Page 1 a COMPREHENSIVE PLAN to IMPROVE the HEALTH OF
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oklahoma State Senate
OKLAHOMA STATE SENATE 2005 LEGISLATIVE SUMMARY AND FY’06 BUDGET REVIEW Oklahoma State Senate 2005 LEGISLATIVE SUMMARY AND FY 2006 BUDGET REVIEW July 1, 2005 We are pleased to present the 2005 Legislative Summary and FY 2006 Budget Review. Included within this document are summaries of all substantive bills and resolutions enacted in the 2005 session and information on appropriation measures and the state budget adopted by the Legislature for FY 2006. The summaries contained herein have been prepared by the following Senate Committee Staff personnel: • Kim Brown, Legislative Analyst, Senate Education Committee • Sara Kyte, Legislative Analyst/Attorney, Senate Retirement and Group Health Committee • Selden Jones, Staff Attorney • Tracy Kersey, Legislative Analyst/Attorney, Senate Judiciary Committee • Judy King, Staff Attorney • Mary Jo Mitts, Legislative Analyst, Senate Energy, Environment and Communications and Sunset Committees • Nancy Pellow, Legislative Analyst, Senate Appropriations Subcommittee on Public Safety and Judiciary • Cheryl Purvis, Staff Attorney • Joanie Raff, Legislative Analyst, Senate Finance Committee • Lexa Shafer, Legislative Analyst, Senate Business and Labor Committee • Tom Stanfill, Legislative Analyst, Senate Aerospace and Technology and Public Safety and Homeland Security Committees • Melanie Stucky, Staff Attorney • Robert Thompson, General Counsel • Jeri Trope, Legislative Analyst, Senate General Government, Agricultural and Rural Development, Tourism and Wildlife and Veterans, Military Affairs and Public -

Ally, the Okla- Homa Story, (University of Oklahoma Press 1978), and Oklahoma: a History of Five Centuries (University of Oklahoma Press 1989)
Oklahoma History 750 The following information was excerpted from the work of Arrell Morgan Gibson, specifically, The Okla- homa Story, (University of Oklahoma Press 1978), and Oklahoma: A History of Five Centuries (University of Oklahoma Press 1989). Oklahoma: A History of the Sooner State (University of Oklahoma Press 1964) by Edwin C. McReynolds was also used, along with Muriel Wright’s A Guide to the Indian Tribes of Oklahoma (University of Oklahoma Press 1951), and Don G. Wyckoff’s Oklahoma Archeology: A 1981 Perspective (Uni- versity of Oklahoma, Archeological Survey 1981). • Additional information was provided by Jenk Jones Jr., Tulsa • David Hampton, Tulsa • Office of Archives and Records, Oklahoma Department of Librar- ies • Oklahoma Historical Society. Guide to Oklahoma Museums by David C. Hunt (University of Oklahoma Press, 1981) was used as a reference. 751 A Brief History of Oklahoma The Prehistoric Age Substantial evidence exists to demonstrate the first people were in Oklahoma approximately 11,000 years ago and more than 550 generations of Native Americans have lived here. More than 10,000 prehistoric sites are recorded for the state, and they are estimated to represent about 10 percent of the actual number, according to archaeologist Don G. Wyckoff. Some of these sites pertain to the lives of Oklahoma’s original settlers—the Wichita and Caddo, and perhaps such relative latecomers as the Kiowa Apache, Osage, Kiowa, and Comanche. All of these sites comprise an invaluable resource for learning about Oklahoma’s remarkable and diverse The Clovis people lived Native American heritage. in Oklahoma at the Given the distribution and ages of studies sites, Okla- homa was widely inhabited during prehistory. -

Oklahoma Legislature
L 1400.5 W628 2005-2006 c.3 Who's Who 50th Oklahoma Legislature * * * * + + Oklahoma Department of Libraries WHO IS WHO 2005 and 2006 Legislative Sessions 50th Oklahoma Legislature February 2006 TABLE OF CONTENTS Oklahoma Elected Officials 1 Governor. 2 Lieutenant Governor 4 Cabinet Members 5 About the Oklahoma Legislature 6 Legislative Service Bureau 7 Senate Senate Leadership 7 President Pro Tempore 8 Senators by District 8 Senate Members 9 Senate Committees 29 Senate Contact Reference List 31 House Speaker of the House 32 House Leadership 33 State Representatives by District 34 House Members 35 House Contact Reference List 71 House Committees 74 This publication printed and issued by the Oklahoma Department of Libraries as authorized by 65 O.S. 1991, section 3- 110. Seventy-five (75) copies have been prepared at a cost of $364.09. Twenty-five (25) copies have been deposited with the Publications Clearinghouse of the Oklahoma Department of Libraries. 2/2006 Oklahoma Elected Officials Governor Brad Henry Insurance Commissioner State Capitol, Room 212 Kim Holland* Oklahoma City 73105 2401 NW 23rd, Suite 28 405/521-2342 FAX 405/521-3353 Oklahoma City 73107 Tulsa: State Office Building PO Box 53408 73152-3408 440 S. Houston, Suite 304, Tulsa 74127 405/521-2828 FAX 405/521-6652 918/581-2801 FAX 918/581-2835 800/522-0071 www.gov.ok.gov www.oid.state.ok. us Lieutenant Governor Commissioner of Labor Mary Fallin Brenda Reneau State Capitol, Room 211 4001 Lincoln Blvd. Oklahoma City 73105 Oklahoma City 73105 405/521-2161 FAX 405/525-2702 405/528-1500 FAX 405/528-5751 www. -
Blowing Off Steam Or Setting Wildfires?
University of Tulsa College of Law TU Law Digital Commons Articles, Chapters in Books and Other Contributions to Scholarly Works 2009 The Oklahoma Taxpayer and Citizen Protection Act: Blowing Off tS eam or Setting Wildfires? Elizabeth McCormick [email protected] Follow this and additional works at: http://digitalcommons.law.utulsa.edu/fac_pub Part of the Law Commons Recommended Citation 23 Geo. Immigr. L. J. 293 (2009). This Article is brought to you for free and open access by TU Law Digital Commons. It has been accepted for inclusion in Articles, Chapters in Books and Other Contributions to Scholarly Works by an authorized administrator of TU Law Digital Commons. For more information, please contact [email protected]. THE OKLAHOMA TAXPAYER AND CITIZEN PROTECTION ACT: BLOWING OFF STEAM OR SETTING WILDFIRES? ELIZABETH MCCORMICK* ABSTRACT This article considers Oklahoma's recent experiment in immigration regulation and examines how it is that Oklahoma has found itself on the front lines of the illegal immigration debate. The article begins with a discussion of the rich history of immigration to and immigrants in Oklahoma. It then attempts to unpack the evolution of Oklahoma's illegal immigration crisis and understand the genesis and the impacts of the state's comprehensive but perhaps exaggerated response to the perceived crisis. Finally, using Oklaho- ma's experience as an example, the article argues that a "steam valve" model of immigration federalism is no longer an apt description of sub-federal immigration lawmaking. Rather than allowing states to blow off their anti-immigrant steam, this article argues that allowing individual states to enact immigration control measures locally provides a dangerous mechanism for national anti-immigrant groups to accomplish through a state-by-state lobbying effort what they have been unable to achieve at the national level. -
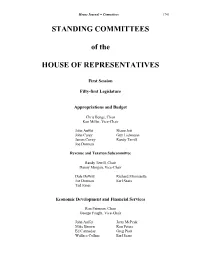
STANDING COMMITTEES of the HOUSE of REPRESENTATIVES
House Journal -- Committees 1741 STANDING COMMITTEES of the HOUSE OF REPRESENTATIVES First Session Fifty-first Legislature Appropriations and Budget Chris Benge, Chair Ken Miller, Vice-Chair John Auffet Shane Jett John Carey Guy Liebmann James Covey Randy Terrill Joe Dorman Revenue and Taxation Subcommittee Randy Terrill, Chair Danny Morgan, Vice-Chair Dale DeWitt Richard Morrissette Joe Dorman Earl Sears Tad Jones Economic Development and Financial Services Ron Peterson, Chair George Faught, Vice-Chair John Auffet Jerry McPeak Mike Brown Ron Peters Ed Cannaday Greg Piatt Wallace Collins Earl Sears 1742 House Journal -- Committees David Derby Mike Shelton Jeff Hickman Paul Wesselhoft Chuck Hoskin Susan Winchester Fred Jordan Banking Subcommittee Susan Winchester, Chair John Carey, Vice-Chair Chris Benge Steve Martin Neil Brannon Anastasia Pittman Rex Duncan R. C. Pruett Charles Key Purcy Walker Industry and Labor Subcommittee Paul Wesselhoft, Chair Ed Cannaday, Vice-Chair Wallace Collins Jerry Shoemake David Dank Weldon Watson Randy McDaniel Insurance and Retirement Subcommittee Jeff Hickman, Chair Charles Key, Vice-Chair Chris Benge Danny Morgan John Carey Mike Shelton Guy Liebmann Education Tad Jones, Chair Todd Thomsen, Vice-Chair Neil Brannon Ray McCarter Ann Coody Jeannie McDaniel Doug Cox Bill Nations David Dank Eric Proctor Lee Denney Phil Richardson Terry Hyman Jabar Shumate Terry Ingmire Daniel Sullivan Sally Kern House Journal -- Committees 1743 Arts and Culture Subcommittee Lee Denney, Chair Ben Sherrer, Vice-Chair Darrell Gilbert -

“Legal ... Illegal ... and Otherwise”
Drugs “Legal ... Illegal ... and Otherwise” 2005 Town Hall October 23-26 in Norman Introduction © 2005 The Oklahoma Academy 1-1 Created for the Oklahoma Academy by David Simpson 1-2 © 2005 The Oklahoma Academy Introduction OUR 2005 TOWN HALL Our 2005 Town Hall Michael Lapolla, University of Oklahoma; & Craig Knutson, e-conographic Consulting Services..... 1-8 Pre-Town Hall Thoughts Ross U. Robinson, Norman Economic Development Coalition ......................................................... 1-9 The Big Picture in Oklahoma Terry Cline, PhD, Oklahoma Secretary of Health ............................................................................ 1-10 Who’s Coming Into My ER? Mark Brandenburg, MD, Saint Francis Hospital, Tulsa.................................................................... 1-12 Who’s Coming Into My Office? Rosemary Priest, M.S., Tulsa .......................................................................................................... 1-15 LEGAL DRUGS: PRESCRIPTION MEDICINES THE BIG PICTURE Rethinking Prescription Drugs Malcolm Gladwell, The New Yorker. .................................................................................................. 2-2 Generation Rx? Pharmacy Today: American Pharmacists Association ....................................................................... 2-8 Productivity (Attributable to Biomedical Research) in the 21st Century Frank Lichtenberg, Professor, Columbia University School of Business.......................................... 2-9 THE INDUSTRY The Trouble With Cheap -

2007 Annual Report CONTENTS
Tulsa Community Foundation 7030 South Yale Avenue, Suite 600 Tulsa, Oklahoma 74136 Office: (918) 494-8823 • Fax: (918) 494-9826 www.tulsacf.org 2007 Annual Report CONTENTS Letter from the Executive Director ......................1 TCF History .......................................................2 Community Needs .............................................3 TCF’s Approach .................................................6 TCF’s Programs .................................................7 Community Impact ..........................................11 Why Give ........................................................12 How to Give ....................................................13 Ways To Give ..................................................15 Donor Profiles .................................................16 Donor Advised Funds .......................................17 Corporate Donor Advised Funds .......................18 Corporate Donor Profiles..................................19 Donor Designated Funds .................................21 Scholarship and Hardship Funds ......................22 Agency Profiles ...............................................23 Charitable Agency Funds ..................................26 Special Gift Profile ..........................................29 Supporting Organizations .................................30 Field of Interest Funds .....................................31 Financials .......................................................32 Board of Trustees ...........................................34 -

STANDING COMMITTEES of the HOUSE of REPRESENTATIVES
House Journal -- Committees 1957 STANDING COMMITTEES of the HOUSE OF REPRESENTATIVES First Session Fifty-second Legislature ADMINISTRATIVE RULES AND AGENCY OVERSIGHT John Wright, Chair George Faught, Vice-Chair John Auffet Steve Martin Mike Brown Jason Murphey Samson Buck Mike Reynolds Joe Dorman Earl Sears Dan Kirby AGRICULTURE AND RURAL DEVELOPMENT Don Armes, Chair John Enns, Vice-Chair Dennis Bailey Leslie Osborn Dale DeWitt R.C. Pruett Eddie Fields Brian Renegar Steve Kouplen Phil Richardson Ryan McMullen Mike Sanders Charles Ortega Harold Wright 1958 House Journal -- Committees APPROPRIATIONS AND BUDGET Ken Miller, Chair Scott Martin, Vice-Chair John Auffet Chuck Hoskin John Carey Mike Jackson Doug Cox Guy Liebmann Lee Denney Danny Morgan Dale DeWitt Ron Peters Joe Dorman Randy Terrill Larry Glenn Weldon Watson Jeff Hickman Education Subcommittee Lee Denney, Chair Earl Sears, Vice-Chair Ed Cannaday Sally Kern Ann Coody Jeannie McDaniel David Derby Bill Nations Eddie Fields Jabar Shumate Wes Hilliard Todd Thomsen Corey Holland Harold Wright General Government and Transportation Subcommittee Guy Liebmann, Chair Colby Schwartz, Vice-Chair Gary Banz Steve Martin Mike Brown Ryan McMullen Mike Jackson Eric Proctor Shane Jett Mike Reynolds Steve Kouplen T.W. Shannon Ken Luttrell Mike Thompson House Journal -- Committees 1959 Human Services Subcommittee Ron Peters, Chair Marian Cooksey, Vice-Chair Dennis Bailey Pam Peterson Wallace Collins Wade Rousselot David Dank Sue Tibbs Dennis Johnson Cory Williams Al McAffrey John Wright Charles Ortega -

State Senate Since Statehood First to Fourth Legislatures
823 State Senate Since Statehood First to Fourth Legislatures From 1907 to 1963, Senators were elected from their districts at-large. For Districts 13, 14, and 15, special nominating provisions existed. District 1st • 1907 2nd • 1909 3rd • 1911 4th • 1913 Pres. Pro Tempore Henry S. Johnston (D) J. C. Graham (D) J. Elmer Thomas (D) C. B. Kendrick (D) 1 Joe S. Morris (D) Joe S. Morris (D) J. H. Langston (R) Geo. L. Aycock (D) 2 A. E. Agee (D) E. L. Mitchell (D) E. L. Mitchell (D) E. L. Mitchell (D) 2 R. E. Echols (D) R. E. Echols (D) R. E. Echols (D) R. E. Echols (D) 3 A. G. Updegraff(R) A. G. Updegraff (R) Wm. A. Briggs (R) Wm. A. Briggs (R) 4 Frank Mathews (D) Henry J. Denton (D) Henry J. Denton (D) J. L. Carpenter (D) 5 Tom Moore (D) Tom Moore (D) Guy P. Horton (D) Guy P. Horton (D) 6 J. J. Williams (D) J. J. Williams (D) J. J. Williams (D) James L. Austin (D) 6 R. A. Billups (D) R. A. Billups (D) Geo. A. Coffey (D) 1 J. V. McClintic (D) 7 R. S. Curd (R) R. S. Curd (R) J. W. McCully (R) J. W. McCully (R) 8 P. J. Goulding (D) P. J. Goulding (D) P. J. Goulding (D) Eugene Watrous (R) 9 S. J. Soldani (D) S. J. Soldani (D) Wm. R. Dutton (R) Wm. R. Dutton (R) 9 Edmund Brazell (D) E. B. Chapman (R) E. B. Chapman (R) J. E. Curran (R) 10 H. -

Oklahoma Agencies, Boards, and Commissions
OklahomaA BC Agencies, Boards, and Commissions Elected Officers, Cabinet, Legislature, High Courts, and Institutions As of September 1, 2011 Acknowledgements The Oklahoma Department of Libraries, Office of Public Information,- ac knowledges the assistance of the Jan Eric Cartwright Memorial Law Library staff, the Oklahoma Publications Clearinghouse, and staff members of the agencies, boards, commissions, and other entities listed. Susan McVey, Director Connie G. Armstrong, Editor Oklahoma Department of Libraries Office of Public Information William R. Young, Administrator Office of Public Information For information about the ABC publication, please contact: Oklahoma Department of Libraries Office of Public Information 200 NE 18 Street, Oklahoma City, OK 73105–3298 405/522–3383 • 800/522–8116 • FAX 405/525–7804 www.odl.state.ok.us iii Contents Executive Branch 1 Governor Mary Fallin ......................................................................3 Office & Key Personnel ..................................................................................4 Oklahoma Elected Officials ..........................................................5 Office of the Lieutenant Governor ............................................................6 Office of the Attorney General ...................................................................7 Office of State Auditor and Inspector ......................................................8 Office of the State Treasurer ........................................................................9 Insurance