Why “Not 20/20” After an Excellent Phacoemulsification Surgery?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Challenges in Ophthalmic Pathology: the Vitreoretinal Membrane Biopsy
Challenges in PAUL HISCOTT, DAVID WONG, IAN GRIERSON ophthalmic pathology: The vitreoretinal membrane biopsy Abstract detachment.s Sheets or strands crossing the vitreous are sometimes called transvitreous The introduction of vitreoretinal microsurgery membranes. Anteriorly, membranes can arise has produced a new type of biopsy; that of the in, or be continuous with, the vitreous base and vitreoretinal membrane. This review even extend as far as the posterior iris surface or investigates methods by which these scar-like pupil. tissues are handled in the laboratory and Biopsies of pathological tissue are usually explores the implications of the results of such undertaken to establish a diagnosis. evaluations. The study of vitreoretinal Vitreoretinal biopsies also may be for diagnostic membrane biopsies has provided much purposes as, for example, in the case of information concerning the pathobiology of intraocular lymphoma, but such conditions are the various conditions which may give rise to rare and tend not to produce membranes. the tissue as well as insights into how Conversely, in the conditions which do produce membranes themselves develop. Moreover, membranes the diagnosis is seldom in doubt. the application of new laboratory techniques Why, then, attempt laboratory studies of is expected to enhance our understanding of vitreoretinal membranes? Laboratory findings the formation of vitreoretinal membranes, and from the membranes may have a number of lead to further advances in their surgical and uses, for example providing 'feed-back' to the medical management. surgeon concerning surgical dissection planes Key words Age-related macular degeneration, (see below). However, the principal objective of Epiretinal membrane, Proliferative diabetic these investigations is to improve our retinopathy, Proliferative vitreoretinopathy, understanding of the pathogenesis of P Hiscott D. -

Evaluation of Phacoemulsification Cataract Surgery Outcomes After Penetrating Keratoplasty
Open Access Maced J Med Sci electronic publication ahead of print, published on December 20, 2019 as https://doi.org/10.3889/oamjms.2019.379 ID Design Press, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. https://doi.org/10.3889/oamjms.2019.379 eISSN: 1857-9655 Basic and Clinical Medical Researches in Vietnam Evaluation of Phacoemulsification Cataract Surgery Outcomes After Penetrating Keratoplasty Le Xuan Cung1, Do Thi Thuy Hang1, Nguyen Xuan Hiep1, Do Quyet2, Than Van Thai3, Vu Thi Nga4, Nguyen Duy Bac2, Dinh Ngan Nguyen2* 1Vietnam National Institute of Ophthalmology, Hanoi, Vietnam; 2Vietnam Military Medical University (VMMU), Hanoi, Vietnam; 3NTT Hi-tech Institute, Nguyen Tat Thanh University, Ho Chi Minh City, Vietnam; 4Institute for Research and Development, Duy Tan University, 03 Quang Trung, Danang, Vietnam Abstract Citation: Cung LX, Hang DTT, Hiep NX, Quyet D, Thai BACKGROUND: Cataract is one of the reasons which causes impaired visual acuity (VA) of the eyes after TV, Nga VT, Bac ND, Nguyen DN. Evaluation of penetrating keratoplasy (PK), which can be treated by cataract surgery after PK or triple procedure. Cataract Phacoemulsification Cataract Surgery Outcomes After Penetrating Keratoplasty. Open Access Maced J Med Sci. surgery after PK has advantages that parameters of the eyes such as axial length, anterior chamber depth (ACD) https://doi.org/10.3889/oamjms.2019.379 as well as corneal curvature are stabilized after removing all sutures postoperatively, and intraocular lens (IOL) Keywords: Complicated Cataract; Corneal graft; power can be calculated correctly. Therefore, postoperative VA will be improved significantly. In Vietnam, there Penetrating Keratoplasty; Phacoemulsification have not been any study about cataract surgery after PK, therefore we conduct this research. -

SHOULD YOU OPEN a DRY-EYE CLINIC? Experts Help You Weigh the Pros and Cons
RETINAL PHOTOS ON THE GO P. 16 • CHANGES TO MEDICARE ABN FORMS P. 20 ENSURING A HAPPY CATARACT PATIENT P. 22 • MANAGING GLAUCOMA IN KPRO PATIENTS P. 58 THE CURRENT STATE OF VITREORETINAL EDUCATION P. 64 • WILLS EYE RESIDENT CASE REPORT P. 70 September 2020 reviewofophthalmology.com SHOULD YOU OPEN A DRY-EYE CLINIC? Experts help you weigh the pros and cons. P. 28 ALSO INSIDE: • The Latest Treatments for Dry Eye P. 38 • Comprehensive Ophthalmologists and Anti-VEGF Injections P. 48 • How to Manage Ocular Herpes P. 54 SHE MAY NEED MORE THAN ARTIFICIAL TEARS TO DISRUPT INFLAMMATION IN DRY EYE DISEASE1,2 Her eyes deserve a change. Choose twice-daily Xiidra for lasting relief that can start as early as 2 weeks.3*† Not an actual patient. *In some patients with continued daily use. One drop in each eye, twice daily (approximately 12 hours apart).3 †XiidraisanLFA-1antagonistforthetreatmentofdryeyedisease.Pivotaltrialdata:ThesafetyandefficacyofXiidrawereassessedinfour Important Safety Information (cont) 12-week,randomized,multicenter,double-masked,vehicle-controlledstudies(N=2133).Patientsweredosedtwicedaily.Useofartificial • I n clinicaltrials,themostcommonadversereactionsreportedin5-25%ofpatientswereinstillationsite tearswasnotallowedduringthestudies.Thestudyendpointsincludedassessmentofsigns(basedonInferiorfluoresceinCornealStaining irritation,dysgeusiaandreducedvisualacuity.Otheradversereactionsreportedin1%to5%ofthepatients Score [ICSS] on a scale of 0 to 4) and symptoms (based on patient-reported Eye Dryness Score [EDS] on a visual analogue scale of 0 to 100).3 were blurred vision, conjunctival hyperemia, eye irritation, headache, increased lacrimation, eye discharge, A larger reduction in EDS favoring Xiidra was observed in all studies at day 42 and day 84. Xiidra reduced symptoms of eye dryness at eye discomfort, eye pruritus and sinusitis. 2 weeks (based on EDS) compared to vehicle in 2 out of 4 clinical trials. -

Exploring Topical Anti-Glaucoma Medication Effects on the Ocular Surface in the Context of the Current Understanding of Dry Eye
The Ocular Surface 16 (2018) 289e293 Contents lists available at ScienceDirect The Ocular Surface journal homepage: www.theocularsurface.com Original Research Exploring topical anti-glaucoma medication effects on the ocular surface in the context of the current understanding of dry eye Aaron B.C. Wong, Michael T.M. Wang, Kevin Liu, Zak J. Prime, Helen V. Danesh-Meyer, * Jennifer P. Craig Department of Ophthalmology, New Zealand National Eye Centre, The University of Auckland, New Zealand article info abstract Article history: Purpose: To assess tear film parameters, ocular surface characteristics, and dry eye symptomology in Received 11 November 2017 patients receiving topical anti-glaucoma medications. Received in revised form Methods: Thirty-three patients with a diagnosis of open angle glaucoma or ocular hypertension, 26 February 2018 receiving unilateral topical anti-glaucoma medication for at least 6 months, were recruited in a cross- Accepted 2 March 2018 sectional, investigator-masked, paired-eye comparison study. Tear film parameters, ocular surface characteristics, and dry eye symptomology of treated and fellow eyes were evaluated and compared. Keywords: Results: The mean ± SD age of the participants was 67 ± 12 years, and the mean ± SD treatment duration Glaucoma ± fi ¼ fi Prostaglandin analogue was 5.3 4.4 years. Treated eyes had poorer non-invasive tear lm breakup time (p 0.03), tear lm ¼ ¼ Tear film osmolarity (p 0.04), bulbar conjunctival hyperaemia (p 0.04), eyelid margin abnormality grade Ocular surface (p ¼ 0.01), tear meniscus height (p ¼ 0.03), and anaesthetised Schirmer value (p ¼ 0.04) than fellow eyes. Dry eye There were no significant differences in dry eye symptomology, meibomian gland assessments, and Meibomian gland ocular surface staining between treated and fellow eyes (all p > 0.05). -

06 35938Nys130220 52
Changes in macular perfusion after Phacoemulsification surgery Sabah Abd El Azeem Soud, Doaa El Said El Badrawy, Nesma Sayed Mohammed Department of Ophthalmology, Alzahraa University Hospital, AL-Azhar University, Cairo, Egypt [email protected] Abstract: Background: Optical coherence tomography angiography (OCT-A) is a non-invasive, non-dye-based imaging modality that is used worldwide in the daily practice of ophthalmology. OCTA enhances our understanding of retinal diseases and retinal vascular changes. Objective: To evaluate, by means of optical coherence tomography angiography (OCTA) the changes that may occur at the macular vessels after phacoemulsification surgery and if these changes can affect the post-operative visual acuity. Patients and Methods: It was a prospective study carried out at Al Zahraa University Hospital on 30 eyes of 21 Patients with senile cataract were included. Retina vessel density at the macular area was checked by OCT A at 1 week, 1 month, and 3 months after cataract surgery. Results: Thirty eyes (21 patients) were included in the final analysis. There was a significant increase in retinal vessel density at the macular area after the cataract surgery, repeated-measures which extended to the end of the follow-up period. At 3 months postoperatively, Appearance of hyper reflective retinal spots post operatively was also noted. Conclusions: Macular vessel density increased after phacoemulsification surgery. These changes seem not to affect visual acuity. Whether these changes will persist over a longer period of time, that still needs to be studied. [Sabah Abd El Azeem Soud, Doaa El Said El Badrawy, Nesma Sayed Mohammed. Changes in macular perfusion after Phacoemulsification surgery. -

Intraocular Pressure During Phacoemulsification
J CATARACT REFRACT SURG - VOL 32, FEBRUARY 2006 Intraocular pressure during phacoemulsification Christopher Khng, MD, Mark Packer, MD, I. Howard Fine, MD, Richard S. Hoffman, MD, Fernando B. Moreira, MD PURPOSE: To assess changes in intraocular pressure (IOP) during standard coaxial or bimanual micro- incision phacoemulsification. SETTING: Oregon Eye Center, Eugene, Oregon, USA. METHODS: Bimanual microincision phacoemulsification (microphaco) was performed in 3 cadaver eyes, and standard coaxial phacoemulsification was performed in 1 cadaver eye. A pressure transducer placed in the vitreous cavity recorded IOP at 100 readings per second. The phacoemulsification pro- cedure was broken down into 8 stages, and mean IOP was calculated across each stage. Intraocular pressure was measured during bimanual microphaco through 2 different incision sizes and with and without the Cruise Control (Staar Surgical) connected to the aspiration line. RESULTS: Intraocular pressure exceeded 60 mm Hg (retinal perfusion pressure) during both standard coaxial and bimanual microphaco procedures. The highest IOP occurred during hydrodissection, oph- thalmic viscosurgical device injection, and intraocular lens insertion. For the 8 stages of the phaco- emulsification procedure delineated in this study, IOP was lower for at least 1 of the bimanual microphaco eyes compared with the standard coaxial phaco eye in 4 of the stages (hydro steps, nu- clear disassembly, irritation/aspiration, anterior chamber reformation). CONCLUSION: There was no consistent difference in IOP between the bimanual microphaco eyes and the eye that had standard coaxial phacoemulsification. Bimanual microincision phacoemul- sification appears to be as safe as standard small incision phacoemulsification with regard to IOP. J Cataract Refract Surg 2006; 32:301–308 Q 2006 ASCRS and ESCRS Bimanual microincision phacoemulsification, defined as capable of insertion through these microincisions become cataract extraction through 2 incisions of less than 1.5 mm more widely available. -

Macular Hole Formation Following Choroidal Neovascularization
Yoshida et al., Int J Ophthalmol Clin Res 2015, 2:1 International Journal of ISSN: 2378-346X Ophthalmology and Clinical Research Case Report: Open Access Macular Hole Formation Following Choroidal Neovascularization Treatment in A High Myopic Eye with Epiretinal Membrane Yusaku Yoshida*, Manabu Yamamoto, Takeya Kohno and Kunihiko Shiraki Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, Japan *Corresponding author: Yusaku Yoshida, MD, Department of Ophthalmology and Visual Science, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan, Fax:+81-666-343- 873, E-mail: [email protected] macular hole development where post-treatment regression of CNV Abstract seemed to have played a major role in a high myopic eye with ERM. Purpose: To report on the development of macular hole after treatment of choroidal neovascularization (CNV) in a patient with Case high myopia and epiretinal membrane (ERM). A 60-year-old man was examined in the Department of Methods: Retrospective single case report. Ophthalmology of Osaka City University Hospital for reduced vision Patients: A 60-year-old man presented with reduced vision in his in his right eye in January 2009. On initial examination, decimal best- right eye. On the initial examination, the right eye was high myopic corrected visual acuity (BCVA) was 0.3 in the right eye and 1.5 in with decimal best-corrected visual acuity (BCVA) of 0.3. the left eye, while intraocular pressures were 13 and 14 mmHg in the right and left eye, respectively. His previous medical and family Results: A subretinal grayish-white lesion was seen at the macula with hemorrhage, and optical coherence tomography showed a histories included nothing of note. -
Epiretinal Membrane
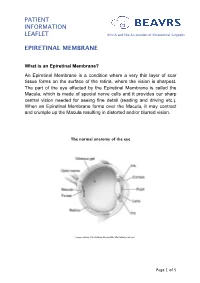
PATIENT INFORMATION LEAFLET British and Eire Association of Vitreoretinal Surgeons EPIRETINAL MEMBRANE What is an Epiretinal Membrane? An Epiretinal Membrane is a condition where a very thin layer of scar tissue forms on the surface of the retina, where the vision is sharpest. The part of the eye affected by the Epiretinal Membrane is called the Macula, which is made of special nerve cells and it provides our sharp central vision needed for seeing fine detail (reading and driving etc.). When an Epiretinal Membrane forms over the Macula, it may contract and crumple up the Macula resulting in distorted and/or blurred vision. The normal anatomy of the eye *Image courtesy of the National Eye Institute http://www.nei.nih.gov Page 1 of 5 PATIENT INFORMATION British and Eire Association of Vitreoretinal Surgeons LEAFLET EPIRETINAL MEMBRANE Why do I have an Epiretinal Membrane? In most cases the development of an Epiretinal Membrane appears to be related to normal aging changes inside the eye. In some cases it can be related to other conditions such as diabetes, blockage of blood vessel, inflammation or following retinal surgery. Epiretinal membranes are not related to Macular Degeneration. Epiretinal Membranes do not usually affect the other eye. They are quite common and affect up to 8% of people in later years. Cross-section of a healthy macula Cross-section of a macula with an epiretinal membrane Assessment for Epiretinal Membrane Your eye doctor is able to detect an Epiretinal Membrane during an eye examination following the use of eye drops that temporarily make your pupils large. -

Five-Year Outcomes of Trabeculectomy and Phacotrabeculectomy
Open Access Original Article DOI: 10.7759/cureus.12950 Five-Year Outcomes of Trabeculectomy and Phacotrabeculectomy Danny Lam 1 , David Z. Wechsler 1, 2 1. Ophthalmology, University of Sydney, Sydney, AUS 2. Ophthalmology, Macquarie University, Sydney, AUS Corresponding author: Danny Lam, [email protected] Abstract Purpose The purpose of this study is to examine five-year outcomes of trabeculectomy and compare the stand-alone procedure when combined with phacoemulsification. Patients and methods This study included 123 eyes of 109 patients, with 79 patients in the trabeculectomy group and 44 patients in the phacotrabeculectomy group. Non-randomized comparative cohort study with data collected retrospectively from an existing database compiled by a single surgeon operating in Sydney, Australia from 2007 to 2019. The primary outcome measure was intraocular pressure. Secondary outcome measures were a number of glaucoma medications, treatment success rates, best-corrected visual acuity, bleb morphology, post-operative complications, and re-operation rate. Results The mean intraocular pressure was 10.6 ± 2.7 mm Hg in the trabeculectomy group (pre-operative mean intraocular pressure of 28.0 ± 9.8) and 12.0 ± 3.0 mm Hg in the phacotrabeculectomy group (pre-operative mean intraocular pressure of 23.4 ± 7.9) after five years (P = 0.052). The number of glaucoma medications required was 0.3 ± 0.7 in the trabeculectomy group (pre-operative mean of 3.7 ± 1.1) and 1.3 ± 1.2 in the phacotrabeculectomy group (pre-operative mean of 3.1 ± 1.0, P < 0.001). Conclusions Intraocular pressure reduction post-operatively over five years was similar between trabeculectomy and phacotrabeculectomy as determined by mean intraocular pressure, and intraocular pressure reduction from baseline. -
Retinal Microvascular Alterations After Phacoemulsification in Patients With
Retinal microvascular alterations after phacoemulsication in patients with diabetes evaluated using optical coherence tomography angiography Le Feng Shanghai Tenth People's Hospital https://orcid.org/0000-0002-2148-7423 Guliqiwaer Azhati Shanghai Tenth People's Hospital Tingting Li Shanghai Tenth People's Hospital Fang Liu ( [email protected] ) https://orcid.org/0000-0003-2844-2225 Research article Keywords: retinal microvasculature, phacoemulsication, diabetes, OCT angiography Posted Date: August 26th, 2019 DOI: https://doi.org/10.21203/rs.2.13588/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/13 Abstract Purpose: To quantify changes in retinal microvasculature in diabetic patients after phacoemulsicatio by using optical coherence tomography angiography (OCTA). Methods: Macular thickness(MT), supercial capillary plexus (SCP), deep capillary plexuses (DCP) and foveal avascular zone (FAZ) measurements of the 3×3 mm macular images were obtained by OCTA at baseline, 1 day,1 week, 1 month, and 3 months after cataract surgery in diabetic and non- diabetic patients. Results: There was a signicant increase in MT at 1 month and 3 months after surgery in both groups (all P<0.05), but no signicant difference between the two groups (p= 0.217). At 3 months postoperatively, the SCP increase was signicantly higher compared with baseline in diabetic group (P<0.05). The MT and SCP was negatively correlated with logMAR best corrected visual acuity(BCVA), while the FAZ area and perimeter were positively correlated with logMAR BCVA in diabetic group. Conclusions: Cataract surgery can increase macular thickness in both diabetic and non- diabetic patients, and also increase the SCP in diabetic patients. -

IOC Mednick: Challenging Surgical Cases
Top 5 Pearls to Consider When Implanting Advanced Technology IOLs in Patients With Unusual Circumstances Zale D. Mednick, BA Guillermo Rocha, MD, FRCSC ’ Pearl #1: The Use of a Toric Multifocal Intraocular Lens (IOL) in the Management of Hyperopic Astigmatism Background The mainstay of treatment for those with hyperopic astigmatism who wish to bypass the need for glasses or contacts has traditionally been laser treatment. Both hyperopic laser in situ keratomileusis (LASIK) and photorefractive keratotomy (PRK) have been used to correct hyperopic astigmatism. Although LASIK can provide promising results for a portion of patients with hyperopic eyes, it becomes less effective when dealing with more exaggerated degrees of hyperopia. Refractive results are much more successful for low diopter (D) hyperopia, with a drop in efficacy starting at + 4.00 to + 5.00 D.1 Esquenazi and Mendoza2 reported that when LASIK is performed on eyes with >5.00 D of hyperopia, both the safety profile of the procedure and the refractive outcomes dramatically decline, coinciding with decreased corrected distance visual acuity (CDVA). Choi and Wilson3 echoed this notion, citing a 2-line drop in CDVA when LASIK was used to treat hyperopia of 5.00 to 8.75 D. This is in stark contrast to the results achieved by LASIK to improve myopia, where corrections are feasible for a far greater range of refractions. Part of the reason that hyperopia is less amenable to correction of higher diopter errors may owe to the fact that larger ablation zones are needed to achieve better refractive results.4 The optimal size of the ablation zone for hyperopic LASIK is >5.5 mm,1 and as such, more corneal alteration is required. -

Phacoemulsification Article by Penelope L
CONTINUING EDUCATION EXAMINATION PHACOEMULSIFICATION ARTICLE BY PENELOPE L. KUHN, CST In1967, an extraordinary innovation in cataract surgery Instrumentation was introduced by Dr Charles D. Kelman.' Distressed by cataract extraction procedures resulting in wound-related The Machine complications and long recuperative periods, Dr Kelman Several generations of phacoemulsification units have been developed a technique enabling surgeons to remove a cata- introduced since Kelman's early prototype in 1967. While ract from a small, 3.0-mm incision utilizing a sophisticated these models differ with respect to various features, instru- form of machine-assisted extracapsular cataract extraction mentation and mechanics are comparable between units. (ECCE). Kelman's development revolutionized cataract The following information is based upon the Phaco- surgery, which until then had been plagued by large inci- Emulsifier Aspirator (PEA) by Alcon Laboratories. sions and traumatic techniques. To describe his new proce- The PEA is an extremely complex piece of equipment, dure, Kelman coined the term phacoemulsijication. yet its operation is relatively simple. It has three basic This paper provides the surgical technologist with an functions: irrigation, aspiration, and ultrasonic vibration. overview of phacoemulsification mechanics, instrumenta- Later PEA models include vitrectomy capabilities. These tion, and operative procedure. functions are selected by compression of a footswitch. In addition, manual control switches are placed on the PEA Kelman Phacoemulsification unit's front console and consist of varying combinations of The term phacoemulsification implies emulsification of the the following: a main power switch, a footswitch position crystalline lens. In actuality, the lens is not liquified but fragmented into pieces small enough to be aspirated.