Pharmacology of MDMA- and Amphetamine-Like New Psychoactive Substances
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recommended Methods for the Identification and Analysis of Synthetic Cathinones in Seized Materialsd
Recommended methods for the Identification and Analysis of Synthetic Cathinones in Seized Materials (Revised and updated) MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Photo credits:UNODC Photo Library; UNODC/Ioulia Kondratovitch; Alessandro Scotti. Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Synthetic Cathinones in Seized Materials (Revised and updated) MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2020 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/49/REV.1 Original language: English © United Nations, March 2020. All rights reserved, worldwide. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. -

Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation In
Graduate Physical and Life Sciences PhD Pharmacology Abstract ID# 1081 Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation in Drug Abuse? Fleischer, Lisa M; Tamashunas, Nina and Miller, Gregory M Addiction Sciences Laboratory, Northeastern University, Boston MA 02115 Abstract Discovered in 2001, Trace Amine Associated Receptor 1 (TAAR1) is a direct target of Data and Results amphetamine, methamphetamine and MDMA. It is expressed in the brain reward circuity and modulates dopamine transporter function and dopamine neuron firing rates. Newly-developed compounds that specifically target TAAR1 have recently been investigated in animal models In addition to brain, TAAR1 is expressed in immune cells METH promotes PKA and PKC Phosphorylation through TAAR1 as candidate therapeutics for methamphetamine, cocaine and alcohol abuse. These studies • We treated HEK/TAAR1 cells and HEK293 involving classic behavioral measures of drug response, as well as drug self-administration, Rhesus and Human cells with vehicle or METH, with and without strongly implicate TAAR1 as a potential therapeutic target for the treatment of addiction. In activators and inhibitors of PKA and PKC. addition to its central actions, we demonstrated that TAAR1 is upregulated in peripheral blood Cells Lines mononuclear cells (PBMC) and B cells following immune activation, and that subsequent • We performed Western blotting experiments to activation of TAAR1 by methamphetamine stimulates cAMP, similar to the function of measure levels of phospho-PKA and phospho- adenosine A2 receptors which are also present in immune cells and play a critical role in the PKC. immune response. Here, we are investigating the relationship between TAAR1 and the • We found that specific activators of PKA and adenosine A2 receptor at the level of cellular signaling and receptor dimerization. -
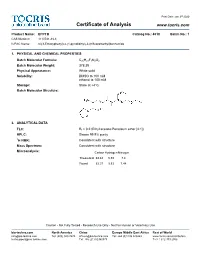
Certificate of Analysis
Print Date: Jan 3rd 2020 Certificate of Analysis www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide 1. PHYSICAL AND CHEMICAL PROPERTIES Batch Molecular Formula: C20H21F3N2O2 Batch Molecular Weight: 378.39 Physical Appearance: White solid Solubility: DMSO to 100 mM ethanol to 100 mM Storage: Store at +4°C Batch Molecular Structure: 2. ANALYTICAL DATA TLC: Rf = 0.2 (Ethyl acetate:Petroleum ether [4:1]) HPLC: Shows 99.9% purity 1H NMR: Consistent with structure Mass Spectrum: Consistent with structure Microanalysis: Carbon Hydrogen Nitrogen Theoretical 63.48 5.59 7.4 Found 63.37 5.53 7.44 Caution - Not Fully Tested • Research Use Only • Not For Human or Veterinary Use bio-techne.com North America China Europe Middle East Africa Rest of World [email protected] Tel: (800) 343 7475 [email protected] Tel: +44 (0)1235 529449 www.tocris.com/distributors [email protected] Tel: +86 (21) 52380373 Tel:+1 612 379 2956 Print Date: Jan 3rd 2020 Product Information www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide Description: Storage: Store at +4°C Trace amine 1 (TA ) receptor antagonist/inverse agonist; 1 Solubility & Usage Info: exhibits a higher potency at the mouse TA1 receptor than the rat DMSO to 100 mM and human TA150 receptors (IC values are 27.5, 4539 and 7487 ethanol to 100 mM nM, respectively). -

Quantification of Drugs of Abuse in Municipal Wastewater Via SPE and Direct Injection Liquid Chromatography Mass Spectrometry
Anal Bioanal Chem (2010) 398:2701–2712 DOI 10.1007/s00216-010-4191-9 ORIGINAL PAPER Quantification of drugs of abuse in municipal wastewater via SPE and direct injection liquid chromatography mass spectrometry Kevin J. Bisceglia & A. Lynn Roberts & Michele M. Schantz & Katrice A. Lippa Received: 2 June 2010 /Revised: 30 August 2010 /Accepted: 2 September 2010 /Published online: 24 September 2010 # US Government 2010 Abstract We present an isotopic-dilution direct injection 50 ng/L. We also present a modified version of this method reversed-phase liquid chromatography–tandem mass spec- that incorporates solid-phase extraction to further enhance trometry method for the simultaneous determination of 23 sensitivity. The method includes a confirmatory LC separa- drugs of abuse, drug metabolites, and human-use markers in tion (selected by evaluating 13 unique chromatographic municipal wastewater. The method places particular emphasis phases) that has been evaluated using National Institute of on cocaine; it includes 11 of its metabolites to facilitate Standards and Technology Standard Reference Material 1511 assessment of routes of administration and to enhance the Multi-Drugs of Abuse in Freeze-Dried Urine. Seven analytes accuracy of estimates of cocaine consumption. Four opioids (ecgonine methyl ester, ecgonine ethyl ester, anhydroecgo- (6-acetylmorphine, morphine, hydrocodone, and oxycodone) nine methyl ester, m-hydroxybenzoylecgonine, p-hydroxy- are also included, along with five phenylamine drugs benzoyl-ecgonine, ecgonine, and anhydroecgonine) were (amphetamine, methamphetamine, 3,4-methylenedioxy- detected for the first time in a wastewater sample. methamphetamine, methylbenzodioxolyl-butanamine, and 3,4-methylenedioxy-N-ethylamphetamine) and two human- Keywords Wastewater . Illicit drugs . Urinary metabolites . use markers (cotinine and creatinine). -

Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission
The Journal of Neuroscience, October 14, 2015 • 35(41):14057–14069 • 14057 Neurobiology of Disease Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission Alexandra Alvarsson,1* Xiaoqun Zhang,1* Tiberiu L Stan,1 Nicoletta Schintu,1 Banafsheh Kadkhodaei,2 Mark J. Millan,3 Thomas Perlmann,2,4 and Per Svenningsson1 1Department of Clinical Neuroscience, Center for Molecular Medicine, Karolinska Institutet, SE-17176 Stockholm, Sweden, 2Ludwig Institute for Cancer Research, SE-17177 Stockholm, Sweden, 3Pole of Innovation in Neuropsychiatry, Institut de Recherches Servier, Centre de Recherches de Croissy, Paris 87290, France, and 4Department of Cell and Molecular Biology, Karolinska Institutet, SE-17177 Stockholm, Sweden Parkinson’s disease (PD) is a movement disorder characterized by a progressive loss of nigrostriatal dopaminergic neurons. Restoration of dopamine transmission by L-DOPA relieves symptoms of PD but causes dyskinesia. Trace Amine-Associated Receptor 1 (TAAR1) modulates dopaminergic transmission, but its role in experimental Parkinsonism and L-DOPA responses has been neglected. Here, we report that TAAR1 knock-out (KO) mice show a reduced loss of dopaminergic markers in response to intrastriatal 6-OHDA administra- tion compared with wild-type (WT) littermates. In contrast, the TAAR1 agonist RO5166017 aggravated degeneration induced by intra- striatal6-OHDAinWTmice.Subchronic L-DOPAtreatmentofTAAR1KOmiceunilaterallylesionedwith6-OHDAinthemedialforebrain bundle resulted in more pronounced rotational behavior and dyskinesia than in their WT counterparts. The enhanced behavioral sensitization to L-DOPA in TAAR1 KO mice was paralleled by increased phosphorylation of striatal GluA1 subunits of AMPA receptors. Conversely, RO5166017 counteracted both L-DOPA-induced rotation and dyskinesia as well as AMPA receptor phosphorylation. -
2015-02 Toxicology Rapid Testing Panel
SOUTH CAROLINA LAW ENFORCEMENT DIVISION NIKKI R. HALEY MARK A. KEEL Governor Chief FORENSIC SERVICES LABORATORY CUSTOMER NOTICE 2015-02 REGARDING TOXICOLOGY RAPID TESTING PANEL August 12, 2015 This notice is to inform the Coroners of South Carolina of a new testing panel available through the SLED Toxicology Department. On Monday, August 17th, the Toxicology Department will begin offering both a Rapid Testing Panel in addition to the already available Expanded Testing Panel. This Rapid Testing Panel is to be utilized in cases where the Expanded Testing Panel is not warranted, specifically where a cause of death has already been established. The Rapid Testing Panel will consist of volatiles analysis, to include, ethanol, acetone, isopropanol and methanol, drug screens, and drug confirmation/quantitation of positive screens. The cases assigned to the Rapid Testing Panel will have an expedited turnaround time. Targeted turn around times will be two weeks for negative cases and six weeks or less for positive cases. While every effort will be made to adhere to these time frames, additional time may be required on occasion due to the nature of postmortem samples. Submitters will be notified if there is a problem with a particular sample. Please see attachment regarding specifically which substances are covered by the Rapid Testing Panel and the Expanded Testing Panel. As always, a detailed case history and list of drugs suspected is appreciated. Rapid Panel and Expanded Panel will be choices available in iLAB. Please contact Lt. Dustin Smith (803-896-7385) with additional questions. ALI-359-T An Accredited Law Enforcement Agency P.O. -

Belviq® (Lorcaserin) Patient Information
Belviq® (lorcaserin) Patient Information Who Is Belviq For? Belviq is a medication for chronic weight management. It is for people with overweight and weight-related conditions or obesity. It is meant to be used together with a lifestyle therapy regimen involving a reduced calorie diet and increased physical activity. How Does Belviq Work? Belviq works in the brain as an appetite suppressant. Who Should Not Take Belviq? Women who are pregnant, nursing, or planning to become pregnant. How Is Belviq Dosed? Belviq® (lorcaserin) Belviq XR® (lorcaserin extended release) Take one 10 mg tablet 2 times each day with Take one 20 mg tablet once daily with or or without food. without food. Is Belviq a Controlled Substance? Belviq is a federally controlled substance because it contains lorcaserin hydrochloride and may be abused or lead to drug dependence. Some states do not allow your doctor to prescribe more than one month at a time. Which Medications Might Not Be Safe to Use with Belviq? Belviq can affect how other medicines work in your body, and other medicines can affect how Belviq works. Tell your doctor about all the medicines and supplements you take, especially those used to treat depression, migraines, or other medical conditions, such as: • Triptans—used to treat migraine headache • Medicines used to treat mood, anxiety, psychotic or thought disorders, including tricyclics, lithium, selective serotonin uptake inhibitors (SSRIs), selective serotonin- norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), or antipsychotics • Cabergoline—used to treat a hormone imbalance involving prolactin • Linezolid—an antibiotic • Tramadol—an opioid pain reliever • Dextromethorphan—an over-the-counter medicine used to treat the common cold or cough • Over-the-counter supplements such as tryptophan or St. -
![3,4-Methylenedioxymethcathinone (Methylone) [“Bath Salt,” Bk-MDMA, MDMC, MDMCAT, “Explosion,” “Ease,” “Molly”] December 2019](https://docslib.b-cdn.net/cover/9290/3-4-methylenedioxymethcathinone-methylone-bath-salt-bk-mdma-mdmc-mdmcat-explosion-ease-molly-december-2019-259290.webp)
3,4-Methylenedioxymethcathinone (Methylone) [“Bath Salt,” Bk-MDMA, MDMC, MDMCAT, “Explosion,” “Ease,” “Molly”] December 2019
Drug Enforcement Administration Diversion Control Division Drug & Chemical Evaluation Section 3,4-Methylenedioxymethcathinone (Methylone) [“Bath salt,” bk-MDMA, MDMC, MDMCAT, “Explosion,” “Ease,” “Molly”] December 2019 Introduction: discriminate DOM from saline. 3,4-Methylenedioxymethcathinone (methylone) is a Because of the structural and pharmacological similarities designer drug of the phenethylamine class. Methylone is a between methylone and MDMA, the psychoactive effects, adverse synthetic cathinone with substantial chemical, structural, and health risks, and signs of intoxication resulting from methylone pharmacological similarities to 3,4-methylenedioxymeth- abuse are likely to be similar to those of MDMA. Several chat amphetamine (MDMA, ecstasy). Animal studies indicate that rooms discussed pleasant and positive effects of methylone when methylone has MDMA-like and (+)-amphetamine-like used for recreational purpose. behavioral effects. When combined with mephedrone, a controlled schedule I substance, the combination is called User Population: “bubbles.” Other names are given in the above title. Methylone, like other synthetic cathinones, is a recreational drug that emerged on the United States’ illicit drug market in 2009. It is perceived as being a ‘legal’ alternative to drugs of Licit Uses: Methylone is not approved for medical use in the United abuse like MDMA, methamphetamine, and cocaine. Evidence States. indicates that youths and young adults are the primary users of synthetic cathinone substances which include methylone. However, older adults also have been identified as users of these Chemistry: substances. O H O N CH3 Illicit Distribution: CH O 3 Law enforcement has encountered methylone in the United States as well as in several countries including the Netherlands, Methylone United Kingdom, Japan, and Sweden. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Pharmacology and Toxicology of Amphetamine and Related Designer Drugs
Pharmacology and Toxicology of Amphetamine and Related Designer Drugs U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol Drug Abuse and Mental Health Administration Pharmacology and Toxicology of Amphetamine and Related Designer Drugs Editors: Khursheed Asghar, Ph.D. Division of Preclinical Research National Institute on Drug Abuse Errol De Souza, Ph.D. Addiction Research Center National Institute on Drug Abuse NIDA Research Monograph 94 1989 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 Pharmacology and Toxicology of Amphetamine and Related Designer Drugs ACKNOWLEDGMENT This monograph is based upon papers and discussion from a technical review on pharmacology and toxicology of amphetamine and related designer drugs that took place on August 2 through 4, 1988, in Bethesda, MD. The review meeting was sponsored by the Biomedical Branch, Division of Preclinical Research, and the Addiction Research Center, National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other matieral in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. -

Ring-Substituted Amphetamine Interactions with Neurotransmitter Receptor Binding Sites in Human Cortex
208 NeuroscienceLetters, 95 (1988) 208-212 Elsevier Scientific Publishers Ireland Ltd. NSL O5736 Ring-substituted amphetamine interactions with neurotransmitter receptor binding sites in human cortex Pamela A. Pierce and Stephen J. Peroutka Deparmentsof Neurologyand Pharmacology, Stanford University Medical Center, StanJbrd,CA 94305 (U.S.A.) (Received 31 May 1988; Revised version received 11 August 1988; Accepted 12 August 1988) Key words.' Ring-substituted amphetamine; (_+)-3,4-Methylenedioxyamphetamine; ( +_)-3,4-Methylene- dioxyethamphetamine; (_+)-3,4-Methylenedioxymethamphetamine; Ecstasy; 4-Bromo-2,5- dimethoxyphenylisopropylamine binding site; Human cortical receptor The binding affinities of 3 ring-substituted amphetamine compounds were determined at 9 neurotrans- mitter binding sites in human cortex. (_+)-3,4-Methylenedioxyamphetamine (MDAk (_+)-3,4-methylene- dioxyethamphetamine (MDE), and (_+)-3,4-methylenedioxymethamphetamine (MDMA or 'Ecstasy') all display highest affinity (approximately 1 /tM) for the recently identified 'DOB binding site' labeled by ['TBr]R(-)4-bromo-2,5-dimethoxyphenylisopropylamine ([77Br]R(-)DOB). MDA displays moderate affinity (4-5/iM) for the 5-hydroxytryptaminetA (5-HTr^), 5-HT_D,and =,-adrenergic sites in human cor- tex. MDE and MDMA display lower affinity or are inactive at all other sites tested in the present study. These observations are discussed in relation to the novel psychoactive effects of the ring-substituted amphetamines. A series of ring-substituted amphetamine derivatives exist which are structurally related to both amphetamines and hallucinogens. However, drugs such as (+)-3,4- methylenedioxyamphetamine (MDA), (_+)-3,4-methylenedioxyethamphetamine (MDE), and (+)-3,4-methylenedioxymethamphetamine (MDMA or 'Ecstasy') ap- pear to produce unique psychoactive effects which are distinct from the effects of both amphetamines and hallucinogens [13, 15]. -

124.204 Schedule I — Substances Included. 1. Schedule I Shall Consist
1 , §124.204 124.204 Schedule I — substances included. 1. Schedule I shall consist of the drugs and other substances, by whatever official name, common or usual name, chemical name, or brand name designated, listed in this section. 2. Opiates. Unless specifically excepted or unless listed in another schedule, any of the following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, whenever the existence of such isomers, esters, ethers, and salts is possible within the specific chemical designation: a. Acetylmethadol. b. Allylprodine. c. Alphacetylmethadol (except levo-alphacetylmethadol also known as levo-alpha- acetylmethadol, levomethadyl acetate, or LAAM). d. Alphameprodine. e. Alphamethadol. f. Alpha-Methylfentanyl (N-(1-(alpha-methyl-beta-phenyl) ethyl-4-piperidyl) propionanilide; 1-(1-methyl-2-phenylethyl)-4-(N-propanilido)piperidine). g. Benzethidine. h. Betacetylmethadol. i. Betameprodine. j. Betamethadol. k. Betaprodine. l. Clonitazene. m. Dextromoramide. n. Difenoxin. o. Diampromide. p. Diethylthiambutene. q. Dimenoxadol. r. Dimepheptanol. s. Dimethylthiambutene. t. Dioxaphetyl butyrate. u. Dipipanone. v. Ethylmethylthiambutene. w. Etonitazene. x. Etoxeridine. y. Furethidine. z. Hydroxypethidine. aa. Ketobemidone. ab. Levomoramide. ac. Levophenacylmorphan. ad. Morpheridine. ae. Noracymethadol. af. Norlevorphanol. ag. Normethadone. ah. Norpipanone. ai. Phenadoxone. aj. Phenampromide. ak. Phenomorphan. al. Phenoperidine. am. Piritramide. an. Proheptazine. ao. Properidine. ap. Propiram. aq. Racemoramide. ar. Tilidine. as. Trimeperidine. at. Beta-hydroxy-3-methylfentanyl (other name: N-[1-(2-hydroxy-2-phenethyl)- 3-methyl-4-piperidinyl]-N-phenylpropanamide). Thu May 19 07:35:43 2016 Iowa Code 2016, Section 124.204 (25, 1) §124.204, 2 au. Acetyl-alpha-methylfentanyl (N-[1-(1-methyl-2-phenethyl)-4-piperidinyl]-N- phenylacetamide). av.