Clear Cell Acanthoma: a Review of Clinical and Histologic Variants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Morphological, Biological, and Biochemical Characteristics of a Benign Human Trichilemmoma Cell Line in Vivo and in Vitro'
[CANCER RESEARCH 41, 2468-2475. June 1981] 0008-5472/81 /0041 -OOOOS02.00 Morphological, Biological, and Biochemical Characteristics of a Benign Human Trichilemmoma Cell Line in Vivo and in Vitro' Tamotsu Kanzaki,2 Hikaru Eto, Akira Umezawa, Tohru Maeda, Hitoo Iwase, and Masatsugu Ito Departments of Dermatology [T. K., H. E., A. U.¡,Obstetrics-Gynecology ¡T.M.], Biochemistry [H. I.], and Plastic Surgery [M. I.], Kitasato University School of Medicine, Sagamihara 228. Japan ABSTRACT but she had left it alone for over 40 years. The tumor did not change in size during this period. In June 1978, the tumor bled A cell line of a benign human tumor, trichilemmoma, was for the first time after a traumatic brushing with a comb and established in vitro and has been maintained in culture for 1.5 then started to grow aggressively. The tumor was elastic, soft, years with more than 30 passages. Plating efficiency was less and 7 x 7 x 3 cm in size (Fig. 1) in February 1979. The surface than 0.1%, and population doubling time was 10 days. Satu ration density was 106 cells/sq cm at the time of a monolayer of the tumor was eroded with telangiectasia. It appeared yel lowish and somewhat translucent. The eroded surface was with 98% cell viability. Ultrastructurally, tissue-cultured trichi coated with pus. The left cervical lymph nodes were softly lemmoma cells showed desmosome-tonofilament complexes at swollen and freely movable. cell-to-cell junctions. The tissue-cultured cells synthesized abundant glycogen (50 to 100 ^g/106 cells) as observed in Tissue Culture. -

Genomic Landscape of a Metastatic Malignant Proliferating Tricholemmal Tumor and Its Response to PI3K Inhibition
www.nature.com/npjprecisiononcology CASE REPORT OPEN Genomic landscape of a metastatic malignant proliferating tricholemmal tumor and its response to PI3K inhibition Jean-Nicolas Gallant1, Andrew Sewell2,8, Karinna Almodovar1, Qingguo Wang3,9, Kimberly B. Dahlman1, Richard G. Abramson4, Meghan E. Kapp5, Brandee T. Brown2, Kelli L. Boyd5, Jill Gilbert1, Daniel N. Cohen5,10, Wendell G. Yarbrough2,9,6, Zhongming Zhao 3,7,11 and Christine M. Lovly1,7 Proliferating tricholemmal tumors (PTTs) are rare benign neoplasms that arise from the outer sheath of a hair follicle. Occasionally, these PTTs undergo malignant transformation to become malignant proliferating tricholemmal tumors (MPTTs). Little is known about the molecular alterations, malignant progression, and management of MPTTs. Here, we describe the case of a 58-year-old female that had a widely metastatic MPTT that harbored an activating PIK3CA mutation and was sensitive to the PI3K inhibitor, alpelisib (BYL719). We review the available literature on metastatic MPTT, detail the patient’s course, and present a whole genome analysis of this rare tumor. npj Precision Oncology (2019) 3:5 ; https://doi.org/10.1038/s41698-019-0077-2 INTRODUCTION posterior scalp cyst for cosmesis. This non-inflamed, non-draining, Proliferating tricholemmal tumors (PTTs) are benign neoplasms of painless, 1–2 cm cyst had been present for close to 10 years the external hair sheath.1 PTTs have the potential for malignant without change in size or fluctuance. The cyst was initially drained transformation, and, when characterized by cytologic atypia, by the PCP, but, when it recurred 6 months later, the PCP excised abnormal mitoses, and infiltrating margins, are termed malignant the cyst and sent the specimen for routine pathology. -

Pilar Sheath Acanthoma Presenting As a Nevus
Letter to Editor Pilar Sheath Acanthoma Presenting as a Nevus Sir, Pilar sheath acanthoma (PSA) is a rare benign follicular neoplasm, which was first described by Mehregan and Brownstein in 1978.[1] PSA usually presents as an asymptomatic, flesh colored papule with a central opening localized at the lower lip with exceptional presentations such as ear lobe, postauricular region, or cheek.[1‑3] A 42‑year‑old female referred with a solitary, slow‑growing nodular lesion at the upper lip region for 6 months. Physical exam revealed a 4 mm, pink‑brown colored nodule with a central opening [Figure 1]. Under clinical prediagnosis of melanocytic nevus, an excisional biopsy Figure 1: Physical examination of the nodule in the upper lip region was performed. In a microscopic examination, a cystic cavity that communicated with surface epidermis has been observed. The wall of the cystic cavity was composed of solid tumor islands extending in the deep dermis [Figure 2]. The cavity was lined with stratified squamous epithelium filled with keratin [Figure 3]. PSA is an uncommon, benign follicular tumor occurring in the faces of middle‑aged and elderly patients. These lesions can present at any location such as cheek, ear lobe on the head, and neck. In our case, a 42‑year‑old female was presented with a pink‑brown colored nodular lesion opening at the upper lip region. The differential diagnosis includes trichofolliculoma and dilated pore of Winer. Trichofolliculomas contain many seconder hair follicles Figure 2: A central cavity with keratin in the dermis which is continuous radiating from the wall of the primary follicle with outer with the surface epithelium (H and E, ×40) and inner root sheaths in a well‑formed stroma which are absent in PSA. -

A Rare Clinical Presentation of Desmoplastic Trichilemmoma
Revista5Vol89ingles_Layout 1 8/8/14 10:17 AM Página 796 796 CASE REPORT s A rare clinical presentation of Desmoplastic Trichilemmoma mimicking Invasive Carcinoma* Daniela Tiemi Sano1 Jeane Jeong Hoon Yang1 Antonio José Tebcherani1 Luiz Arthur de Paula Machado Bazzo1 DOI: http://dx.doi.org/10.1590/abd1806-4841.20143095 Abstract: Trichilemmoma is a benign neoplasm from the outer sheath of the pilosebaceous follicle. Desmoplastic trichilemmoma, a rare variant, is histologically characterized by a central area of desmoplasia that can clinically mimic an invasive carcinoma, requiring histopathological examination to define the diagnosis. Keywords: Hair diseases; Hair follicle; Skin neoplasms INTRODUCTION The trichilemmoma is a benign solid tumor ori- ma, without the presence of malignant processes, and ginating from external sheath cells of pilosebaceous associated with nevus sebaceous of Jadassohn in the follicles, and the desmoplastic trichilemmoma is a rare periphery of the lesion (Figures 3, 4, 5 and 6). Patient benign histological variant.1,2,3 Clinically, it may look is still under outpatient follow-up, with good clinical like other cutaneous lesions.2 Among the differential evolution and no relapse of lesion. diagnoses, we can cite basal-cell carcinoma, squamous cell carcinoma and viral lesions; the histopathological DISCUSSION examination is necessary for diagnostic confirmation. The trichilemmoma is a benign tumor origina- We report here a case of desmoplastic trichilemmoma ting from external root sheath cells of pilosebaceous in a -

The Tamilnadu Dr. M.G.R. Medical University Chennai, Tamil Nadu
CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS Dissertation Submitted in partial fulfillment of university regulations for M.D. DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROSY BRANCH XII – A THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY CHENNAI, TAMIL NADU SEPTEMBER 2006 CERTIFICATE This is to certify that this Dissertation entitled “CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS” is a bonafide work done by DR.G.BALAJI, Postgraduate student of Department of Dermatology, Leprosy and Institute of STD, Madras Medical College and Government General Hospital, Chennai – 3 for the award of Degree of M.D.( Dermatology, Venereology and Leprosy ) Branch XII – A during the academic year of 2003-2006. This work has not previously formed in the basis for the award of any degree or diploma. Prof. Dr. B. Parveen, MD., DD., Professor & Head, Dept. of Dermatology and Leprosy, Madras Medical College & Govt. General Hospital, Chennai – 3. Prof. Dr. Kalavathy Ponniraivan, MD., The Dean Madras Medical College & Govt. General Hospital, Chennai – 3. SPECIAL ACKNOWLEDGEMENT I sincerely thank Prof. Dr. Kalavathy Ponniraivan, MD., Dean, Madras Medical College & Govt. General Hospital, Chennai – 3, for granting me permission to use the resources of this institution for my study. ACKNOWLEDGEMENT I sincerely thank Prof. B.Parveen MD.,DD, Professor and Head of Department of Dermatology for her invaluable guidance and encouragement for the successful completion of this study. I express my heart felt gratitude to Dr.N.Gomathy MD.,DD, former Head of department of Dermatology who was instrumental in the initiation of this project, giving constant guidance throughout my work. -

Trichoblastoma Arising from the Nevus Sebaceus of Jadassohn
Open Access Case Report DOI: 10.7759/cureus.15325 Trichoblastoma Arising From the Nevus Sebaceus of Jadassohn Fatimazahra Chahboun 1 , Madiha Eljazouly 1 , Mounia Elomari 2 , Faycal Abbad 3 , Soumiya Chiheb 1 1. Dermatology Unit, Cheikh Khalifa International University Hospital, Mohammed VI University of Health Sciences, Casablanca, MAR 2. Plastic and Reconstructive Surgery, Cheikh Khalifa International University Hospital, Mohammed VI University of Health Sciences, Casablanca, MAR 3. Pathology, Cheikh Khalifa International University Hospital, Mohammed VI University of Health Sciences, Casablanca, MAR Corresponding author: Fatimazahra Chahboun, [email protected] Abstract Trichoblastoma is a rare benign skin adnexal tumour, belonging to the category of trichogenic tumours. The clinical and histological findings may often be confused with basal cell carcinoma, a malignant epidermal skin tumour. We report here a case of a 70-year-old man presented with a dome-shaped, dark-pigmented nodule within a yellowish hairless plaque on the scalp. The plaque had existed since childhood. However, the central pigmented nodule began appearing three months ago and enlarging gradually. The patient had no medical history. Furthermore the physical examination revealed a translucent, verrucous, and yellowish plaque, with central and pigmented nodule measuring 0.7 × 0.5 cm. Also basal cell carcinoma and trichoblastoma’s diagnosis were discussed. The patient was subsequently referred to the plastic surgery department, where he underwent a total excision. The histological examination was in favour of trichoblastoma arising from the nevus sebaceus. After 24 months of checking, no recurrence was observed. Trichoblastoma is a benign adnexal tumour. Its progression to malignant trichoblastoma (or trichoblastic carcinoma) is possible, but remains exceptional. -

What Are Basal and Squamous Cell Skin Cancers?
cancer.org | 1.800.227.2345 About Basal and Squamous Cell Skin Cancer Overview If you have been diagnosed with basal or squamous cell skin cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Are Basal and Squamous Cell Skin Cancers? Research and Statistics See the latest estimates for new cases of basal and squamous cell skin cancer and deaths in the US and what research is currently being done. ● Key Statistics for Basal and Squamous Cell Skin Cancers ● What’s New in Basal and Squamous Cell Skin Cancer Research? What Are Basal and Squamous Cell Skin Cancers? Basal and squamous cell skin cancers are the most common types of skin cancer. They start in the top layer of skin (the epidermis), and are often related to sun exposure. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer cells. To learn more about cancer and how it starts and spreads, see What Is Cancer?1 Where do skin cancers start? Most skin cancers start in the top layer of skin, called the epidermis. There are 3 main types of cells in this layer: ● Squamous cells: These are flat cells in the upper (outer) part of the epidermis, which are constantly shed as new ones form. When these cells grow out of control, they can develop into squamous cell skin cancer (also called squamous cell carcinoma). -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Hair Follicle Tumors
Hair Follicle Tumors 803-808-7387 www.gracepets.com These notes are provided to help you understand the diagnosis or possible diagnosis of cancer in your pet. For general information on cancer in pets ask for our handout “What is Cancer”. Your veterinarian may suggest certain tests to help confirm or eliminate diagnosis, and to help assess treatment options and likely outcomes. Because individual situations and responses vary, and because cancers often behave unpredictably, science can only give us a guide. However, information and understanding for tumors in animals is improving all the time. We understand that this can be a very worrying time. We apologize for the need to use some technical language. If you have any questions please do not hesitate to ask us. What is this tumor? This is one of many similar tumors that arise by disordered growth of the hair follicles. These tumors are almost all benign and can be permanently cured by total surgical removal. Some occur at multiple sites within the same animal. This family of tumors grade into each other. Precise nomenclature is usually irrelevant as almost all are benign. What do we know about the cause? The reason why a particular pet may develop this, or any cancer, is not straightforward. Cancer is often seemingly the culmination of a series of circumstances that come together for the unfortunate individual. Cross Section of Skin & Hair Follicle B-catenin is required for differentiation of skin cells into hair follicles. If there is over-production of this chemical in the body, hair follicle tumors develop. -

Expert-Level Diagnosis of Nonpigmented Skin Cancer by Combined Convolutional Neural Networks
Supplementary Online Content Tschandl P, Rosendahl C, Akay BN, et al. Expert-level diagnosis of nonpigmented skin cancer by combined convolutional neural networks. JAMA Dermatol. Published online November 28, 2018. doi:10.1001/jamadermatol.2018.4378 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set eAppendix. Neural Network Training eTable 1. Complete List of Diagnoses and Their Frequencies Within the Test-Set eTable 2. Education of Users According to Their Experience Group eTable 3. Percent of Correct Prediction of the Malignancy Status for Specific Diagnoses of a CNN Using Either Close-up or Dermatoscopic Images This supplementary material has been provided by the authors to give readers additional information about their work. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set A threshold cut at 0.2 (black) is found for a minimum of 51.3% specificity. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eAppendix. Neural Network Training We compared multiple architecture and training hyperparameter combinations in a grid-search fashion, and used only the single best performing network for dermoscopic and close-up images, based on validation accuracy, for further analyses. We trained four different CNN architectures (InceptionResNetV2, InceptionV3, Xception, ResNet50) and used model definitions and ImageNet pretrained weights as available in the Tensorflow (version 1.3.0)/ Keras (version 2.0.8) frameworks. -
A Case of Polypoid Clear Cell Acanthoma on the Nipple
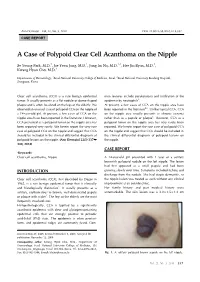
Ann Dermatol Vol. 22, No. 3, 2010 DOI: 10.5021/ad.2010.22.3.337 CASE REPORT A Case of Polypoid Clear Cell Acanthoma on the Nipple Se Young Park, M.D.1, Jae Yoon Jung, M.D.1, Jung Im Na, M.D.1,2, Hee Jin Byun, M.D.1, Kwang Hyun Cho, M.D.1 Departments of Dermatology, 1Seoul National University College of Medicine, Seoul, 2Seoul National University Bundang Hospital, Seongnam, Korea Clear cell acanthoma (CCA) is a rare benign epidermal mon features include parakeratosis and infiltration of the tumor. It usually presents as a flat nodule or dome-shaped epidermis by neutrophils3. plaque and is often localized on the legs of the elderly. We At present, a few cases of CCA on the nipple area have observed an unusual case of polypoid CCA on the nipple of been reported in the literature4-6. Unlike typical CCA, CCA a 14-year-old girl. At present, a few cases of CCA on the on the nipple area usually presents as chronic eczema nipple area have been reported in the literature. However, rather than as a papule or plaque6. However, CCA as a CCA presented as a polypoid tumor on the nipple area has polypoid tumor on the nipple area has very rarely been been reported very rarely. We herein report the very rare reported. We herein report the rare case of polypoid CCA case of polypoid CCA on the nipple and suggest that CCA on the nipple and suggest that CCA should be included in should be included in the clinical differential diagnosis of the clinical differential diagnosis of polypoid lesions on polypoid lesions on the nipple.