Proposed Integrated Control of Zoonotic Plasmodium Knowlesi in Southeast Asia Using Themes of One Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plasmodium Evasion of Mosquito Immunity and Global Malaria Transmission: the Lock-And-Key Theory
Plasmodium evasion of mosquito immunity and global malaria transmission: The lock-and-key theory Alvaro Molina-Cruz1,2, Gaspar E. Canepa1, Nitin Kamath, Noelle V. Pavlovic, Jianbing Mu, Urvashi N. Ramphul, Jose Luis Ramirez, and Carolina Barillas-Mury2 Laboratory of Malaria and Vector Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, MD 20852 Contributed by Carolina Barillas-Mury, October 15, 2015 (sent for review September 19, 2015; reviewed by Serap Aksoy and Daniel L. Hartl) Plasmodium falciparum malaria originated in Africa and became for the parasite to evade mosquito immunity. The implications global as humans migrated to other continents. During this jour- of P. falciparum selection by mosquitoes for global malaria ney, parasites encountered new mosquito species, some of them transmission are discussed. evolutionarily distant from African vectors. We have previously shown that the Pfs47 protein allows the parasite to evade the mos- Results quito immune system of Anopheles gambiae mosquitoes. Here, we Differences in Compatibility Between P. falciparum Isolates from investigated the role of Pfs47-mediated immune evasion in the Diverse Geographic Origin and Different Anopheline Species. The adaptation of P. falciparum to evolutionarily distant mosquito species. compatibility between P. falciparum isolates from different continents We found that P. falciparum isolates from Africa, Asia, or the Americas and mosquito vectors that are geographically and evolutionarily have low compatibility to malaria vectors from a different continent, distant was investigated by simultaneously infecting major malaria an effect that is mediated by the mosquito immune system. We iden- vectors from Africa (A. gambiae), Southeast Asia (Anopheles dirus), tified 42 different haplotypes of Pfs47 that have a strong geographic and the New World (A. -

RTS,S Malaria Vaccine First Malaria Vaccine Will Be Piloted in Areas of Three African Countries Through Routine Immunization Programs
CENTER FOR VACCINE INNOVATION AND ACCESS The RTS,S malaria vaccine First malaria vaccine will be piloted in areas of three African countries through routine immunization programs Summary the vaccine’s role in reducing childhood deaths and severe malaria, and its safety in the context of routine use. Data and Malaria kills more than 400,000 people a year worldwide and information from the MVIP will inform a WHO policy causes illness in tens of millions more, with most deaths recommendation on the broader use of the vaccine. RTS,S has occurring among young children living in sub-Saharan Africa. been approved for use in the pilot evaluation and Phase 4 Although existing interventions have helped to reduce malaria studies by the national regulatory authority in each of the three deaths significantly over the past 15 years, a vaccine could add participating countries. an important complementary tool for malaria control efforts. Financing for the MVIP has been mobilized through an RTS,S/AS01 (RTS,S) is the first malaria vaccine shown to unprecedented collaboration among three global health funding provide partial protection against malaria in young children. It bodies: Gavi, the Vaccine Alliance; the Global Fund to Fight will be the first malaria vaccine provided to young children AIDS, Tuberculosis and Malaria; and Unitaid. Additionally, through national immunization programs in three sub-Saharan WHO, PATH, and GSK are providing in-kind contributions, African countries—Ghana, Kenya, and Malawi. These countries which include GSK’s donation of the vaccine for use in the will introduce the vaccine in selected areas as part of a large- MVIP. -

Comparison of the Plasmodium Species Which Cause Human Malaria
Comparison of the Plasmodium Species Which Cause Human Malaria Plasmodium Stages found Appearance of Erythrocyte species in blood (RBC) Appearance of Parasite normal; multiple infection of RBC more delicate cytoplasm; 1-2 small chromatin Ring common than in other species dots; occasional appliqué (accollé) forms normal; rarely, Maurer’s clefts seldom seen in peripheral blood; compact Trophozoite (under certain staining conditions) cytoplasm; dark pigment seldom seen in peripheral blood; mature Schizont normal; rarely, Maurer’s clefts = 8-24 small merozoites; dark pigment, (under certain staining conditions) clumped in one mass P.falciparum crescent or sausage shape; chromatin in a Gametocyte distorted by parasite single mass (macrogametocyte) or diffuse (microgametocyte); dark pigment mass normal to 1-1/4 X,round; occasionally fine Ring Schüffner’s dots; multiple infection of RBC large cytoplasm with occasional not uncommon pseudopods; large chromatin dot enlarged 1-1/2–2 X;may be distorted; fine large ameboid cytoplasm; large chromatin; Trophozoite Schüffner’s dots fine, yellowish-brown pigment enlarged 1-1/2–2 X;may be distorted; fine large, may almost fill RBC; mature = 12-24 Schizont Schüffner’s dots merozoites; yellowish-brown, coalesced P.vivax pigment round to oval; compact; may almost fill enlarged 1-1/2–2 X;may be distorted; fine RBC; chromatin compact, eccentric Gametocyte Schüffner’s dots (macrogametocyte) or diffuse (micro- gametocyte); scattered brown pigment normal to 1-1/4 X,round to oval; occasionally Ring Schüffner’s dots; -

Research Toward Vaccines Against Malaria
© 1998 Nature Publishing Group http://www.nature.com/naturemedicine REVIEW Louis Miller (National Institute of Allergy and Infectious Diseases) and Stephen Hoffman (Naval Medical Research Institute) review progress toward developing malaria vaccines. They argue that multiple antigens from different stages may be needed to protect the diverse populations at risk, and that an optimal vaccine would Induce Immunity against all stages. Vaccines for African children, In whom the major mortality occurs, must induce immunity against ase,cual blood stages. Research toward vaccines against malaria Malaria is one of the major causes of the only stage of the life cycle that causes disease and death between the Tropic LOUIS H. MILLER1 disease. The stages before the asexual of Cancer and Tropic of Capricorn. & STEPHEN L. HOFFMAN2 blood stage are lumped together and Plasmodium falciparum has an especially called pre-erythrocytic. A small propor profound impact on infants and children in sub-Saharan Africa, tion of the asexual blood stages differentiate into sexual stages, where its effect on health is increasing as chloroquine resistance the gametocytes in red cells that infect mosquitoes; vaccines to spreads across the continent. We believe that vaccination the mosquito stages are called transmission-blocking vaccines. against P. falciparum is the intervention with the greatest poten The parasites' multistage life cycle and the fact that immune re tial to reduce malaria-associated severe morbidity and mortality sponses that recognize one stage often do not affect the next in areas with the most intense transmission and that it may do stage have made vaccine development for malaria more diffi so without necessarily preventing blood stage infection. -

A Review on the Progress of Sex-Separation Techniques For
Mashatola et al. Parasites & Vectors 2018, 11(Suppl 2):646 https://doi.org/10.1186/s13071-018-3219-4 REVIEW Open Access A review on the progress of sex-separation techniques for sterile insect technique applications against Anopheles arabiensis Thabo Mashatola1,2,3, Cyrille Ndo4,5,6, Lizette L. Koekemoer1,2, Leonard C. Dandalo1,2, Oliver R. Wood1,2, Lerato Malakoane1,2, Yacouba Poumachu3,4,7, Leanne N. Lobb1,2, Maria Kaiser1,2, Kostas Bourtzis3 and Givemore Munhenga1,2* Abstract The feasibility of the sterile insect technique (SIT) as a malaria vector control strategy against Anopheles arabiensis has been under investigation over the past decade. One of the critical steps required for the application of this technique to mosquito control is the availability of an efficient and effective sex-separation system. Sex-separation systems eliminate female mosquitoes from the production line prior to irradiation and field release of sterile males. This is necessary because female mosquitoes can transmit pathogens such as malaria and, therefore, their release must be prevented. Sex separation also increases the efficiency of an SIT programme. Various sex-separation strategies have been explored including the exploitation of developmental and behavioural differences between male and female mosquitoes, and genetic approaches. Most of these are however species-specific and are not indicated for the major African malaria vectors such as An. arabiensis. As there is currently no reliable sex-separation method for An. arabiensis, various strategies were explored in an attempt to develop a robust system that can be applied on a mass- rearing scale. The progress and challenges faced during the development of a sexing system for future pilot and/or large-scale SIT release programmes against An. -

Malaria History
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike License. Your use of this material constitutes acceptance of that license and the conditions of use of materials on this site. Copyright 2006, The Johns Hopkins University and David Sullivan. All rights reserved. Use of these materials permitted only in accordance with license rights granted. Materials provided “AS IS”; no representations or warranties provided. User assumes all responsibility for use, and all liability related thereto, and must independently review all materials for accuracy and efficacy. May contain materials owned by others. User is responsible for obtaining permissions for use from third parties as needed. Malariology Overview History, Lifecycle, Epidemiology, Pathology, and Control David Sullivan, MD Malaria History • 2700 BCE: The Nei Ching (Chinese Canon of Medicine) discussed malaria symptoms and the relationship between fevers and enlarged spleens. • 1550 BCE: The Ebers Papyrus mentions fevers, rigors, splenomegaly, and oil from Balantines tree as mosquito repellent. • 6th century BCE: Cuneiform tablets mention deadly malaria-like fevers affecting Mesopotamia. • Hippocrates from studies in Egypt was first to make connection between nearness of stagnant bodies of water and occurrence of fevers in local population. • Romans also associated marshes with fever and pioneered efforts to drain swamps. • Italian: “aria cattiva” = bad air; “mal aria” = bad air. • French: “paludisme” = rooted in swamp. Cure Before Etiology: Mid 17th Century - Three Theories • PC Garnham relates that following: An earthquake caused destruction in Loxa in which many cinchona trees collapsed and fell into small lake or pond and water became very bitter as to be almost undrinkable. Yet an Indian so thirsty with a violent fever quenched his thirst with this cinchona bark contaminated water and was better in a day or two. -

Meeting Report
Meeting Report EXPERT CONSULTATION ON PLASMODIUM KNOWLESI MALARIA TO GUIDE MALARIA ELIMINATION STRATEGIES 1–2 March 2017 Kota Kinabalu, Malaysia Expert Consultation on Plasmodium Knowlesi Malaria to Guide Malaria Elimination Strategies 1–2 March 2017 Kota Kinabalu, Malaysia WORLD HEALTH ORGANIZATION REGIONAL OFFICE FOR THE WESTERN PACIFIC RS/2017/GE/05/(MYS) English only MEETING REPORT EXPERT CONSULTATION ON PLASMODIUM KNOWLESI MALARIA TO GUIDE MALARIA ELIMINATION STRATEGIES Convened by: WORLD HEALTH ORGANIZATION REGIONAL OFFICE FOR THE WESTERN PACIFIC Kota Kinabalu, Malaysia 1–2 March 2017 Not for sale Printed and distributed by: World Health Organization Regional Office for the Western Pacific Manila, Philippines September 2017 NOTE The views expressed in this report are those of the participants of the Expert Consultation on Plasmodium knowlesi Malaria to Guide Malaria Elimination Strategies and do not necessarily reflect the policies of the World Health Organization. This report has been prepared by the World Health Organization Regional Office for the Western Pacific for governments of Member States in the Region and for those who participated in the Expert Consultation on Plasmodium knowlesi Malaria to Guide Malaria Elimination Strategies, which was held in Kota Kinabalu, Malaysia from 1 to 2 March 2017. CONTENTS ABBREVIATIONS SUMMARY 1. INTRODUCTION ............................................................................................................................................. 1 2. PROCEEDINGS ............................................................................................................................................... -

Renal Localization of Plasmodium Vivax and Zoonotic Monkey Parasite Plasmodium Knowlesi Derived Components in Malaria Associated Acute Kidney Injury
bioRxiv preprint doi: https://doi.org/10.1101/544726; this version posted May 3, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Renal Localization of Plasmodium vivax and Zoonotic Monkey Parasite Plasmodium knowlesi Derived Components in Malaria Associated Acute Kidney Injury Pragyan Acharya1#, Atreyi Pramanik1*, Charandeep Kaur1*, Kalpana Kumari2*, Rajendra Mandage1, Amit Kumar Dinda2, Jhuma Sankar3, Arvind Bagga3, Sanjay Kumar Agarwal4, Aditi Sinha3, Geetika Singh2 *These authors have contributed equally # Corresponding Author: [email protected] (Lab 3002, Department of Biochemistry, 3rd Floor, Teaching Block, AIIMS, Ansari Nagar, New Delhi – 110029) Author Affiliations: 1 Department of Biochemistry, All India Institute of Medical Sciences, New Delhi, India 2Department of Pathology, All India Institute of Medical Sciences, New Delhi, India 3Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India 4Department of Nephrology, All India Institute of Medical Sciences, New Delhi, India 1 bioRxiv preprint doi: https://doi.org/10.1101/544726; this version posted May 3, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. ABSTRACT Objectives Acute kidney injury (AKI) is a frequent clinical manifestation of severe malaria. Although the pathogenesis of P. falciparum severity is attributed to cytoadherence, the pathogenesis due to P. -

Sexual Development in Plasmodium Parasites: Knowing When It’S Time to Commit
REVIEWS VECTOR-BORNE DISEASES Sexual development in Plasmodium parasites: knowing when it’s time to commit Gabrielle A. Josling1 and Manuel Llinás1–4 Abstract | Malaria is a devastating infectious disease that is caused by blood-borne apicomplexan parasites of the genus Plasmodium. These pathogens have a complex lifecycle, which includes development in the anopheline mosquito vector and in the liver and red blood cells of mammalian hosts, a process which takes days to weeks, depending on the Plasmodium species. Productive transmission between the mammalian host and the mosquito requires transitioning between asexual and sexual forms of the parasite. Blood- stage parasites replicate cyclically and are mostly asexual, although a small fraction of these convert into male and female sexual forms (gametocytes) in each reproductive cycle. Despite many years of investigation, the molecular processes that elicit sexual differentiation have remained largely unknown. In this Review, we highlight several important recent discoveries that have identified epigenetic factors and specific transcriptional regulators of gametocyte commitment and development, providing crucial insights into this obligate cellular differentiation process. Trophozoite Malaria affects almost 200 million people worldwide and viewed under the microscope, it resembles a flat disc. 1 A highly metabolically active and causes 584,000 deaths annually ; thus, developing a After the ring stage, the parasite rounds up as it enters the asexual form of the malaria better understanding of the mechanisms that drive the trophozoite stage, in which it is far more metabolically parasite that forms during development of the transmissible form of the malaria active and expresses surface antigens for cytoadhesion. the intra‑erythrocytic developmental cycle following parasite is a matter of urgency. -

Indel-Informed Bayesian Analysis Suggests Cryptic Population
Infection, Genetics and Evolution 75 (2019) 103994 Contents lists available at ScienceDirect Infection, Genetics and Evolution journal homepage: www.elsevier.com/locate/meegid Research Paper Indel-informed Bayesian analysis suggests cryptic population structure between Plasmodium knowlesi of humans and long-tailed macaques (Macaca T fascicularis) in Malaysian Borneo ⁎ JustinJ.S. Wilcox ,1, Abigail Kerschner, Hope Hollocher Department of Biological Sciences, University of Notre Dame, Notre Dame, IN 46556-5688, USA ARTICLE INFO ABSTRACT Keywords: Plasmodium knowlesi is an important causative agent of malaria in humans of Southeast Asia. Macaques are Malaria natural hosts for this parasite, but little is conclusively known about its patterns of transmission within and Plasmodium knowlesi between these hosts. Here, we apply a comprehensive phylogenetic approach to test for patterns of cryptic Zoonosis population genetic structure between P. knowlesi isolated from humans and long-tailed macaques from the state Macaque of Sarawak in Malaysian Borneo. Our approach differs from previous investigations through our exhaustive use Host specificity of archival 18S Small Subunit rRNA (18S) gene sequences from Plasmodium and Hepatocystis species, our inclusion Phylogeny of insertion and deletion information during phylogenetic inference, and our application of Bayesian phyloge- netic inference to this problem. We report distinct clades of P. knowlesi that predominantly contained sequences from either human or macaque hosts for paralogous A-type and S-type 18S gene loci. We report significant partitioning of sequence distances between host species across both types of loci, and confirmed that sequences of the same locus type showed significantly biased assortment into different clades depending on their host species. -
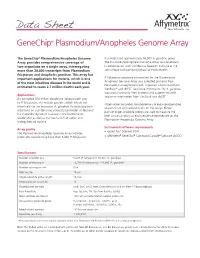
Genechip® Plasmodium/Anopheles Genome Array
Data Sheet GeneChip® Plasmodium/Anopheles Genome Array The GeneChip® Plasmodium/Anopheles Genome transcripts and approximately 16,900 A. gambiae genes. Array provides comprehensive coverage of The Plasmodium/Anopheles Genome Array was developed two organisms on a single array, interrogating in collaboration with the Malaria Research Institute at the more than 20,000 transcripts from Plasmodium Johns Hopkins Bloomberg School of Public Health. falciparum and Anopheles gambiae. This array has important applications for malaria, which is one P. falciparum sequence information for the Plasmodium/ of the most infectious diseases in the world and is Anopheles Genome Array was collected primarily from PlasmodB and augmented with sequence information from estimated to cause 2.7 million deaths each year. GenBank® and dbEST. Sequence information for A. gambiae was drawn primarily from Ensembl and augmented with Applications sequence information from GenBank and dbEST. An estimated 300 million people are infected each year by P. falciparum, the malaria parasite, which infects red Oligonucleotide probes complementary to each corresponding blood cells via the mosquito, A. gambiae. By including both sequence are synthesized in situ on the arrays. Eleven organisms on a single array, scientists can better understand pairs of oligonucleotide probes are used to measure the the molecular dynamics involved in the host/parasite level of transcription of each sequence represented on the relationship as well as the mechanism of action and Plasmodium/Anopheles Genome Array. biology behind malaria. Instrument/software requirements Array profile GeneChip® Scanner 3000 The Plasmodium/Anopheles Genome Array includes ® ® ® probe sets representing more than 5,400 P. falciparum Affymetrix GeneChip Command Console Software (AGCC) Specifications Number of probe sets 5,407 (P. -

Plasmodium Falciparum Full Life Cycle and Plasmodium Ovale Liver Stages in Humanized Mice
ARTICLE Received 12 Nov 2014 | Accepted 29 May 2015 | Published 24 Jul 2015 DOI: 10.1038/ncomms8690 OPEN Plasmodium falciparum full life cycle and Plasmodium ovale liver stages in humanized mice Vale´rie Soulard1,2,3, Henriette Bosson-Vanga1,2,3,4,*, Audrey Lorthiois1,2,3,*,w, Cle´mentine Roucher1,2,3, Jean- Franc¸ois Franetich1,2,3, Gigliola Zanghi1,2,3, Mallaury Bordessoulles1,2,3, Maurel Tefit1,2,3, Marc Thellier5, Serban Morosan6, Gilles Le Naour7,Fre´de´rique Capron7, Hiroshi Suemizu8, Georges Snounou1,2,3, Alicia Moreno-Sabater1,2,3,* & Dominique Mazier1,2,3,5,* Experimental studies of Plasmodium parasites that infect humans are restricted by their host specificity. Humanized mice offer a means to overcome this and further provide the opportunity to observe the parasites in vivo. Here we improve on previous protocols to achieve efficient double engraftment of TK-NOG mice by human primary hepatocytes and red blood cells. Thus, we obtain the complete hepatic development of P. falciparum, the transition to the erythrocytic stages, their subsequent multiplication, and the appearance of mature gametocytes over an extended period of observation. Furthermore, using sporozoites derived from two P. ovale-infected patients, we show that human hepatocytes engrafted in TK-NOG mice sustain maturation of the liver stages, and the presence of late-developing schizonts indicate the eventual activation of quiescent parasites. Thus, TK-NOG mice are highly suited for in vivo observations on the Plasmodium species of humans. 1 Sorbonne Universite´s, UPMC Univ Paris 06, CR7, Centre d’Immunologie et des Maladies Infectieuses (CIMI-Paris), 91 Bd de l’hoˆpital, F-75013 Paris, France.