REMARKABLE NURSES Then and Now, We Remain Remarkable!
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minority Percentages at Participating Newspapers
Minority Percentages at Participating Newspapers Asian Native Asian Native Am. Black Hisp Am. Total Am. Black Hisp Am. Total ALABAMA The Anniston Star........................................................3.0 3.0 0.0 0.0 6.1 Free Lance, Hollister ...................................................0.0 0.0 12.5 0.0 12.5 The News-Courier, Athens...........................................0.0 0.0 0.0 0.0 0.0 Lake County Record-Bee, Lakeport...............................0.0 0.0 0.0 0.0 0.0 The Birmingham News................................................0.7 16.7 0.7 0.0 18.1 The Lompoc Record..................................................20.0 0.0 0.0 0.0 20.0 The Decatur Daily........................................................0.0 8.6 0.0 0.0 8.6 Press-Telegram, Long Beach .......................................7.0 4.2 16.9 0.0 28.2 Dothan Eagle..............................................................0.0 4.3 0.0 0.0 4.3 Los Angeles Times......................................................8.5 3.4 6.4 0.2 18.6 Enterprise Ledger........................................................0.0 20.0 0.0 0.0 20.0 Madera Tribune...........................................................0.0 0.0 37.5 0.0 37.5 TimesDaily, Florence...................................................0.0 3.4 0.0 0.0 3.4 Appeal-Democrat, Marysville.......................................4.2 0.0 8.3 0.0 12.5 The Gadsden Times.....................................................0.0 0.0 0.0 0.0 0.0 Merced Sun-Star.........................................................5.0 -

Infographic Placements
MEDIA OUTLET NAME CITY STATE READERSHIP Your Alaska Link Anchorage AK 8,989 Kodiak Daily Mirror Kodiak AK 6,484 Seward Journal Delta Junction AK 5,001 Delta Wind Delta Junction AK 1,200 Fairbanks Daily News-Miner Fairbanks AK 434,431 Gadsden Times Gadsden AL 71,778 Alex City Outlook Alexander City AL 50,933 Wetumpka Herald Wetumpka AL 37,608 Courier Journal Florence AL 24,563 Arab Tribune Arab AL 13,952 Elba Clipper Elba AL 10,969 Randolph Leader Roanoke AL 6,449 Cutoff News Bessemer AL 5,963 Montgomery Independent Montgomery AL 4,632 Tallassee Tribune Alexander City AL 4,500 Southeast Sun Enterprise AL 4,337 Tuskegee News Tuskegee AL 3,294 Moulton Advertiser Moulton AL 3,073 Opelika Observer Online Opelika AL 3,000 WHEP 1310 Foley AL 613 Times Daily's TN Valley Search Decatur AL 5,700 Times Daily's TN Valley Brides Decatur AL 5,968 Northwest Arkansas Democrat-Gazette Online Fayetteville AR 159,356 Log Cabin Democrat Conway AR 67,156 Courier News Russellville AR 47,028 River Valley Now Russellville AR 15,000 El Dorado News-Times Online El Dorado AR 8,601 ASU Herald State University AR 6,698 Saline Courier Benton AR 5,511 Waldron News Waldron AR 3,158 De Queen Bee De Queen AR 2,204 Newton County Times Jasper AR 1,665 Radio Works Camden AR 1,500 Madison County Record Huntsville AR 1,221 Bray Online Magnolia AR 1,000 Dewitt Era Enterprise Online Dewitt AR 1,000 Southern Progressive Online Horseshoe Bend AR 300 Harrison Daily Times Harrison AR 53,294 Ashley County Ledger Hamburg AR 8,974 Ashley News Observer Crossett AR 1,001 The Seward Journal -

Obituary Index 3Dec2020.Xlsx
Last First Other Middle Maiden ObitSource City State Date Section Page # Column # Notes Naber Adelheid Carrollton Gazette Carrolton IL 9/26/1928 1 3 Naber Anna M. Carrollton Gazette Patriot Carrolton IL 9/23/1960 1 2 Naber Bernard Carrollton Gazette Carrolton IL 11/17/1910 1 6 Naber John B. Carrollton Gazette Carrolton IL 6/13/1941 1 1 Nace Joseph Lewis Carthage Republican Carthage IL 3/8/1899 5 2 Nachtigall Elsie Meler Chicago Daily News Chicago IL 3/27/1909 15 1 Nachtigall Henry C. Chicago Daily News Chicago IL 11/30/1909 18 4 Nachtigall William C. Chicago Daily News Chicago IL 10/5/1925 38 3 Nacke Mary Schleper Effingham Democrat Effingham IL 8/6/1874 3 4 Nacofsky Lillian Fletcher Chicago Daily News Chicago IL 2/22/1922 29 1 Naden Clifford Kendall County Journal Yorkville IL 11/8/1990 Countywide 2 2 Naden Earl O. Waukegan News Sun Waukegan IL 11/2/1984 7A 4 Naden Elizabeth Broadbent Kendall County Journal Yorkville IL 1/17/1900 8 4 Naden Isaac Kendall County Journal Yorkville IL 2/28/1900 4 1 Naden James Darby Kendall County Journal Yorkville IL 12/25/1935 4 5 Naden Jane Green Kendall County Journal Yorkville IL 4/10/1912 9 3 Naden John M. Kendall County Journal Yorkville IL 9/13/1944 5 4 Naden Martha Kendall County Journal Yorkville IL 12/6/1866 3 1 Naden Obadiah Kendall County Journal Yorkville IL 11/8/1911 1 1 Naden Samuel Kendall County Journal Yorkville IL 6/17/1942 7 1 Naden Samuel Mrs Kendall County Journal Yorkville IL 8/15/1878 4 3 Naden Samuel Mrs Kendall County Journal Yorkville IL 8/8/1878 1 4 Naden Thomas Kendall County -

Blocked Titles - Academic and Public Library Markets Factiva
Blocked Titles - Academic and Public Library Markets Factiva Source Name Source Code Aberdeen American News ABAM Advocate ADVO Akron Beacon Journal AKBJ Alexandria Daily Town Talk ADTT Allentown Morning Call XALL Argus Leader ARGL Asbury Park Press ASPK Asheville Citizen-Times ASHC Baltimore Sun BSUN Battle Creek Enquirer BATL Baxter County Newspapers BAXT Belleville News-Democrat BLND Bellingham Herald XBEL Brandenton Herald BRDH Bucryus Telegraph Forum BTF Burlington Free Press BRFP Centre Daily Times CDPA Charlotte Observer CLTO Chicago Tribune TRIB Chilicothe Gazette CGOH Chronicle-Tribune CHRT Cincinnati Enquirer CINC Clarion-Ledger (Jackson, MS) CLDG Cochocton Tribune CTOH Columbus Ledger-Enquirer CLEN Contra Costa Times CCT Courier-News XCNW Courier-Post CPST Daily Ledger DLIN Daily News Leader DNLE Daily Press DAIL Daily Record DRNJ Daily Times DTMD Daily Times Adviser DTA Daily World DWLA Democrat & Chronicle (Rochester, NY) DMCR Des Moines Register DMRG Detroit Free Press DFP Detroit News DTNS Duluth News-Tribune DNTR El Paso Times ELPS Florida Today FLTY Fort Collins Coloradoan XFTC Fort Wayne News Sentinel FWNS Fort Worth Star-Telegram FWST Grand Forks Herald XGFH Great Falls Tribune GFTR Green Bay Press-Gazette GBPG Greenville News (SC) GNVL Hartford Courant HFCT Harvard Business Review HRB Harvard Management Update HMU Hattiesburg American HATB Herald Times Reporter HTR Home News Tribune HMTR Honolulu Advertiser XHAD Idaho Statesman BSID Iowa City Press-Citizen PCIA Journal & Courier XJOC Journal-News JNWP Kansas City Star -

Community Health Needs Assessment 2019
Community Health Needs Assessment 2019 OSF SAINT ANTHONY MEDICAL CENTER WINNEBAGO COUNTY CHNA 2019 | Winnebago County 2 TABLE OF CONTENTS Executive Summary .............................................................................................................................. 3 Introduction ............................................................................................................................................. 5 Methods ................................................................................................................................................. 7 Chapter 1. Community Themes/Demographic Profile 1.1 Population ....................................................................................................................... 11 1.2 Age, Gender and Race Distribution ....................................................................... 12 1.3 Household/Family ....................................................................................................... 14 1.4 Economic Information ................................................................................................ 16 1.5 Education ........................................................................................................................ 18 1.6 Telehealth ........................................................................................................................ 20 1.7 Key Takeaways from Chapter 1 ............................................................................. 21 Chapter 2. Prevention -
Declaration of Brandon Schwartz in Support of Plaintiff's Motion For
1 2 3 4 5 6 7 8 9 UNITED STATES DISTRICT COURT SOUTHERN DISTRICT OF CALIFORNIA 10 11 RICHARD WINTERS, individually, and on behalf of other members of the general public similarly Case No. 3:20-cv-00468-BAS-BGS 12 situated, DECLARATION OF BRANDON SCHWARTZ 13 Plaintiff, REGARDING NOTICE PLAN 14 IMPLEMENTATION AND SETTLEMENT vs. ADMINISTRATION 15 TWO TOWNS CIDERHOUSE INC., Judge: Hon. Cynthia Bashant 16 Defendant. 17 18 19 20 21 22 23 24 25 26 27 28 Winters et al. v. Two Towns Ciderhouse Inc., No. 3:20-cv-00468-BAS-BGS DECLARATION OF BRANDON SCHWARTZ 1 I, Brandon Schwartz, declare: 2 1. I am the Director of Notice for Postlethwaite & Netterville, APAC (“P&N”), a full-service 3 administration firm providing legal administration services, including the design, development, and 4 implementation of unbiased complex legal notification programs. 5 2. On September 21, 2020, the Court approved the Notice Plan and appointed P&N as the 6 Claims Administrator in the Order: (1) Preliminarily Approving Class Action Settlement; (2) Conditionally 7 Approving Proposed Settlement Class; and (3) Setting Hearing of Final Approval of Settlement (the 8 “Order”). The Court certified a Class defined as: 9 All persons within the United States who purchased the following 2 Towns Products 10 as consumers within four years prior to the filing of the original Complaint until the 11 Class Notice Date: Bright Cider, Easy Squeezy, Pacific Pineapple, Made Marion, 12 Ginja Ninja, or Outcider, Bad Apple, Cherried Away, Cot in the Act, Sun’s Out 13 Saison, Nice & Naughty, Rhubarbarian, Pearadise, Prickly Pearadise, Serious 14 Scrump, and Imperial Hop & Stalk. -
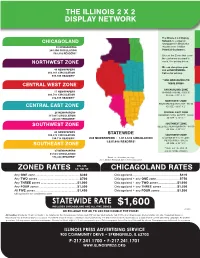
Illinois Display Easy Ad Or 2X2” Network
THE ILLINOIS 2 X 2 DISPLAY NETWORK The Illinois 2 x 2 Display Network is a group of CHICAGOLAND newspapers in Illinois that 50 NEWSPAPERS reaches over 1 million 264,900 CIRCULATION Potential Customers. 503,310 READERS* Choose the Zones that cover the customers you want to reach. See pricing below. NORTHWEST ZONE We can also place your 46 NEWSPAPERS 2x2 ad NATIONWIDE. 262,161 CIRCULATION Call us for pricing. 498,106 READERS* **ADD NEWSPAPERS TO THESE ZONES: CENTRAL WEST ZONE CHICAGOLAND ZONE 55 NEWSPAPERS CHICAGO TRIBUNE - $200.00 206,783 CIRCULATION AD SIZE - 3.22” X 3.5” 392,888 READERS* NORTHWEST ZONE ROCKFORD REGISTER STAR - $50.00 CENTRAL EAST ZONE AD SIZE - 3.625” X 2” 26 NEWSPAPERS CENTRAL EAST ZONE 117,935 CIRCULATION CHAMPAIGN NEWS-GAZETTE - $50.00 224,077 READERS* AD SIZE - 3.13” X 2” SOUTHWEST ZONE SOUTHWEST ZONE BELLEVILLE NEWS-DEMOCRAT - $50.00 AD SIZE - 3.22” X 2” 26 NEWSPAPERS 100,375 CIRCULATION STATEWIDE SOUTHWEST ZONE 190,713 READERS* 230 NEWSPAPERS • 1,013,678 CIRCULATION IL EDITION OF THE ST. LOUIS 1,925,988 READERS* POST-DISPATCH - $50.00 AD SIZE - 3.22” X 2” SOUTHEAST ZONE ** MUST BUY THE ZONE TO 27 NEWSPAPERS ADD ON PAPERS SPECIFIED 61,524 CIRCULATION 116,896 READERS* *Based on 1.9 readers per copy. 2011, Newton Research, Illinois Press Association NW, CW, ZONED RATES CE, SW, SE CHICAGOLAND RATES Any ONE zone .........................................................$360 Chicagoland .............................................................$410 Any TWO zones ......................................................$700 Chicagoland + any ONE zone ..............................$750 Any THREE zones ...............................................$1,000 Chicagoland + any TWO zones ........................$1,050 Any FOUR zones .................................................$1,300 Chicagoland + any THREE zones ....................$1,350 All FIVE zones ......................................................$1,450 Chicagoland + any FOUR zones ......................$1,500 Chicagoland is not considered a zone. -

Visibility Reports
Strong Growth And Increased Demand Brings Positive Changes For KEEN Utility™ English Story Number: LA75593 Clear Time Dec 08, 2015 8:00 AM ET View Release Assets What did I send with my releases? Distribution Where did my release appear online? 196 91,458,259 Traffic What traffic did my release generate? 263 2,191 29 Audience Who are the audiences viewing my release? 160 17 Engagement How are people engaging with my release? 3 Industry Benchmarks On a scale of 1 - 100, how this release performed compared to other similar releases. 56 total visibility 63 38 68 distribution traffic audience 20 engagement Distribution 196 91,458,259 Websites Total Potential Audience Distribution Summary See the types of websites your release posted to, and the industries they cover. Media Type Website Industry Broadcast Media Newspaper Media & Information Financial News & Information Service Blog Retail & Consumer Blog-Parental Influencers The rest Business Services Other Media Type Websites Website Industry Websites Broadcast Media 86 Media & Information 175 Newspaper 78 Financial 9 News & Information Service 20 Retail & Consumer 8 Blog 5 Business Services 2 Blog-Parental Influencers 3 Other 2 Portal 2 Total Number of Websites 196 Trade Publications 2 Total Number of Websites 196 Distribution Details The details of each component of your online distribution. Online Distribution The details of each site that posted your release. 196 postings to websites on our network have been found, with a total potential audience of 91,458,259 unique visitors -

Jury Demand. Filing Fee $ 350, Receipt Number 0
GateHouse Media, Inc. et al v. That's Great News, LLC Doc. 1 Att. 1 GateHouse Media, Inc. List of Publications EXHIBIT A Masthead City State Daily Siftings Herald Arkadelphia AR Arkadelphia Extra Arkadelphia AR Gurdon Times Gurdon AR The Sun Times Heber Springs AR Daily World TMC Helena AR The Daily World Helena AR Hope Star Hope AR Star Extra Hope AR Nevada County Picayune Hope AR Newport Independent Newport AR Stuttgart Daily Leader Stuttgart AR The Xtra Stuttgart AR The Arsenel Sentinel White Hall AR The White Hall Journal White Hall AR Gridley Herald Gridley CA The Gridley Shopping News Gridley CA Weed Press Mt Shasta CA Dunsmuir News Mt Shasta CA Mt Shasta Herald Mt Shasta CA Super Saver Advertiser Mt Shasta CA The Daily Independent Ridgecrest CA Super Tuesday Ridgecrest CA Midway Driller Taft CA Bargain Hunter Taft CA Siskiyou Daily News Yreka CA The Link Yreka CA LaJunta Tribune Democrat LaJunta CO The Ag Journal LaJunta CO The Fowler Tribune LaJunta CO Bent County Democrat Las Pimas CO Norwich Bulletin Norwich CT Colchester Bulletin Norwich CT Shop Local Shoreline Norwich CT Shop Local Town and County Norwich CT Brandywine Community Publication Dover DE Dover Post Dover DE Hockessin-Greenville-Pike Creek Community Publication Dover DE Milford Beacon Dover DE The Airlifter Dover DE Smyrna/Clayton Sun Times Dover DE The Middletown Transcript Dover DE The Sussex Countian Dover DE The Express Dover DE Hamburg Reporter Hamburg IA Abingdon Argus-Sentinel Abindon IL Press Addison/Bensenville/Wood Dale IL The Times Record Aledo IL Town -
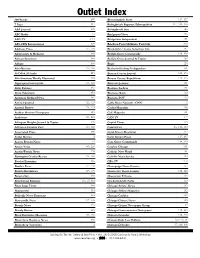
Outlet Index
Outlet Index 600 Words 207 Bloomingdale Press 117, 137 7 Days 217 Bolingbrook Reporter/Metropolitan 117, 140, 146 ABA Journal 185 Bolingbrook Sun 146 ABC Radio 31 Bridgeport News 226 ABC-TV 2, 16 Bridgeview Independent 151 ABS-CBN International 197 Brighton Park/McKinley Park Life 226 Addison Press 117, 136 Brookfield / Lyons Suburban Life 137 Adolescents & Medicine 185 Buffalo Grove Countryside 119, 128 African-Spectrum 189 Buffalo Grove Journal & Topics 128 Afrique 189 Bugle 126 Afro-Netizen 113, 189 Burbank-Stickney Independent 151 Al-Offok Al-Arabi 215 Bureau County Journal 121, 176 Alfa American Weekly Illustrated 203 Bureau County Republican 121, 176 Algonquin Countryside 118, 128 Business Journal 101 Alsip Express 151 Business Ledger 101 Alton Telegraph 153 Business Week 182 American Medical News 182 BusinessPOV 113 Antioch Journal 122, 123 Cable News Network - CNN 2 Antioch Review 118, 123 Cachet Magazine 190 Arabian Horizon Newspaper 215 Café Magazine 101 Arabstreet 113, 215 CAN TV 1, 7 Arlington Heights Journal & Topics 128 Capital Times 153 Arlington Heights Post 119, 128 Capitol Fax Sec 1:34, 109 Associated Press 108 Carol Stream Examiner 137 At the Movies 2 Carol Stream Press 117, 137 Aurora Beacon News 91 Cary-Grove Countryside 118, 129 Austin Voice 189, 224 Catalyst Chicago 101 Austin Weekly News 224 Catholic New World 101 Barrington Courier-Review 118, 128 Catholic News Service 109 Bartlett Examiner 136 CBS-TV 2, 8 Bartlett Press 117, 136 Champaign News Gazette 154 Batavia Republican 117, 136 Charleston Times-Courier 110, -

CFNIL GRANT COMMUNICATION GUIDELINES PURPOSE This Document Provides Guidance for Fulfilling Your Requirements About Publicizing Your Grant
CFNIL GRANT COMMUNICATION GUIDELINES PURPOSE This document provides guidance for fulfilling your requirements about publicizing your grant. The Community Foundation of Northern Illinois (CFNIL) requires recipients to publicize their grant in order to inform the community about your work and inspire continuing support. ACKNOWLEDGMENT REQUIREMENTS Please acknowledge your organization’s grant in one or more of the following ways: SEND A PRESS RELEASE Send out a press release to local news organizations to inform them about your project and the supporting CFNIL grant. A list of regional media contacts can be found on the reverse side of this document. Press release and cover email templates are found at cfnil.org/grant-resources. Boilerplate language about CFNIL is included in the press release template and found below. CFNIL would be happy to provide a quote for your press release. SHARE WITH YOUR ESTABLISHED AUDIENCES We encourage your organization to share information about your grant through the methods you typically use to communicate with your followers, such as newsletters (print or digital), annual reports, and social media. When announcing the grant on CFNIL @the_cfnil social media, make sure to tag us in your posts. Using great images can help boost interest in social media content; we’re happy to help create images, infographics, and photo layouts for your social media feeds -- contact us! @the_cfnil TheCFNIL Grants made for events offer many additional opportunities for promotion. Add CFNIL as a co-host on your Facebook event, and it will appear to all our followers, too. Include the CFNIL logo on event signage, programs, or t-shirts. -
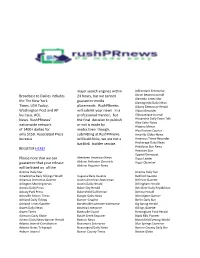
Broadcast to Dailies Includes the the New York Times, USA Today
major search engines within Adirondack Enterprise Broadcast to Dailies includes 24 hours, but we cannot Akron Beacon Journal Alameda Times-Star the The New York guarantee media Alamogordo Daily News Times, USA Today, placements. RushPRnews Albany Democrat-Herald Washington Post and AP will submit your news in a Albion Recorder bureaus, AOL professional manner, but Albuquerque Journal News. RushPRnews’ the final decision to publish Alexandria Daily Town Talk Alice Echo-News nationwide network or not is made by Altoona Mirror of 1400+ dailies for media.Even though, Alva Review-Courier only $150. Associated Press submitting at RushPRnews Amarillo Globe-News bureaus will build links, we are not a Americus Times-Recorder Anchorage Daily News backlink builder service. Andalusia Star News REGISTER HERE! Anniston Star Appeal-Democrat Please note that we can Aberdeen American News Argus Leader guarantee that your release Abilene Reflector Chronicle Argus Observer Abilene Reporter-News will be listed on all the Arizona Daily Star Arizona Daily Sun Arkadelphia Daily Siftings Herald Augusta Daily Gazette Bedford Gazette Arkansas Democrat-Gazette Austin American-Statesman Bellevue Gazette Arlington Morning News Austin Daily Herald Bellingham Herald Artesia Daily Press Baker City Herald Belvidere Daily Republican Asbury Park Press Bakersfield Californian Benicia Herald Asheville Citizen-Times Bangor Daily News Bennington Banner Ashland Daily Tidings Banner-Graphic Berlin Daily Sun Ashland Times-Gazette Bartlesville Examiner-Enterprise Big Spring Herald