Frequently Asked Questions from the Community on COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PART 3: Recommendations & Conclusion
CRAWLEY BASELINE CHARACTER ASSESSMENT Part 3: RECOMMENDATIONS & CONCLUSION 10 RecOMMenDatiOns & COnclUsiON Summary of recommendations The detailed analysis of the town centre, historic villages and thirteen New 10.1 INTRODUCTION Town neighbourhoods has revealed a number of areas that would benefit EDAW | AECOM were commissioned by Crawley Borough Council to from enhancement, additional protection or regeneration/redevelopment. undertaken a rapid baseline assessment of the character of present day This chapter pulls the findings together to identify priority areas across the Crawley comprising a desk top study, development of a rapid assessment borough which would benefit from further detailed study. toolkit, field assessments and photography, GIS survey and data capture and the production of a report. Three areas offer significant potential for enhancement or regeneration. These are the Town Centre, Broadfield / Bewbush, and on a smaller Eight strategic character areas covering the borough were identified scale the Three Bridges Station area (Refer to figure 31 for details of the comprising: locations). • Town Centre 10.1 Bewbush and Broadfield • Historic Settlements These neighbourhoods were built during the 1970s and contain a number of experimental housing layout styles which depart from the traditional • Pre New Town Expansion arrangement of streets and perimeter block development, and instead separate pedestrian and vehicle traffic, creating cul-de-sacs and semi-public • New Town Phase 1a amenity grassed spaces within the development block. The creation of • New Town Phase 1b poorly overlooked walkways, abundance of semi-public open space, parking courts and a lack of vehicle access to properties is a management burden • New Town Phase 2 / Expansion of Phase 1 and encourages anti-social behaviour. -

Crawley Business Directory - Carers Support West Sussex
09/11/2020 Carers Support West Sussex Crawley Business Directory - Carers Support West Sussex - Carers Support West Sussex - https://www.carerssupport.org.uk - Crawley Business Directory Posted By Laura Bird On February 17, 2020 @ 12:41 pm In | Comments Disabled Click this icon to display a print-friendly version of the page, then scroll down and select ‘Click here to print’ Name Address Telephone Website Offering Health and Wellbeing £10 discount Abrahams Road, 07707 Astara Therapies astaraholistic.co.uk on treatment Crawley 063843 price Hair and beauty £5 off per session; The Serene 16 Allyington Way, 07941 Serenebeauty.com Wednesday Beauty Room Crawley, RH10 7WA 089996 and Thursday 9am - 4pm Leisure and Recreation Card holders will be notified by Carers Support West The Hawth, Hawth The Hawth 01293 of exclusive Avenue, Crawley, hawth.co.uk Theatre 553636 special offers RH10 6YZ throughout the year (notifications will come via email only). 10% discount to carers on any CASUAL Pease Pottage Hill, 01293 K2 everyoneactive.com visits for gym Crawley, RH11 9BQ 585300 or swimming at K2 Crawley. Retail https://www.carerssupport.org.uk/crawley-business-directory/print/ 1/4 09/11/2020 Carers Support West Sussex Crawley Business Directory - Carers Support West Sussex Name Address Telephone Website Offering 07503 Mary Kay Online skincare and 387409 20% discount Skincare and marykay.co.uk cosmetic company (Caroline on purchases Cosmetics Phillips) 10% discount 12-14 Broadfield Kamsons on retail Barton, Crawley, 01293 Pharmacy - kamsons.co.uk items -

Witney Road, Furnace Green, Crawley, West Sussex, RH10 6GJ Offers in Excess of £450,000 Freehold
Witney Road, Furnace Green, Crawley, West Sussex, RH10 6GJ Offers in Excess of £450,000 Freehold in brief… Entrance hall with downstairs cloakroom Family bathroom Kitchen/breakfast room with integrated appliances Private 40’ x 24’ south west facing rear garden with access to garage Bright and spacious living/dining room Garage and driveway parking Master bedroom with large en-suite shower room and built-in wardrobes Spacia Amtico flooring throughout the ground floor Three further bedrooms good sized bedrooms Council Tax Band 'E' and EPC 'B' in more detail… outside and the location… A beautifully presented four-bedroom semi-detached Outside there is driveway parking leading to a single garage family home built by Barratt to their ‘Woodbridge’ and access to an attractive south west facing rear garden design, situated within a cul-de-sac location in the with paved patio abutting the rear of the property, the sought-after area of Furnace Green within a short walk remainder laid to lawn and the whole enclosed by wooden of Three Bridges station and Crawley town centre. panel fencing. The property, which offers spacious and versatile Internal viewings highly recommended. accommodation over three floors, comprises on the ground floor of an entrance hallway, downstairs cloakroom with low level WC and wash hand basin. Location The kitchen/breakfast room has a box bay window to The property stands on the favoured southern side of the front of the property and is fitted with an Crawley, close to Tilgate Forest with its selection of water attractive range of black high gloss wall and base units, sports, bridle paths, forest walks, golf course and close to sink unit, roll top work surfaces over, integrated gas Furnace Green shopping parade with its selection of hob and electric oven, part-tiled walls, integrated convenience stores, restaurants/takeaways, off-licence and dishwasher, fridge/freezer and washing machine. -

610 Bus Time Schedule & Line Route
610 bus time schedule & line map 610 Bewbush - Thomas Bennett School - Holy Trinity View In Website Mode School The 610 bus line (Bewbush - Thomas Bennett School - Holy Trinity School) has 3 routes. For regular weekdays, their operation hours are: (1) Bewbush: 3:10 PM (2) Crawley: 3:32 PM (3) Gossops Green: 8:05 AM Use the Moovit App to ƒnd the closest 610 bus station near you and ƒnd out when is the next 610 bus arriving. Direction: Bewbush 610 bus Time Schedule 11 stops Bewbush Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 3:10 PM Thomas Bennett School, Tilgate Tuesday 3:10 PM Southgate Avenue South, Tilgate Thatcher Close, Crawley Wednesday 3:10 PM Stadium, Broadƒeld Thursday 3:10 PM Friday 3:10 PM Coachmans Drive North, Broadƒeld Regents Close, Crawley Saturday Not Operational Broadƒeld Barton North, Broadƒeld Broadƒeld Barton, Broadƒeld 610 bus Info Pelham Drive, Broadƒeld Direction: Bewbush Pelham Drive, Crawley Stops: 11 Trip Duration: 11 min Breezehurst Drive East, Bewbush Line Summary: Thomas Bennett School, Tilgate, Southgate Avenue South, Tilgate, Stadium, Breezehurst Drive Central, Bewbush Broadƒeld, Coachmans Drive North, Broadƒeld, Broadƒeld Barton North, Broadƒeld, Broadƒeld Breezehurst Drive West, Bewbush Barton, Broadƒeld, Pelham Drive, Broadƒeld, Breezehurst Drive East, Bewbush, Breezehurst Drive Dorsten Square, Bewbush Central, Bewbush, Breezehurst Drive West, Bewbush, Dorsten Square, Bewbush Dorsten Place, Crawley Direction: Crawley 610 bus Time Schedule 12 stops Crawley Route Timetable: VIEW LINE -

Declarations of Interest
Declarations Of Interest Last Name First Name Role Interest Type Declared interest Provider Date incurred Date to Action taken to mitigate risk Adams Alan Director of Adult Social Care Nil Declaration 01/12/2020 Current (West Sussex County Council) Ansari Louise Lay Member (Patient and Public Outside Employment I am the Director of Communications at the Centre for Centre for Ageing Better 31/05/2016 Current Any conflicts relating to any of the Sussex Engagement) Ageing Better, a charitable foundation that works to ensure CCGs will be identified and managed as they everyone can enjoy later life. The Centre has an arise in line with CCG policy endowment and is a funder and grant giver; whilst it runs programmes of activity none of these are services in health or other sectors. Declarations of Partner holds some shares in Astra Zeneca Astra Zeneca 01/04/2020 Current Any conflicts relating to any of the Sussex Interest – Other CCGs will be identified and managed as they arise in line with CCG policy Banjoko Titilola Executive Managing Director Outside Employment Active engagement in Diaspora related activities and Better Health for Africa 05/05/2020 Current Any conflicts relating to any of the Sussex (Brighton and Hove) member of Better Health for Africa CCGs will be identified and managed as they arise in line with CCG policy Declarations of Trustee of Tropical Health and Education Trust Tropical Health and Education Trust 01/05/2018 Current Any conflicts relating to any of the Sussex Interest – Other CCGs will be identified and managed -

The West Sussex (Electoral Changes) Order 2016
Draft Order laid before Parliament under section 59(9) of the Local Democracy, Economic Development and Construction Act 2009; draft to lie for forty days pursuant to section 6(1) of the Statutory Instruments Act 1946, during which period either House of Parliament may resolve that the Order be not made. DRAFT STATUTORY INSTRUMENTS 2016 No. LOCAL GOVERNMENT, ENGLAND The West Sussex (Electoral Changes) Order 2016 Made - - - - Coming into force in accordance with article 1(2), (3), (4) and (5) Under section 58(4) of the Local Democracy, Economic Development and Construction Act 2009(a) (“the Act”), the Local Government Boundary Commission for England( b) (“the Commission”) published a report dated August 2016 stating its recommendations for changes to the electoral arrangements for the county of West Sussex. The Commission has decided to give effect to those recommendations. A draft of the instrument has been laid before each House of Parliament, a period of forty days has expired since the day on which it was laid and neither House has resolved that the instrument be not made. The Commission makes the following Order in exercise of the power conferred by section 59(1) of the Act. Citation and commencement 1. —(1) This Order may be cited as the West Sussex (Electoral Changes) Order 2016. (2) This article and article 2 come into force on the day after the day on which this Order is made. (3) Article 3 comes into force— (a) for the purpose of proceedings preliminary, or relating, to the election of councillors, on the day after the day on which it is made; (b) for all other purposes, on the ordinary day of election of councillors in England and Wales(c) in 2017. -
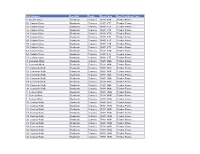
Flat Number Locality Town Post Code Non Traditional Type 3 Colwyn
Flat Number Locality Town Post Code Non Traditional Type 3 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 16 Colwyn Close Bewbush Crawley RH11 8TF Timber Frame 27 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 32 Colwyn Close Bewbush Crawley RH11 8TF Timber Frame 33 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 38 Colwyn Close Bewbush Crawley RH11 8TF Timber Frame 47 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 57 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 59 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 63 Colwyn Close Bewbush Crawley RH11 8TS Timber Frame 64 Colwyn Close Bewbush Crawley RH11 8TF Timber Frame 74 Colwyn Close Bewbush Crawley RH11 8TF Timber Frame 4 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 9 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 12 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 14 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 15 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 16 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 27 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 35 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 40 Coxcomb Walk Bewbush Crawley RH11 8BA Timber Frame 3 Curteys Walk Bewbush Crawley RH11 8NN Timber Frame 6 Curteys Walk Bewbush Crawley RH11 8NP Timber Frame 7 Curteys Walk Bewbush Crawley RH11 8NN Timber Frame 10 Curteys Walk Bewbush Crawley RH11 8NP Timber Frame 11 Curteys Walk Bewbush Crawley RH11 8NN Timber Frame 12 Curteys Walk Bewbush Crawley RH11 8NP Timber Frame 13 Curteys Walk Bewbush Crawley RH11 8NN Timber Frame -

14 the Chase, Furnace Green, Crawley, West Sussex, RH10 6HW £475,000
14 The Chase, Furnace Green, Crawley, West Sussex, RH10 6HW £475,000 Four double bedroom family home Double glazing Garage & parking Desirable cul-de-sac location Recently re-roofed Wonderful size private garden Potential to extend STPP Requires some updating EPC rating C Property Description Homes Partnership is delighted to offer for sale this detached family home situated in a sought after cul-de-sac in Furnace Green just a 20 minute w alk from Three Bridges mainline station. The property has recently been re-roofed and has many benefits including a dow nstairs cloakroom, tw o reception rooms, four double bedrooms, double glazing, gas fired central heating, off road parking for two vehicles, an integral garage and a southerly facing rear garden. In our opinion the property offers scope for an extension (subject to planning permission) and requires some updating providing an ideal opportunity to create your perfect home. Property in this location are highly sought after and an early view ing is highly recommended. Double glazed front door and w indow leading to: ENTRANCE HALL Stairs to the first floor w ith understairs cupboard. Radiator. Doors to lounge, dining room, kitchen and: CLOAKROOM White suite comprising a low level WC. Wall mounted w ash hand basin. Radiator. Opaque double glazed window to the front. LOUNGE 18' 5" x 11' 5" (5.61m x 3.48m) approximate. Double glazed w indow and French doors leading to a lean-to at the rear. Virgin Media point. Radiator. Opening to: DINING ROOM 12' 0" x 9' 5" (3.66m x 2.87m) approximate. -
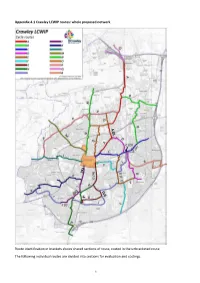
Appendix 4.1 Crawley LCWIP Routes: Whole Proposed Network
Appendix 4.1 Crawley LCWIP routes: whole proposed network Route identification in brackets shows shared sections of route, costed in the unbracketed route. The following individual routes are divided into sections for evaluation and costings. 1 LCWIP 2020 cycle routes A Gatwick Airport to town centre via Manor Royal and Northgate (joins route D) B Pound Hill to Manor Royal via Forge Wood C Copthorne to town centre via Three Bridges (limited to Pound Hill within Crawley boundary, joins route D) D Maidenbower to Manor Royal via Three Bridges (joins routes C and A) E Maidenbower to town centre via Furnace Green (joins routes F and I) F Tilgate Park to town centre via Furnace Green (joins routes E and I) G Tilgate to town centre (extended to K2, joins route I) H Pease Pottage to town centre via K2/Tilgate (joins route G) I Bewbush to Three Bridges via Broadfield & Tilgate Nature Centre (joins routes J, F and G) J Broadfield to town centre (joins routes I, H and K) K Kilnwood Vale to town centre (joins route J) L Ifield to town centre M Ifield Avenue to town centre N Lowfield Heath to town centre (subsequently split into a separate route O) O Manor Royal (west) to town centre P Ifield to Manor Royal via Langley Green Q Gatwick Airport to Horley (not developed within this LCWIP) R Worth Way (not developed within this LCWIP) Route proposals follow. 2 Appendix 4.1 Crawley LCWIP routes: A – Gatwick Airport to town centre via Manor Royal (and Northgate) Currently more than 14,500 Gatwick Airport employees drive to work and over half the workforce live in Crawley. -

Furnace Green £300,000 Guide Crawley, West Sussex Freehold Guide Price £300,000-£310,000
Furnace Green £300,000 Guide Crawley, West Sussex Freehold Guide Price £300,000-£310,000 • Terraced House • Conservatory • Summer House • Three Bedrooms • Kitchen • G/C/H Via Radiators • Lounge • Utility Room • Large Boarded Loft Forest View, Furnace Green, Crawley, West Sussex, RH10 6PJ A three bedroom terraced house situated in the desirable neighborhood of Furnace Green. The spacious lounge is drenched in natural light from the dual aspect windows. There is a separate kitchen which has an opening to a handy utility room. There is a vast conservatory - just the place to relax with a light infused view or use as a dining room and the underfloor heating enables it to be used all year around. On the first floor there are 3 well proportioned bedrooms, a stylish bathroom and a separate w.c. A staircase from the landing leads to a large boarded loft with a velux window. Externally there is an attractive rear garden with astro turf. It presents itself as the ideal place to dine alfresco with a barbecue and the summer house comes complete with a bar so if you love entertaining you can invite friends over. The property comes complete with G/C/H via radiators and double glazing. Forest View borders the stunning Tilgate forest, its public golf course and Gainsborough playing fields. The Oaks Primary/Junior school is within 400m, which was rated good by Ofsted in 2012. Entrance Hallway 2.74m x 1.83m (9' x 6') Lounge Kitchen 3.96m x 3m (13' x 9' 10") Utility 2.36m x 1.93m (7' 9" x 6' 4") Conservatory 3.61m x 2.59m (11' 10" x 8' 6") Landing 3.2m x 0.79m (10' 6" x 2' 7") Bedroom 1 3.3m x 3.02m (10' 10" x 9' 11") Bedroom 2 3.1m x 2.77m (10' 2" x 9' 1") Bedroom 3 2.51m x 2.36m (8' 3" x 7' 9") Bathroom 1.65m x 1.65m (5' 5" x 5' 5") W.C. -

Aroundgatwick.Com LOCAL HOTELS and GUEST HOUSES FURTHER
TRAIN SERVICES TAXIS CAR RENTAL First Capital Connect Key Arrive in style Step out of the airport and straight into a rental Connecting services car if you are looking for a fast, flexible and To Brighton One of the fastest ways, door to door, value for money way of reaching your final Journey time: 27 minutes anywhere in the UK. destination, or anywhere else you want to go. Frequency: Up to 4 an hour Operates: Daily To London Save up to 20% on return journeys by City car, executive saloon, 4x4 or MPV - a range From Gatwick First 04:52 Last 23:41 visiting our website gatwickairport.com of rental providers conveniently located at each From Brighton First 05:10 Last 23:37 or call on 01293 567700 terminal can supply you with whatever vehicle East Croydon is required. Southern Coulsdon South To Crawley, Horsham, Haywards Heath, Horley and East Croydon Merstham Journey time: 3-20mins Operates: Daily Redhill From Gatwick First 00:38 Last 23:38 Earlswood From Crawley First 05:29 Last 23:59 From Horley First 00:31 Last 23:53 Salfords From East Croydon First 00:06 Last 23:53 Horley Monday to Saturday daytime frequencies are shown. Train times may vary, see operator Connect Capital First AIRPORT CARS timetable for full information. Journey times are approximate. Information accurate at time of Southern publication July 2012. Subject to change. LOCAL HOTELS AND GUEST HOUSES Local hotels and guest houses run shuttle buses from: Gatwick Airport South Terminal bus stops 9 & 10 North Terminal 8 9 Three Bridges bus stops & Littlehaven Ileld Near to these stops are lists of these hotels with contact telephone numbers. -

Manor Royal Business District County Oak Northgate
R O A WH J Y E E C W D V CHA N I E I T Y R N R B R E W D D R O E L LWO D R N N T OA S A Superstores N O R R Northgate O O R G WA E N O IN Y I D E T M K U H D E R A L RO T F C L BARN P I L T R D COUNTY D A N Heathyground C S OA Primary SchoolA D 21 E O A D L FIELD ROAD ATW R A L Wood G I N C O OAK A E R W ATE COPTHORNE A G Y OR D N N C TS WY FLEMING WAY MA THE DRIVE A T O AD H C BE O A O R RL U The O W NT Forge O E D O Y OROUGH ROAD D O Larches B R R AK Sussex Manor Wood M N Y O N A METCA W D Y County Oak O CR R D A Business Park A WA Y C O 4 E O N DL L 26 R O L R A O OOLB F Retail Park A TH L P O W K B O A Y C W D R C C E D Y ST Crawley W A MEAD RD A r I U E C O IL a N R OBBLES A EY NE Cherry Lane W w W E O V P R A F t T A L N O OA L e A W DCophall S Y T Outdoor A E r G E R T ' L Leisure C W BOUNDA E s W TILGATE T A LD E B T D Wood NN Sports Pitch E LVIN LAN CR E I O Willoughby Fields Crawley KE ON r F L B M o UE FI F N IE I E A Park E o AV L I Outdoor Sports Pitch Household Waste R Y TO D AP R 21 k E A L D O A PLE F KENM W A R A A A W and Recycling Centre D CR Junction 10 A V D R O FIELD D A O N M E METCAL AD F N R N Y Y Summersvere ERN OW O N WA C D U JELVI K T R C E E O EAD Cycle Track and O I Wood 1 RN F A W 01 O W D T W W A2 H T O D Playing Field A P ME A NES Western L N A Y G O D A C L W O K O Playing Field O O H IL R Langley Green Tinsley Lane RD T N Crawters TONS DRIVE E D T L Crawley Y CH MANOR ROYAL RA C I L M Hospital G O E F IFIE Outdoor L O E E I E Brook C S A L E L R HAYWARDS N I D RY E E E E D Crawley L S U A D N A D V