Single-Incision Laparoscopic Surgery in Liver Resection For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Is Pylorus Resecting Pancreaticoduodenectomy a Better Surgical Alternative Than Pylorus Preserving Pancreaticoduodenectomy Regarding Delayed Gastric Emptying?
Editorial Page 1 of 3 Is pylorus resecting pancreaticoduodenectomy a better surgical alternative than pylorus preserving pancreaticoduodenectomy regarding delayed gastric emptying? Shengliang He, Jin He Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA Correspondence to: Jin He, MD, PhD, FACS. Department of Surgery, Johns Hopkins Hospital, 600 N. Wolfe Street, Blalock 665, Baltimore, MD 21287, USA. Email: [email protected]. Provenance: This is an invited Editorial commissioned by Section Editor Dr. Ang Li (Department of General Surgery, Xuanwu Hospital Capital Medical University, Beijing 100053, China). Comment on: Hackert T, Probst P, Knebel P, et al. Pylorus Resection Does Not Reduce Delayed Gastric Emptying After Partial Pancreatoduodenectomy: A Blinded Randomized Controlled Trial (PROPP Study, DRKS00004191). Ann Surg 2018;267:1021-7. Received: 28 February 2018; Accepted: 19 March 2018; Published: 19 July 2018. doi: 10.21037/dmr.2018.07.04 View this article at: http://dx.doi.org/10.21037/dmr.2018.07.04 Pylorus preserving pancreaticoduodenectomy (PPPD) incidences (5). has been popularized as the surgical approach for patients As the currently largest, randomized controlled trial, with periampullary lesions by Traverso and Longmire PROPP study included 188 patients with statistical since 1978 (1). It was first hypothesized to reduce the superiority hypothesis (pylorus resection is associated occurrence of dumping, diarrhea, bile reflux gastritis and with less DGE than pylorus preservation). In the control improve overall nutritional status compared with classic group, duodenum was divided 2 cm distal to the pylorus. pancreaticoduodenectomy, also known as classic Whipple An antecolic end-to-side (ETS) duodenojejunostomy (CW). Based on the Cochrane database review in 2016, was performed 50 cm distal to the hepaticojejunostomy. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

The Differences Between ICD-9 and ICD-10
Preparing for the ICD-10 Code Set: Fact Sheet 2 October 1, 2015 Compliance Date Get the Facts to be Compliant Alert: The new ICD-10 compliance date is October 1, 2015. The Differences Between ICD-9 and ICD-10 This is the second fact sheet in a series and is focused on the differences between the ICD-9 and ICD-10 code sets. Collectively, the fact sheets will provide information, guidance, and checklists to assist you with understanding what you need to do to implement the ICD-10 code set. The ICD-10 code sets are not a simple update of the ICD-9 code set. The ICD-10 code sets have fundamental changes in structure and concepts that make them very different from ICD-9. Because of these differences, it is important to develop a preliminary understanding of the changes from ICD-9 to ICD-10. This basic understanding of the differences will then identify more detailed training that will be needed to appropriately use the ICD-10 code sets. In addition, seeing the differences between the code sets will raise awareness of the complexities of converting to the ICD-10 codes. Overall Comparisons of ICD-9 to ICD-10 Issues today with the ICD-9 diagnosis and procedure code sets are addressed in ICD-10. One concern today with ICD-9 is the lack of specificity of the information conveyed in the codes. For example, if a patient is seen for treatment of a burn on the right arm, the ICD-9 diagnosis code does not distinguish that the burn is on the right arm. -
Appendectomy: Simple Appendicitis
Appendectomy: Simple Appendicitis Your child has had an appendectomy (ap pen DECK toe mee). This is the surgical removal of the appendix. The appendix is a small, narrow sac at the beginning of the large intestine (Picture 1). The appendix has no known function. What to Expect After Surgery . Your child will awaken in the Post Anesthesia Care Unit (PACU) near the surgery area. He or she may be in the PACU for 1 to 2 hours. After your child wakes up in the PACU, he or she will return to a hospital room or be Esophagus transferred to the Surgery Unit. Discharge will be directly from the Surgery Unit. Liver Stomach . Your child will have 3 to 4 small incision Large sites (see Helping Hand HH-I-283, Intestines Laparoscopic Surgery (colon) ). Small . Your child will receive fluids and pain intestines medicine through an intravenous line (IV). Rectum When your child can take liquids by mouth, pain medicine will also be given by mouth. Appendix . Your child will need to cough and deep-breathe often to help keep the lungs clear. He or she may use a plastic device called an incentive Picture 1 The appendix inside the body. spirometer to help with this. Your child will need to get up and walk soon after surgery. Walking will help "wake up" the bowels; it will also help with breathing and blood flow. Your child will be able to go home on the same day of the surgery if he or she is: o able to drink clear liquids like water, clear soft drinks, broth, and fruit punch o taking pain medicine by mouth and his or her pain is controlled, and o able to walk. -
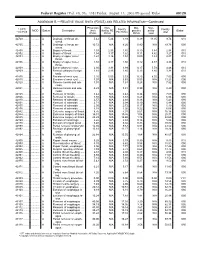
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

Incidental Drainage of a Periappendicular Abscess During Colonoscopy
UCTN – Unusual cases and technical notes E175 Incidental drainage of a periappendicular abscess during colonoscopy A 50-year-old man was referred to the of oral metronidazole and ciprofloxacin. A P. Figueiredo, V. Fernandes, J. Freitas outpatient colonoscopy clinic after a posi- computed tomography (CT) scan 1 week Department of Gastroenterology, tive fecal occult blood test during screen- after the procedure revealed no abnormal Hospital Garcia de Orta, Almada, Portugal ing for colorectal cancer. Colonoscopy, findings and the patient remained asymp- which was performed with the patient tomatic. sedated, revealed a 12-mm tumor covered Acute appendicitis is the most frequent References by normal, smooth mucosa at the site of acute abdominal emergency seen in de- 1 Oliak D, Yamini D, Udani VM et al. Can per- forated appendicitis be diagnosed preopera- the appendicular orifice. A biopsy was veloped countries. Its most common com- tively based on admission factors? J Gastro- taken, but this led to an immediate puru- plication is perforation and this may be intest Surg 2000; 4: 470–474 lent discharge occurring from the lesion followed by abscess formation [1]. Colo- 2 Ohtaka M, Asakawa A, Kashiwagi A et al. (●" Video 1). Therefore, a diagnosis of a noscopic diagnosis and treatment of a Pericecal appendiceal abscess with drainage periappendicular abscess was incidentally periappendicular abscess is rare [2]. In during colonoscopy. Gastrointest Endosc 1999; 49: 107–109 established. this case a periappendicular abscess was 3 Antevil J, Brown C. Percutaneous drainage After the patient had recovered from the incidentally discovered and drained dur- and interval appendectomy. In: Scott-Turner sedation, he was specifically questioned ing a colonoscopy. -

Immune Functions of the Vermiform Appendix
The Proceedings of the International Conference on Creationism Volume 3 Print Reference: Pages 335-342 Article 30 1994 Immune Functions of the Vermiform Appendix Frank Maas Follow this and additional works at: https://digitalcommons.cedarville.edu/icc_proceedings DigitalCommons@Cedarville provides a publication platform for fully open access journals, which means that all articles are available on the Internet to all users immediately upon publication. However, the opinions and sentiments expressed by the authors of articles published in our journals do not necessarily indicate the endorsement or reflect the views of DigitalCommons@Cedarville, the Centennial Library, or Cedarville University and its employees. The authors are solely responsible for the content of their work. Please address questions to [email protected]. Browse the contents of this volume of The Proceedings of the International Conference on Creationism. Recommended Citation Maas, Frank (1994) "Immune Functions of the Vermiform Appendix," The Proceedings of the International Conference on Creationism: Vol. 3 , Article 30. Available at: https://digitalcommons.cedarville.edu/icc_proceedings/vol3/iss1/30 IMMUNE FUNCTIONS OF THE VERMIFORM APPENDIX FRANK MAAS, M.S. 320 7TH STREET GERVAIS, OR 97026 KEYWORDS Mucosal immunology, gut-associated lymphoid tissues. immunocompetence, appendix (human and rabbit), appendectomy, neoplasm, vestigial organs. ABSTRACT The vermiform appendix Is purported to be the classic example of a vestigial organ, yet for nearly a century it has been known to be a specialized organ highly infiltrated with lymphoid tissue. This lymphoid tissue may help protect against local gut infections. As the vertebrate taxonomic scale increases, the lymphoid tissue of the large bowel tends to be concentrated In a specific region of the gut: the cecal apex or vermiform appendix. -

Vomiting in Children
Vomiting in Children T. Matthew Shields, MD,* Jenifer R. Lightdale, MD, MPH* *Division of Pediatric Gastroenterology and Nutrition, UMass Memorial Children’s Medical Center, Department of Pediatrics, University of Massachusetts Medical School, Worcester, MA Education Gaps 1. There are at least 4 known physiologic pathways that can trigger vomiting, 3 of which are extraintestinal. 2. Understanding which pathway is causing a patient’s vomiting will help determine best treatment options, including which antiemetic is most likely to be helpful to mitigate symptoms. 3. Bilious emesis in a newborn should indicate bowel obstruction. 4. Cyclic episodes of vomiting may be indicative of a migraine variant. Objectives After completing this article, readers should be able to: 1. Understand the main pathways that trigger vomiting via the emetic reflex. 2. Differentiate among acute, chronic, and cyclic causes of vomiting. 3. Create a broad differential diagnosis for vomiting based on a patient’s history, physical examination findings, and age. 4. Recognize red flag signs and symptoms of vomiting that require emergent evaluation. 5. Recognize when to begin an antiemetic medication. AUTHOR DISCLOSURE Dr Shields has 6. Select antiemetic medications according to the presumed underlying disclosed no financial relationships relevant to this article. Dr Lightdale has disclosed that she mechanism of vomiting. has a research grant from AbbVie and receives honorarium as a speaker for Mead Johnson. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device. Vomiting is a common symptom of numerous underlying conditions for which children frequently present for healthcare. Although vomiting can originate from ABBREVIATIONS the gastrointestinal (GI) tract itself, it can also signal more generalized, systemic 5-HT 5-hydroxytryptamine disorders. -
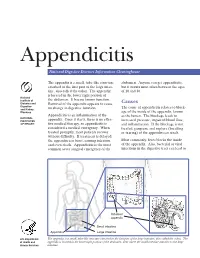
Appendicitis
Appendicitis National Digestive Diseases Information Clearinghouse The appendix is a small, tube-like structure abdomen. Anyone can get appendicitis, attached to the first part of the large intes- but it occurs most often between the ages tine, also called the colon. The appendix of 10 and 30. is located in the lower right portion of National Institute of the abdomen. It has no known function. Diabetes and Removal of the appendix appears to cause Causes Digestive The cause of appendicitis relates to block- and Kidney no change in digestive function. Diseases age of the inside of the appendix, known Appendicitis is an inflammation of the as the lumen. The blockage leads to NATIONAL INSTITUTES appendix. Once it starts, there is no effec- increased pressure, impaired blood flow, OF HEALTH tive medical therapy, so appendicitis is and inflammation. If the blockage is not considered a medical emergency. When treated, gangrene and rupture (breaking treated promptly, most patients recover or tearing) of the appendix can result. without difficulty. If treatment is delayed, the appendix can burst, causing infection Most commonly, feces blocks the inside and even death. Appendicitis is the most of the appendix. Also, bacterial or viral common acute surgical emergency of the infections in the digestive tract can lead to Inflamed appendix Small intestine Appendix Large intestine U.S. Department The appendix is a small, tube-like structure attached to the first part of the large intestine, also called the colon. The of Health and appendix is located in the lower right portion of the abdomen, near where the small intestine attaches to the large Human Services intestine. -

Journal of Pediatric Surgery Case Reports 40 (2019) 71–75
Journal of Pediatric Surgery Case Reports 40 (2019) 71–75 Contents lists available at ScienceDirect Journal of Pediatric Surgery Case Reports journal homepage: www.elsevier.com/locate/epsc Laparoscopic resection of pancreatic neck lesion with Roux-en-Y T pancreatico-jejunostomy ∗ ∗ Martin Sidlera, , Pratik Shahb, Michael Ashworthc, Paolo De Coppia, a Specialist Neonatal and Paediatric Surgery, Great Ormond Street Hospital, London, United Kingdom b Paediatric Endocrinology, Great Ormond Street Hospital, London, United Kingdom c Paediatric Histopathology, Great Ormond Street Hospital, London, United Kingdom ABSTRACT Background: Congenital hyperinsulinism is a rare disease and patients not re- sponding to medical treatment need near-total or partial pancreatectomy, dependent on whether they have diffuse or focal hyperinsulinism, respectively. While laparoscopic technique for distal and for total pancreatectomy has been developed, minimally invasive resection of the pancreatic neck with pancreatico-jejunostomy has not been reported in children before. Case summary: A 2-year old boy suffered from congenital hyperinsulinism, which was refractory to high-dose medical treatment. The nuclear-medicine scanrevealed a focal lesion of the pancreatic neck, hence partial pancreatectomy was indicated. On laparoscopy, a slightly prominent tissue mass was apparent in the area of the pancreatic neck. We proceeded with laparoscopic mobilisation of the pancreas from the underlying splenic vessels and resected the pancreatic neck and adjacent parts of the body and the head. After macroscopic resection of the mass, the patient's intraoperative blood glucose levels increased to a point where insulin had to be substituted. To drain the pancreatic tail, we formed an end-to-side anastomosis in the proximal Jejunum and brought the open end to the pancreatic tail and performed a laparoscopic pancreatico-jejunostomy. -

Gastroparesis and Dumping Syndrome: Current Concepts and Management
Journal of Clinical Medicine Review Gastroparesis and Dumping Syndrome: Current Concepts and Management Stephan R. Vavricka 1,2,* and Thomas Greuter 2 1 Center of Gastroenterology and Hepatology, CH-8048 Zurich, Switzerland 2 Department of Gastroenterology and Hepatology, University Hospital Zurich, CH-8091 Zurich, Switzerland * Correspondence: [email protected] Received: 21 June 2019; Accepted: 23 July 2019; Published: 29 July 2019 Abstract: Gastroparesis and dumping syndrome both evolve from a disturbed gastric emptying mechanism. Although gastroparesis results from delayed gastric emptying and dumping syndrome from accelerated emptying of the stomach, the two entities share several similarities among which are an underestimated prevalence, considerable impairment of quality of life, the need for a multidisciplinary team setting, and a step-up treatment approach. In the following review, we will present an overview of the most important clinical aspects of gastroparesis and dumping syndrome including epidemiology, pathophysiology, presentation, and diagnostics. Finally, we highlight promising therapeutic options that might be available in the future. Keywords: gastroparesis; dumping syndrome; pathophysiology; clinical presentation; treatment 1. Introduction Gastroparesis and dumping syndrome both evolve from a disturbed gastric emptying mechanism. While gastroparesis results from significantly delayed gastric emptying, dumping syndrome is a consequence of increased flux of food into the small bowel [1,2]. The two entities share several important similarities: (i) gastroparesis and dumping syndrome are frequent, but also frequently overlooked; (ii) they affect patient’s quality of life considerably due to possibly debilitating symptoms; (iii) patients should be taken care of within a multidisciplinary team setting; and (iv) treatment should follow a step-up approach from dietary modifications and patient education to pharmacological interventions and, finally, surgical procedures and/or enteral feeding. -

Endoscopic Approaches to Gastroparesis
Endoscopic Approaches to Gastroparesis Kevin Liu, MD,1 Thomas Enke, MD,2 and Aziz Aadam, MD1 1Division of Gastroenterology, Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, Illinois 2Department of Medicine, Feinberg School of Medicine, Northwestern University, Chicago, Illinois Corresponding author: Abstract: Gastroparesis is a complex syndrome with multiple Dr Aziz Aadam underlying etiologies and pathophysiologies that can cause signif- 676 North Saint Clair St, Suite 1400 icant morbidity for patients. Currently, there are limited effective Chicago, IL 60611 and durable medical and surgical treatments for patients with Tel: (312) 695-3364 E-mail: [email protected] gastroparesis. As such, there has been recent innovation and development in minimally invasive endoscopic treatments for gastroparesis. Endoscopic therapies that have been investigated for gastroparesis include enteral feeding tube placement, intrapyloric botulinum toxin injection, transpyloric stenting, gastric peroral endoscopic myotomy, and gastric electrical stimulation. This article aims to assess the effectiveness of current endoscopic therapies, as well as discuss future directions for endoscopic therapies, in the management of gastroparesis. astroparesis is defined as a complex syndrome of symp- toms, including early satiety, postprandial fullness, nausea, vomiting, bloating, and upper abdominal pain, with a Gcorresponding objective delay in gastric emptying in the absence of mechanical obstruction.1 The primary etiologies