Journal Vol 5 No. 2 Issue 9
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dormant Account 10 Years and Above As on Ashadh 2076
Everest Bank Limited Head Office, Lazimpat 14th Aug 2019 DORMANT ACCOUNT 10 YEARS AND ABOVE AS ON ASHADH 2076 SN A/C NAME CURRENCY 1 BIRENDRA & PUNAMAYA EUR 2 ROBERT PRAETZEL EUR 3 NABARAJ KOIRALA EUR 4 SHREE NAV KANTIPUR BAHUUD NPR 5 INTERCONTINENTAL KTM HOTE NPR 6 KANHIYALAL & RAJESH OSWAL NPR 7 LAXMI HARDWARE NPR 8 NAVA KSHITIZ ENTERPRISES NPR 9 SWADESHI VASTRA BIKRI BHA NPR 10 UNNAT INDUSTRIES LTD. NPR 11 RAJ PHOTO STUDIO NPR 12 RND ENTERPRISES NPR 13 LUMBINI RESORT AND HILL D NPR 14 ARUNODAY POLYPACK IND. NPR 15 UNNAT INDUSTRIES PVT.LTD. NPR 16 KRISHNA MODERN DAL UDYOG NPR 17 TIRUPATI DISTRIB. CONCERN NPR 18 LAXMI GALLA KATTA KHARID NPR 19 URGN HARDWARE CONCERN. NPR 20 AASHMA COOPERATIVE FINANC NPR 21 VERITY PRINTERS(P)LT NPR 22 PUZA TRADERS NPR 23 NEPAL MATCH MANUFACTURER NPR 24 G.B TEXTILE MILLS PVT. LT NPR 25 VISION 9PRODUCT. (P) L.-R NPR 26 PHOOLPATI ENTERPRISES NPR 27 ROSHI SAVING & CREDIT CO. NPR 28 SHRESTHA TRD.GROUP P.LTD. NPR 29 P.D.CONSULT (PARTNERS FOR NPR 30 N.Y.S.M.S RELIEF FUND NPR 31 ASHOK WIRE PVT. LTD NPR 32 PAWAN KRISHNA HARDWARE ST NPR 33 OCEAN COMPUTER PVT. LTD. NPR 34 CHHIGU MULTIPURPOSE CO-OP NPR 35 GAJENDRA TRADERS NPR 36 SURENDRA KARKI NPR 37 GATE WAY INT'L TRADERS NPR 38 VYAHUT COMMERCIAL TRADERS NPR 39 SAPTA KOSHI SAV.&CR. CO.L NPR 40 MHAIPI HOSIERY NPR 41 STYLE FOOTWEARS P LTD NPR 42 MINA IMPEX NPR 43 CUSTOM CLEARANCE SERVICE NPR 44 HOTEL LA DYNASY PVT. -

Mofa Tellist
Ministry of Foreign Affairs Phone: 4200182-185 Fax: 4200061, 4200160 , 4211522 OFFICE OF THE MINISTER FOR FOREIGN AFFAIRS Designation Name Telephone (O) Ext. Minister for Foreign Hon'ble Mr. Pradeep Kumar 4200196- 97 Affairs Gyawali Under Secretary Mr. Tej Bahadur Chhetri 4200196- 97 413 Section Officer Mr. Kul Bahadur Magar 240 Personal Secretary (Under Mr. Janga Bahadur Nepali 424 Secretary) Personal Press Expert Mr. Sudhan Gnawali 426 Personal Secretary Mr. Khem Raj Gyawali 236 (Section Officer) Nayab Subba Mr. Chuman Singh KC 414 IT Assistant Mrs. Juna Aryal 239 OFFICE OF THE FOREIGN SECRETARY ([email protected], Fax Foreign Secretary Mr. Shanker Das Bairagi 4200192-93 Section Officer Ms. Aastha Subba 268 Nayab Subba, PA Mr. Kapil Mani Ghimire 255 Office Assistant Mr. Khadga Bahadur Rana 255 OFFICE OF THE SPOKESPERSON ([email protected]) Spokesperson Mr. Bharat Raj Poudyal 4200176 231 Assistant Spokesperson Mr. Suresh Adhikari 407 GENERAL ADMINISTRATION DIVISION ([email protected]) Joint Secretary Mr. Kali Prasad Pokhrel 4200154 247 Nayab Subba Mr. Deepak Niraula 256 Administration Section ([email protected], Fax no.: 4200480) Under Secretary Mr. Gyan Bahadur Magar 220 Under Secretary Ms. Rojina Tamrakar 204 Under Secretary (Law) Ms. Arati Shrestha 434 Section Officer Mr. Binod Mukhiya 4200186 254 Section Officer Mr. Til Bahadur Sunar 4200186 252 Section Officer Mr. Bhupendra Prasad Ghimire 4200186 251 Nayab Subba Mr. Gyanhari Gyawali 254 Nayab Subba Mr. Dipendra Prasad Sah 251 Nayab Subba Mr. Gajendra Rai 252 IT Officer Mr. Bikram Shrestha 253 IT Assistant Ms. Riya Joshi 253 IT Assistant Ms. Prena Adhikari 251 Office Assistant Mr. -

AMBITION ACADEMY BANESHWOR, KATHMANDU CONGRATULATIONS !!! the Following Candidates Are Passed the Entrance Examination
AMBITION ACADEMY BANESHWOR, KATHMANDU CONGRATULATIONS !!! The following candidates are passed the entrance examination. The selected candidates are informed to visit the admission section for the further interview on 2076-03-22,Sunday, 6:30 am onwards. S.N. F.N. NAME OF THE STUDENTS STREAM RESULT 1 1836 AAKRITI PARAJULI MGMT PASS 2 1863 AARADHYA LAMSAL SCIENCE PASS 3 1846 AARATI KARNA SCIENCE PASS 4 1867 AARATI SEDHAIN SCIENCE PASS 5 1775 AARSHI KOIRALA SCIENCE PASS 6 608 AASHMA GAUTAM SCIENCE PASS 7 1638 AASHU KUSHWAR MGMT PASS 8 1888 AAYUSH NIROULA PASS 9 1637 AAYUSHMA POKHAREL MGMT PASS 10 1834 ABHISHEK GAUTAM SCIENCE PASS 11 1661 ABHISHEK THAPA MGMT PASS 12 1837 AJAY BAKHUNCHHE HUMANITIES PASS 13 1617 ALAAN SHRESTHA MGMT PASS 14 1695 ALBIN KATTEL SCIENCE PASS 15 1886 ALFAISAL MIKRNI MGMT PASS 16 1650 ALISHA KHADKA SCIENCE PASS 17 AMAN ADHIKARI MGMT PASS 18 609 AMAN KHADKA SCIENCE PASS 19 1725 AMIR BHANDARI MGMT PASS 20 1639 AMISHA THAPA MAGAR MGMT PASS 21 666 AMIT SHAH SCIENCE PASS 22 1664 AMRIT PATEL MGMT PASS 23 1683 AMRITA SHRESTHA SCIENCE PASS 24 688 ANIKET KUMAR THAKUR MGMT PASS 25 1670 ANIL GAUTAM SCIENCE PASS 26 673 ANIMESH ACHARYA SCIENCE PASS 27 1659 ANISH REGMI MGMT PASS 28 1665 ANISHA GHIMIRE PASS 29 1686 ANISHA POUDEL MGMT PASS 30 1839 ANITA JABEGU LIMBU MGMT PASS 31 1684 ANITA KHADKA SCIENCE PASS 32 616 ANJALI BHUJEL MGMT PASS 33 1624 ANJU BARME SCIENCE PASS S.N. F.N. NAME OF THE STUDENTS STREAM RESULT 34 1805 ANKIT KARKI SCIENCE PASS 35 1807 ANMOL SHRESTHA SCIENCE PASS 36 1885 ANOJ NIROULA MGMT PASS 37 675 ANSHU NEUPANE -
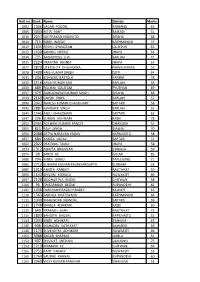
Roll No. Rank Name District Marks 1002 1306 SAGAR POUDEL
Roll no. Rank Name District Marks 1002 1306 SAGAR POUDEL MORANG 65 1006 3004 NITIN PANT BAITADI 51 1010 2047 JAY PRAKASH MAHATO SIRAHA 58 1011 715 BIBEK WAGLE KATHMANDU 71 1012 1435 RESHU SYANGTAN LALITPUR 63 1015 1430 SANJOG NEPALI JHAPA 63 1016 735 AASHUTOSH JHA SARLAHI 71 1025 2224 PRASNNA BASNET JHAPA 57 1027 2870 UTKRISHTA DHUNGANA NAWALPARASI 52 1028 1409 ANIL KUMAR SINGH DOTI 64 1031 204 BISHWAS BASTOLA PARBAT 78 1032 2116 ARUN KUMAR SAH SARLAHI 58 1033 889 ROCHAK GAUTAM PYUTHAN 69 1037 979 GURUCHARAN KUMAR SINGH SIRAHA 68 1039 2169 SAKSHI PRIYA SARLAHI 57 1040 2042 NARESH KUMAR CHAUDHARY SAPTARI 58 1041 2887 ABHISHEK SINGH SARLAHI 52 1043 1545 ANJU CHAUDHARI SAPTARI 62 1047 236 SUMAN ADHIKARI KASKI 78 1052 2465 ROSHANI KUMARI PANDIT DHANUSA 55 1055 815 RAVI SINGH SIRAHA 70 1056 2088 SATYA NARAYAN YADAV KAPILVASTU 58 1057 684 KABITA YADAV SAPTARI 71 1062 2022 PRATIMA TAMLI JHAPA 58 1073 1912 ASMITA BHANDARI SYANGJA 59 1075 20 SAROJ GC GULMI 85 1080 704 MISEK LIMBU TAPLEJUNG 71 1081 2712 SUBHAM KUMAR RAUNIYARGUPTA SUNSARI 53 1085 1919 ANKITA PANDEY RAUTAHAT 59 1090 1142 SHIVANI KOIRALA NUWAKOT 66 1097 2129 SIDDHARTHA REGMI CHITWAN 58 1100 96 CHUDAMADI REGMI RUPANDEHI 82 1102 1438 DARSHAN PRASAD PANDEY KALIKOT 63 1110 1363 SARDILA KHATIWADA KATHMANDU 64 1111 1949 MAHENDRA MANDAL SAPTARI 59 1115 1748 BIMALA ADHIKARI KASKI 60 1125 640 PRAKASH SHAH RAUTAHAT 72 1131 2892 SANGITA BHUSAL KAPILVASTU 52 1134 1093 BIBEK ADHIKARI SYANGJA 67 1140 908 MAHADEV KATHAYAT BAJHANG 69 1146 1175 SUVEKSHYA ADHIKARI NUWAKOT 66 1151 3088 SAGAR SHARMA JUMLA 51 1152 407 SHIVAJEE SHEDAIN LAMJUNG 75 1153 1219 MAMATA KC CHITWAN 66 1155 2755 AMIT PANDEY NUWAKOT 53 1160 1764 SAURAV KHANAL RUPANDEHI 60 1165 2960 VICKY KUMAR PANJIYAR DHANUSA 52 Roll no. -

Gaurishankar 2066 67
Gaurishankar List of UnPaid Divident Warrants Fiscal Year :67/68 S.NO. Holder No. Holder'S Name KITTA Net Amt W.No 1 81 JAGANNATH BHATTARAI 10 14.00 000081 2 82 YOGESH CHANDRA MISHRA 10 14.00 000082 3 83 NARESH PARIYAR 10 14.00 000083 4 84 VANDANA KUMARI MISHRA 10 14.00 000084 5 85 BIMALA NEPALI 10 14.00 000085 6 86 DIVAS NEPAL 10 14.00 000086 7 87 UTSAV NEPAL 10 14.00 000087 8 88 NIRMALA BASTOLA NEPAL 10 14.00 000088 9 89 BHARAT PD. NEPAL 10 14.00 000089 10 90 TILAK BDR. BHATTARAI 10 14.00 000090 11 91 GANGA BHATTARAI 10 14.00 000091 12 92 ROZINA KARKI 10 14.00 000092 13 97 LAXMAN PD. POKHREL 10 14.00 000097 14 98 KAMALA KUMARI KHANAL POKHREL 10 14.00 000098 15 99 ALINA POKHREL 10 14.00 000099 16 100 ABHISEK POKHREL 10 14.00 000100 17 101 YOG NRN. SAH 10 14.00 000101 18 102 PRABHA KUMARI MAHATO 10 14.00 000102 19 103 AMAN BIKRAM SHAH 10 14.00 000103 20 104 AYUSH BIKRAM SHAH 10 14.00 000104 21 105 SHILA KUMARI MAHATO 10 14.00 000105 22 137 SHARMILA KHADKA 10 14.00 000127 23 150 RAMESH KRISHNA MAHARJAN 10 14.00 000135 24 185 DHUNDIRAM KHANAL 10 14.00 000157 25 197 TULSI RAM KHANAL 10 14.00 000169 26 198 BHAGHABATA KHANAL 10 14.00 000170 27 199 MAHESH KHANAL 10 14.00 000171 28 200 SHEKHAR KHANAL 10 14.00 000172 29 207 NAWARAJ PURI 10 14.00 000179 30 208 UMESH PURI 10 14.00 000180 31 228 RAMESH LAGE 10 14.00 000198 32 229 TULSI PD NEPAL 10 14.00 000199 33 236 BIRAJ GAUTAM 10 14.00 000206 34 238 KANCHHI DAHAL 10 14.00 000208 35 239 RAM PD DAHAL 10 14.00 000209 36 262 SANJAY KUMAR PANDEY 10 14.00 000220 37 263 SAURAV PANDEY 10 14.00 000221 -

Theatre for Social Change in Kathmandu, Nepal
School of Oriental and African Studies University of London REHEARSING FOR LIFE: THEATRE FOR SOCIAL CHANGE IN KATHMANDU, NEPAL Monica Mottin Doctor in Philosophy Social Anthropology 2009-10 ProQuest Number: 10673177 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 10673177 Published by ProQuest LLC(2017). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 I declare that the work presented in this thesis is my own. Monica Mottin 2 Acknowledgements Infinite gratitude goes to all the artists and activists whose collaboration made this research possible. This research could be carried out thanks to a grant from the CRF (University of London). I wish to thank my supervisors Prof. David Mosse and Prof. Michael Hutt for their inspirational ideas and support during the challenges of the fieldwork and writing up, and my family, for their patience and love. 3 Abstract The objective is this research is to examine the production and performance of theatrical activities aiming at bringing about social change in both development and political intervention. My investigation began with Aarohan Theatre Group, a Kathmandu-based professional company and subsequently extended to Maoist cultural troupes. -

America Nepal Society, Washington, DC, MEMBERSHIP LIST -2011/2012
America Nepal Society, Washington, DC, MEMBERSHIP LIST ‐2011/2012 S.N Head of the House Family Member Phone NumberCITY state Last Name First Name 1 Thapa Bijay Archana Ghimire 703.855.2579South Riding VA 2 Dawadi Mukti Ambika dawadi 703.915.9957Falls Church VA 3 Shrestha Manoj MD 4 Pudasaini Thakur 703.565.4697Manassas VA 5 Dahal Ojaswi 240.478.4102Gaithersburg MD 6 Tiwari Loknath 301.332.1427 MD 7 Gurung Dinesh 410.288.8123 MD 8 Bhandary Chetnath 310.332.1427 MD 9 Tiwari Tilak MD 10 Neupane Goma Falls Church VA 11 Neupane Sushil Kalpana 301.755.3328Falls Church VA 12 Shrestha Pramesh VA 13 Shah Vijaya 703.931.1721Falls Church VA 14 Gaudel Laxmi 703.280.8782Chantilly VA 15 Baral Keshab Gayatir 571.216.8951Chantilly VA 16 Shrestha Rajesh 703.996.6476Woodbridge VA 17 kc Subu 703.851.2970South Riding VA 18 Dahal Kedar Chantilly VA 19 Malakar Ram Silver spring MD 20 Sharma Hari 703.307.7151 MD 21 Sangraula Prem 703.356.3874Falls Church VA 22 Kharel Narayan MD 23 Maharjan Ganga MD 24 Ranjit Ratna MD 25 Thapa Rabina Narayan Thapa 443.839.6555Baltimore MD 26 Niraula Rita MD 27 Maharjan Bijay MD 28 Shrestha Neeta MD 29 Karki Rup Ashburn VA 30 Sharma Bidya VA 31 Thapa Sundar MD 32 Sharma Dhaneswar 240.421.3625Gaithesburg MD 33 Khanal Krishna Chantilly VA 34 Sangraula Khem 703.759.9181Chantilly VA 35 Sharma Anand Arlington VA 36 Tiwari Sudip Ranjana TiwariFalls Church VA 37 Koirala Shankar VA 38 Pandey Gyan 39 Bhandary Madusudan 40 Dhakal Lal krishna 41 Pokhrel Kali Prasad Arlington VA 1 America Nepal Society, Washington, DC, MEMBERSHIP LIST ‐2011/2012 -
Divident List
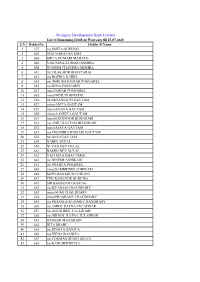
Shangrila Development Bank Limited List of Remaining Divident Warrants till 15-07-2020 S.N HolderNo Holder'S Name 1 577 ms.SMITA GURUNG 2 603 YOG NARAYAN SAH 3 604 SHILA KUMARI MAHATO 4 606 VANDANA KUMARI MISHRA 5 608 YOGESH CHANDRA MISHRA 6 612 mr.TILAK BDR BHATTARAI 7 613 ms.ROZINA KARKI 8 615 mr.DHRUBA KUMAR POKHAREL 9 616 ms.NIMA POKHAREL 10 617 minorNIRAB POKHAREL 11 618 minorMINU POKHAREL 12 626 mr.JAGANNATH GAUTAM 13 627 minorANITA GAUTAM 14 629 minorAVAYA GAUTAM 15 630 minorAANKITA GAUTAM 16 631 minorKOHINOOR BHANDARI 17 632 ms.ANJU GAUTAM BHANDARI 18 633 minorAJAYA GAUTAM 19 635 ms.CHANDRA KUMARI GAUTAM 20 636 mr.ANUJ GAUTAM 21 639 NABIN ARYAL 22 640 NUTAN DEV DULAL 23 641 BASHU DEV DULAL 24 642 YACHANA BHATTARAI 25 643 mr.DINESH ADHIKARI 26 644 ms.PRABHA POKHREL 27 645 minorSAMBRIDHI ADHIKARI 28 646 KESH BAHADUR GURUNG 29 647 TEK BAHADUR GURUNG 30 648 SIR BAHADUR GURUNG 31 652 mr.SIYARAM CHAUDHARY 32 653 minorSUMI CHAUDHARY 33 654 minorPRASHANT CHAUDHARY 34 655 ms.PRAMILA KUMARI CHAUDHARY 35 656 mr.AMRIT RATNA TULADHAR 36 657 ms.ANUSHREE TULADHAR 37 658 mr.NIRMAL RATNA TULADHAR 38 663 RAMESH MAHARJAN 39 664 RITA SHAHI 40 665 mr.BINAYA BANIYA 41 666 ms.JEENA BAANIYA 42 667 mr.YOGMAN SINGH DEUJA 43 668 ms.KANCHHI DEUJA 44 670 mr.KRISHNA BDR. BASNET 45 671 ms.ANJALI KHADKA 46 678 mr.MANOJ KUMAR SHAH 47 682 mr.MANOJ KUMAR MANDAL GANGAI 48 689 LAXMI GURUNG 49 690 mr.PADAM RAJ SIGDEL 50 691 ms.JYOTI KHADGI 51 692 RAMHARI BOHARA 52 693 NIRMALA SANGROULA BOHARA 53 694 SAMPADA BOHARA 54 695 mr.LAXMAN PAUDEL 55 696 minorSAMBRIDDHI MAHARJAN 56 698 mr.BUDDHA RATNA MAHARJAN 57 703 GAJENDRA RAJ GHIMIRE 58 713 MAHENDRA PD. -

Dividend Not Claimed
Shangrila Development Bank Limited List of UnIssued Divident Warrants Fiscal Year : 67/68 - 68/69 - 69/70 - 70/71 S.N Holder'S Name 1 YOGESH CHANDRA MISHRA 2 NABIN ARYAL 3 NUTAN DEV DULAL 4 BASHU DEV DULAL 5 YACHANA BHATTARAI 6 RAMESH MAHARJAN 7 RITA SHAHI 8 GAJENDRA RAJ GHIMIRE 9 JASHWINA NEUPANE 10 UDHAB POKHREL 11 SANGEET K.C. 12 SANGAM K.C. 13 PARBATI K.C 14 BEENA K.C. 15 HUM BDR. K.C. 16 GAJA LAXMI TAMRAKAR 17 MOHAN RATNA TAMRAKAR 18 KALPANA SHRESTHA 19 SUBASH KUMAR SHRESTHA 20 BISHNU MAYA SHRESTHA 21 UJWAL BDR TIWARI 22 JOSHNA TIWARI 23 TIKA PD DHUNGEL 24 PROGRESS SHRESTHA 25 GITA ARYAL 26 THAKUR PD ARYAL 27 RAJENDRA ADHIKARI 28 UJJWAL SHRESTHA 29 SALIK RAM KALATHOKI 30 SHAMA TULADHAR 31 NATASHA TULADHAR 32 LAXMI SHRESTHA PANDEY 33 ANUKRITIKA PRASAI 34 GITANJALI SHRESTHA 35 NIKETIKA PRASAI 36 KANCHAN JUNGHA PRASAI 37 PRIYA PRASAI 38 INDIRA PRASAI 39 NARENDRA RAJ PRASAI 40 SUBIGYA POKHAREL 41 SADIKAHYA POKHAREL 42 SHARADA KUMARI KHATIWADA 43 BISHNU PD POKHAREL 44 GITA GNAWALI 45 LEKHNATH POKHREL 46 DURGA MAYA DAHAL 47 SAROJ DAHAL 48 AAFRIN GURUNG 49 SRISHTI NEUPANE 50 RAJKUMAR BASTOLA 51 KRISHNA BDR. KUNWAR 52 PUSPA RAJ PATHAK 53 RATNA SUNDER SHAKYA 54 PRATIBHA SHAKYA 55 SAUNDARYA SHAKYA 56 PURNIMA SHAKYA 57 SAGAR SINGH SAUD 58 BASANTA RATNA TULADHAR 59 LAYATA TULADHAR 60 ARJUN PANTA 61 DURGA POKHAREL PANTA 62 NAGENDRA PD. NIROULA 63 HARIBOL PRADHAN 64 MENUKA PAUDYAL 65 NISHA PAUDYAL 66 ISAWORI PAUDYAL 67 LAXMI PAUDYAL 68 KRISHNA BDR. SHRESTHA 69 SHARAD BABU SHRESTHA 70 RANI SHRESTHA SUVEKSHA 71 SHASHI RANJAN KALWAR 72 SHREEYA KHADGI 73 SABITA TULADHAR 74 SHEKHAR KHADGI 75 DINESH RAJ KOIRALA 76 PUNDEV PD. -

Laxmi Bank Ltd. Shortlisted Candidate for Written Exam (Trainee Assistant) Kathmandu Center S.No
Laxmi Bank Ltd. Shortlisted Candidate for Written Exam (Trainee Assistant) Kathmandu Center S.No. Symbol No. Name Email Id 1 TA00001 Premita Poudel [email protected] 2 TA00002 Dhan Bahadur Jagari [email protected] 3 TA00003 Ganesh Gaire [email protected] 4 TA00004 Sabitri Badu [email protected] 5 TA00005 Saraswoti Saud [email protected] 6 TA00006 Pramila Pradhan [email protected] 7 TA00007 Munu Rai [email protected] 8 TA00008 Deepa Lamichhane [email protected] 9 TA00009 Tribhuwan Gami [email protected] 10 TA00010 Usha Basnet [email protected] 11 TA00011 Sujan kc [email protected] 12 TA00012 Alisha Shrestha [email protected] 13 TA00013 Babita Aryal [email protected] 14 TA00014 Anjila Shrestha [email protected] 15 TA00015 Rishi Prasad Lamichhane [email protected] 16 TA00016 Ayesha Ghimire [email protected] 17 TA00017 Sujata Karki [email protected] 18 TA00018 Ashmita Dumre [email protected] 19 TA00019 Indira Pokhrel [email protected] 20 TA00020 Kamala Pokhrel [email protected] 21 TA00021 Ganesh Bahadur Khatri [email protected] 22 TA00022 Bibek K.C. [email protected] 23 TA00023 Subodh Ghimire [email protected] 24 TA00024 NIRU TIWARI [email protected] 25 TA00025 Samajhana Dhukuchhu [email protected] 26 TA00026 Bivek Nepal [email protected] 27 TA00027 Kabita Koju [email protected] 28 TA00028 Mohammad Manjur [email protected] 29 TA00029 Sujita Maharjan [email protected] 30 TA00030 Manda -

NATIONALISM and REGIONAL RELATIONS in DEMOCRATIC TRANSITIONS: COMPARING NEPAL and BHUTAN a Thesis Submitted in Partial Fulfillme
NATIONALISM AND REGIONAL RELATIONS IN DEMOCRATIC TRANSITIONS: COMPARING NEPAL AND BHUTAN A thesis submitted in partial fulfillment of the requirements for the degree of Master of Arts By DEKI PELDON Bachelor of Arts, Asian University for Women, 2014 2018 Wright State University WRIGHT STATE UNIVERSITY GRADUATE SCHOOL [May 4, 2018] I HEREBY RECOMMEND THAT THE THESIS PREPARED UNDER MY SUPERVISION BY DEKI PELDON ENTITLED NATIONALISM AND REGIONAL RELATIONS IN DEMOCRATIC TRANSITIONS: COMPARING NEPAL AND BHUTAN BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS. Laura M. Luehrmann, Ph.D. Thesis Director Laura M. Luehrmann, Ph.D. Director, Master of Arts Program in International and Comparative Politics Committee on Final Examination: Laura M. Luehrmann, Ph.D. School of Public and International Affairs Pramod Kantha, Ph.D. School of Public and International Affairs Judson Murray, Ph.D. Department of Religion, Philosophy and Classics Barry Milligan, Ph.D. Interim Dean of the Graduate School ABSTRACT Peldon, Deki. M.A., International and Comparative Politics Graduate Program, Wright State University, 2018. How Nationalism and Regional Influence Affected the Political Transitions of Bhutan and Nepal Democracy is facing crisis as its values including political rights and civil liberties are declining around the world. If democracy is to prevail, the reasons for the decline need to be addressed. To this end, the research question is: how nationalism and regional influences affect the political transitions of Bhutan and Nepal. The research question is answered by analyzing leadership stability, ethnicity and the caste system, as well as the roles of regional giants India and China in Bhutan’s and Nepal’s political transitions. -
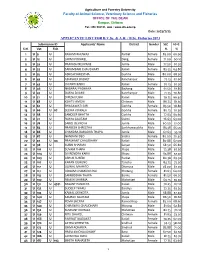
Applicants List for B.V.Sc. & A.H. And
Agriculture and Forestry University Faculty of Animal Science, Veterinary Science and Fisheries OFFICE OF THE DEAN Rampur, Chitwan Tel.: 056 592131, web : www.afu.edu.np Date: 2073/7/23 APPLICANTS' LIST FOR B.V.Sc. & A.H. / B.Sc. Fisheries 2073 Submission ID Applicants' Name District Gender SLC 10+2 S.N. Vet. Fish. % % 1 U 9 U RASHMI BHUWAJI Parbat Female 83.00 66.90 2 U 12 U LAXMI POKHREL Dang Female 71.00 60.10 3 U 32 U PRAKASH NEUPANE Jumla Male 77.50 67.20 4 U 33 U SAKAMBARI CHAUDHARY Kailali Female 83.25 64.80 5 U 35 U ASHISH SHRESTHA Gorkha Male 80.00 68.30 6 U 42 U ABHISHEK BASNET Kanchanpur Male 77.13 67.60 7 U 43 U JAYANTI KARKI Kailali Female 70.13 67.30 8 U 46 U NABARAJ PADHAYA Bajhang Male 61.50 61.80 9 U 47 U BIJAYA DHAMI Kanchanpur Male 71.75 70.80 10 U 51 U DIPESH JOSHI Kailali Male 79.75 66.40 11 U 58 U KSHITIJ AMGAI Chitwan Male 86.75 81.30 12 U 62 U BHAGAWATI GIRI Gorkha Female 85.50 78.80 13 U 66 U 67 SEEMA KOIRALA Gorkha Female 80.13 70.30 14 U 68 U SANDEEP BHATTA Gorkha Male 77.63 69.60 15 U 72 U BIJAYA GAUTAM Gulmi Male 76.63 63.00 16 U 78 U SAROJ DEVKOTA Jumla Male 60.50 51.00 17 U 85 U PRABESH SHRESTHA Sankhuwasabha Male 83.38 65.00 18 U 86 U CHANDRA BAHADUR THAPA Jumla Male 67.63 55.10 19 U 87 U NANDANI DEO Siraha Female 80.00 70.40 20 U 92 U 94 PRASHANT CHAUDHARY Kailali Male 80.88 67.00 21 U 98 U SUBIN SHARMA Salyan Male 68.50 66.80 22 U 101 U SUVAM THAPA Jhapa Male 75.38 67.30 23 U 104 U DHIRENDRA KARKI Mugu Male 63.88 57.30 24 U 109 U ASHOK SUBEDI Parbat Male 80.38 69.30 25 U 110 U KARAN GURUNG Tanahu Male