue in group VIP was found to increase catecholamine release to response to VIP stimulation. the same extent as in the control group, however, in Using intact capsular tissue it was found that VIP caused contrast to the control group, the adrenal response to VIP a dose-dependent increase in aldosterone secretion, with a was not altered by adrenergic antagonists in the low concomitant increase in both adrenaline and noradrenaline sodium group. -

Affect Breast Cancer Risk
HOW HORMONES AFFECT BREAST CANCER RISK Hormones are chemicals made by the body that control how cells and organs work. Estrogen is a female hormone made mainly in the ovaries. It’s important for sexual development and other body functions. From your first monthly period until menopause, estrogen stimulates normal breast cells. A higher lifetime exposure to estrogen may increase breast cancer risk. For example, your risk increases if you start your period at a young age or go through menopause at a later age. Other hormone-related risks are described below. Menopausal hormone therapy Pills Menopausal hormone therapy (MHT) is The U.S. Food and Drug Administration also known as postmenopausal hormone (FDA) recommends women use the lowest therapy and hormone replacement dose that eases symptoms for the shortest therapy. Many women use MHT pills to time needed. relieve hot flashes and other menopausal Any woman currently taking or thinking symptoms. MHT should be used at the Birth control about taking MHT pills should talk with her lowest dose and for the shortest time pills (oral doctor about the risks and benefits. contraceptives) needed to ease menopausal symptoms. Long-term use can increase breast cancer Vaginal creams, suppositories Current or recent use risk and other serious health conditions. and rings of birth control pills There are 2 main types of MHT pills: slightly increases breast Vaginal forms of MHT do not appear to cancer risk. However, estrogen plus progestin and estrogen increase the risk of breast cancer. However, this risk is quite small alone. if you’ve been diagnosed with breast cancer, vaginal estrogen rings and suppositories are because the risk of Estrogen plus progestin MHT breast cancer for most better than vaginal estrogen creams. -

Detectx® Serum 17Β-Estradiol Enzyme Immunoassay Kit
DetectX® Serum 17β-Estradiol Enzyme Immunoassay Kit 1 Plate Kit Catalog Number KB30-H1 5 Plate Kit Catalog Number KB30-H5 Species Independent Sample Types Validated: Multi-Species Serum and Plasma Please read this insert completely prior to using the product. For research use only. Not for use in diagnostic procedures. www.ArborAssays.com KB30-H WEB 210308 TABLE OF CONTENTS Background 3 Assay Principle 4 Related Products 4 Supplied Components 5 Storage Instructions 5 Other Materials Required 6 Precautions 6 Sample Types 7 Sample Preparation 7 Reagent Preparation 8 Assay Protocol 9 Calculation of Results 10 Typical Data 10-11 Validation Data Sensitivity, Linearity, etc. 11-13 Samples Values and Cross Reactivity 14 Warranty & Contact Information 15 Plate Layout Sheet 16 ® 2 EXPECT ASSAY ARTISTRY KB30-H WEB 210308 BACKGROUND 17β-Estradiol, C18H24O2, also known as E2 or oestradiol (1, 3, 5(10)-Estratrien-3, 17β-diol) is a key regulator of growth, differentiation, and function in a wide array of tissues, including the male and female reproductive tracts, mammary gland, brain, skeletal and cardiovascular systems. The predominant biological effects of E2 are mediated through two distinct intracellular receptors, ERα and ERβ, each encoded by unique genes possessing the functional domain characteristics of the steroid/thyroid hormone superfamily of nuclear receptors1. ERα is the predominant form expressed in the breast, uterus, cervix, and vagina. ERβ exhibits a more limited pattern and is primarily expressed in the ovary, prostate, testis, spleen, lung, hypothalamus, and thymus2. Estradiol also influences bone growth, brain development and maturation, and food intake3, and it is also critical in maintaining organ functions during severe trauma4,5. -

A Guide to Feminizing Hormones – Estrogen
1 | Feminizing Hormones A Guide to Feminizing Hormones Hormone therapy is an option that can help transgender and gender-diverse people feel more comfortable in their bodies. Like other medical treatments, there are benefits and risks. Knowing what to expect will help us work together to maximize the benefits and minimize the risks. What are hormones? Hormones are chemical messengers that tell the body’s cells how to function, when to grow, when to divide, and when to die. They regulate many functions, including growth, sex drive, hunger, thirst, digestion, metabolism, fat burning & storage, blood sugar, cholesterol levels, and reproduction. What are sex hormones? Sex hormones regulate the development of sex characteristics, including the sex organs such as genitals and ovaries/testicles. Sex hormones also affect the secondary sex characteristics that typically develop at puberty, like facial and body hair, bone growth, breast growth, and voice changes. There are three categories of sex hormones in the body: • Androgens: testosterone, dehydroepiandrosterone (DHEA), dihydrotestosterone (DHT) • Estrogens: estradiol, estriol, estrone • Progestin: progesterone Generally, “males” tend to have higher androgen levels, and “females” tend to have higher levels of estrogens and progestogens. What is hormone therapy? Hormone therapy is taking medicine to change the levels of sex hormones in your body. Changing these levels will affect your hair growth, voice pitch, fat distribution, muscle mass, and other features associated with sex and gender. Feminizing hormone therapy can help make the body look and feel less “masculine” and more “feminine" — making your body more closely match your identity. What medicines are involved? There are different kinds of medicines used to change the levels of sex hormones in your body. -

Antiestrogenic Action of Dihydrotestosterone in Mouse Breast
Antiestrogenic action of dihydrotestosterone in mouse breast. Competition with estradiol for binding to the estrogen receptor. R W Casey, J D Wilson J Clin Invest. 1984;74(6):2272-2278. https://doi.org/10.1172/JCI111654. Research Article Feminization in men occurs when the effective ratio of androgen to estrogen is lowered. Since sufficient estrogen is produced in normal men to induce breast enlargement in the absence of adequate amounts of circulating androgens, it has been generally assumed that androgens exert an antiestrogenic action to prevent feminization in normal men. We examined the mechanisms of this effect of androgens in the mouse breast. Administration of estradiol via silastic implants to castrated virgin CBA/J female mice results in a doubling in dry weight and DNA content of the breast. The effect of estradiol can be inhibited by implantation of 17 beta-hydroxy-5 alpha-androstan-3-one (dihydrotestosterone), whereas dihydrotestosterone alone had no effect on breast growth. Estradiol administration also enhances the level of progesterone receptor in mouse breast. Within 4 d of castration, the progesterone receptor virtually disappears and estradiol treatment causes a twofold increase above the level in intact animals. Dihydrotestosterone does not compete for binding to the progesterone receptor, but it does inhibit estrogen-mediated increases of progesterone receptor content of breast tissue cytosol from both control mice and mice with X-linked testicular feminization (tfm)/Y. Since tfm/Y mice lack a functional androgen receptor, we conclude that this antiestrogenic action of androgen is not mediated by the androgen receptor. Dihydrotestosterone competes with estradiol for binding to the cytosolic estrogen receptor of mouse breast, […] Find the latest version: https://jci.me/111654/pdf Antiestrogenic Action of Dihydrotestosterone in Mouse Breast Competition with Estradiol for Binding to the Estrogen Receptor Richard W. -

EAU Pocket Guidelines on Male Hypogonadism 2013
GUIDELINES ON MALE HYPOGONADISM G.R. Dohle (chair), S. Arver, C. Bettocchi, S. Kliesch, M. Punab, W. de Ronde Introduction Male hypogonadism is a clinical syndrome caused by andro- gen deficiency. It may adversely affect multiple organ func- tions and quality of life. Androgens play a crucial role in the development and maintenance of male reproductive and sexual functions. Low levels of circulating androgens can cause disturbances in male sexual development, resulting in congenital abnormalities of the male reproductive tract. Later in life, this may cause reduced fertility, sexual dysfunc- tion, decreased muscle formation and bone mineralisation, disturbances of fat metabolism, and cognitive dysfunction. Testosterone levels decrease as a process of ageing: signs and symptoms caused by this decline can be considered a normal part of ageing. However, low testosterone levels are also associated with several chronic diseases, and sympto- matic patients may benefit from testosterone treatment. Androgen deficiency increases with age; an annual decline in circulating testosterone of 0.4-2.0% has been reported. In middle-aged men, the incidence was found to be 6%. It is more prevalent in older men, in men with obesity, those with co-morbidities, and in men with a poor health status. Aetiology and forms Male hypogonadism can be classified in 4 forms: 1. Primary forms caused by testicular insufficiency. 2. Secondary forms caused by hypothalamic-pituitary dysfunction. 164 Male Hypogonadism 3. Late onset hypogonadism. 4. Male hypogonadism due to androgen receptor insensitivity. The main causes of these different forms of hypogonadism are highlighted in Table 1. The type of hypogonadism has to be differentiated, as this has implications for patient evaluation and treatment and enables identification of patients with associated health problems. -

Degradation and Metabolite Formation of Estrogen Conjugates in an Agricultural Soil
Journal of Pharmaceutical and Biomedical Analysis 145 (2017) 634–640 Contents lists available at ScienceDirect Journal of Pharmaceutical and Biomedical Analysis j ournal homepage: www.elsevier.com/locate/jpba Degradation and metabolite formation of estrogen conjugates in an agricultural soil a,b b,∗ Li Ma , Scott R. Yates a Department of Environmental Sciences, University of California, Riverside, CA 92521, United States b Contaminant Fate and Transport Unit, U.S. Salinity Laboratory, Agricultural Research Service, United States Department of Agriculture, Riverside, CA 92507, United States a r t i c l e i n f o a b s t r a c t Article history: Estrogen conjugates are precursors of free estrogens such as 17ß-estradiol (E2) and estrone (E1), which Received 10 April 2017 cause potent endocrine disrupting effects on aquatic organisms. In this study, microcosm laboratory Received in revised form 11 July 2017 ◦ experiments were conducted at 25 C in an agricultural soil to investigate the aerobic degradation and Accepted 31 July 2017 metabolite formation kinetics of 17ß-estradiol-3-glucuronide (E2-3G) and 17ß-estradiol-3-sulfate (E2- Available online 1 August 2017 3S). The aerobic degradation of E2-3G and E2-3S followed first-order kinetics and the degradation rates were inversely related to their initial concentrations. The degradation of E2-3G and E2-3S was extraordi- Keywords: narily rapid with half of mass lost within hours. Considerable quantities of E2-3G (7.68 ng/g) and E2-3S Aerobic degradation 17ß-estradiol-3-glucuronide (4.84 ng/g) were detected at the end of the 20-d experiment, particularly for high initial concentrations. -

Diverse Pathomechanisms Leading to the Breakdown of Cellular Estrogen Surveillance and Breast Cancer Development: New Therapeutic Strategies
Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2014 Volume: 8 Drug Design, Development and Therapy Dovepress Running head verso: Suba Running head recto: Diverse pathomechanisms leading to breast cancer development open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DDDT.S70570 Open Access Full Text Article REVIEW Diverse pathomechanisms leading to the breakdown of cellular estrogen surveillance and breast cancer development: new therapeutic strategies Zsuzsanna Suba Abstract: Recognition of the two main pathologic mechanisms equally leading to breast cancer National Institute of Oncology, development may provide explanations for the apparently controversial results obtained by sexual Budapest, Hungary hormone measurements in breast cancer cases. Either insulin resistance or estrogen receptor (ER) defect is the initiator of pathologic processes and both of them may lead to breast cancer development. Primary insulin resistance induces hyperandrogenism and estrogen deficiency, but during these ongoing pathologic processes, ER defect also develops. Conversely, when estrogen resistance is the onset of hormonal and metabolic disturbances, initial counteraction is For personal use only. hyperestrogenism. Compensatory mechanisms improve the damaged reactivity of ERs; however, their failure leads to secondary insulin resistance. The final stage of both pathologic pathways is the breakdown of estrogen surveillance, leading to breast cancer development. Among pre- menopausal breast cancer cases, insulin resistance is the preponderant initiator of alterations with hyperandrogenism, which is reflected by the majority of studies suggesting a causal role of hyperandrogenism in breast cancer development. In the majority of postmenopausal cases, tumor development may also be initiated by insulin resistance, while hyperandrogenism is typi- cally coupled with elevated estrogen levels within the low postmenopausal hormone range.