Extra Corporeal Oxygenation (Ecmo) Learning Package
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Incidence of Microemboli to the Brain Is Less with Endarterectomy Than with Percutaneous Revascularization with Distal filters Or flow Reversal
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector From the Southern Association for Vascular Surgery The incidence of microemboli to the brain is less with endarterectomy than with percutaneous revascularization with distal filters or flow reversal Naren Gupta, MD, PhD,a Matthew A. Corriere, MD, MS,a,c Thomas F. Dodson, MD,a Elliot L. Chaikof, MD, PhD,a Robert J. Beaulieu, BS,b James G. Reeves, MD,a Atef A. Salam, MD,a and Karthikeshwar Kasirajan, MD,a Atlanta, Ga Background: Current data suggest microembolization to the brain may result in long-term cognitive dysfunction despite the absence of immediate clinically obvious cerebrovascular events. We reviewed a series of patients treated electively with carotid endarterectomy (CEA), carotid artery stenting (CAS) with distal filters, and carotid stenting with flow reversal (FRS) monitored continuously with transcranial Doppler scan (TCD) during the procedure to detect microembolization rates. Methods: TCD insonation of the M1 segment of the middle cerebral artery was conducted during 42 procedures (15 CEA, 20 CAS, and 7 FRS) in 41 patients seen at an academic center. One patient had staged bilateral CEA. Ipsilateral microembolic signals (MESs) were divided into three phases: preprotection phase (until internal carotid artery [ICA] cross-shunted or clamped if no shunt was used, filter deployed, or flow reversal established), protection phase (until clamp/shunt was removed, filter removed, or antegrade flow re-established), and postprotection phase (after clamp/ shunt was removed, filter removed, or antegrade flow re-established). Descriptive statistics are reported as mean ؎ SE for continuous variables and N (%) for categorical variables. -

Research Article Endothelial Dysfunction of Patients with Peripheral Arterial Disease Measured by Peripheral Arterial Tonometry
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Hindawi Publishing Corporation International Journal of Vascular Medicine Volume 2016, Article ID 3805380, 6 pages http://dx.doi.org/10.1155/2016/3805380 Research Article Endothelial Dysfunction of Patients with Peripheral Arterial Disease Measured by Peripheral Arterial Tonometry Kimihiro Igari, Toshifumi Kudo, Takahiro Toyofuku, and Yoshinori Inoue Division of Vascular and Endovascular Surgery, Department of Surgery, Tokyo Medical and Dental University, 1-5-45 Yushima, Bunkyo-ku, Tokyo 113-8519, Japan Correspondence should be addressed to Kimihiro Igari; [email protected] Received 16 July 2016; Revised 17 September 2016; Accepted 27 September 2016 Academic Editor: Thomas Schmitz-Rixen Copyright © 2016 Kimihiro Igari et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objective. Endothelial dysfunction plays a key role in atherosclerotic disease. Several methods have been reported to be useful for evaluating the endothelial dysfunction, and we investigated the endothelial dysfunction in patients with peripheral arterial disease (PAD) using peripheral arterial tonometry (PAT) test in this study. Furthermore, we examined the factors significantly correlated with PAT test. Methods. We performed PAT tests in 67 patients with PAD. In addition, we recorded the patients’ demographics, including comorbidities, and hemodynamical status, such as ankle brachial pressure index (ABI). Results. In a univariate analysis, the ABI value ( = 0.271, = 0.029) and a history of cerebrovascular disease ( = 0.208, = 0.143) were found to significantly correlatewithPATtest,whichcalculatedthereactivehyperemiaindex(RHI).Inamultivariateanalysis,onlytheABIvalue significantly and independently correlated with RHI ( = 0.254, = 0.041). -

8 Implantable Membrane Oxygenator
Artificial Lung 8 . Cardiopulmonary Bypass - oxgenator 1 Cardiopulmonary Bypass § Cardiopulmonary bypass (CPB), also called heart-lung bypass, allows the temporary replacement of the gas exchange function of the lungs and the blood-pumping function of the heart § The terms pump-oxygenator and heart–lung machine graphically describe the equipment used § By extension, the term is also applies to surgical procedures which take place primarily on the external aspects of the heart, such as creating new routes for blood to reach the distal coronary arteries from the aorta 3 Cardiopulmonary Bypass § As usually employed for cardiac surgery, the heart–lung machine is part of a total, venoarterial cardiopulmonary bypass circuit à meaning that all the venous blood returning to the right heart cavities is collected in the extracorporeal circuit à circulated through the gas exchange device, from where it is pumped back into the arterial tree à thereby “bypassing” the heart cavities and the pulmonary circulation 5 Cardiopulmonary Bypass Scheme of standard operating conditions during cardiopulmonary bypass 6 Cardiopulmonary Bypass 7 Artificial Lung Artificial Lung vs. Natural Lung 8 Artificial Lung vs. Natural Lung § In the natural lungs, the factors underlying exchange across the alveolo-capillary barrier and transport by the blood can be grouped into four classes:- ú The ventilation of the lungs (the volume flow rate of gas) and the composition of the gas mixture to which mixed venous (pulmonary artery) blood will be exposed 9 Artificial Lung vs. Natural Lung § In the natural lungs, the factors underlying exchange across the alveolo-capillary barrier and transport by the blood can be grouped into four classes:- ú The permeability of the materials which separate the gas phase from the blood phase in the pulmonary alveoli 10 Artificial Lung vs. -

Left Atrial to Femoral Artery Full Cardiopulmonary Bypass: a Novel Technique for Descending and Thoracoabdominal Aortic Surgery
Published online: 2019-12-09 Original Article 19 Left Atrial to Femoral Artery Full Cardiopulmonary Bypass: A Novel Technique for Descending and Thoracoabdominal Aortic Surgery Dimitra Papanikolaou, MD1 Chris Savio, BS, CCP1 Mohammad A. Zafar, MBBS1 Leon Freudzon, MD1 Jinlin Wu, MD1 Mohamed Abdelbaky, MD1 Keith J. Pelletier, MBA, MHS, CCP1 Joelle Buntin, MSN, RN, RN-BC1 Thais Faggion Vinholo, BS, MSc1 Bulat A. Ziganshin, MD, PhD1,2 Brian Schwartz, MS, CCP1 John A. Elefteriades, MD, PhD (Hon)1 1 Aortic Institute at Yale-New Haven Hospital, Yale University School Address for correspondence John A. Elefteriades, MD, Aortic Institute of Medicine, New Haven, Connecticut at Yale-New Haven, Yale University School of Medicine, Clinic Building 2 Department of Surgical Diseases, Kazan State Medical University, CB 317, 789 Howard Avenue, New Haven, CT 06519 Kazan, Russia (e-mail: [email protected]). Int J Angiol 2020;29:19–26. Abstract Left atrial-femoral artery (LA-FA) bypass with a centrifugal pump and no oxygenator is commonly used for descending and thoracoabdominal aortic (DTAA) operations, mitigating the deleterious effects of cross-clamping. We present our initial experience performing DTAA replacement under LA-FA (left-to-left) cardiopulmonary bypass (CPB) with an oxygenator. DTAA replacement under LA-FA bypass with an oxygenator was performed in 14 consecutive patients (CPB group). The pulmonary vein and femoral artery (or distal aorta) were cannulated and the full CPB machine were used, including oxygenator, roller pump, pump suckers, and kinetically enhanced drainage. The CPB group was compared with 50 consecutive patients who underwent DTAA replacement utilizing traditional LA-FA bypass without an oxygenator (LA-FA group). -

The Mayo Gibbon Heart-Lung Bypass Machine in the Marc
Mayo Clinic Proceedings Legacy December 2014 Pioneers in Cardiac Surgery: The Mayo Gibbon Heart-Lung Bypass Machine This preliminary report shared the results from animal studies, but by May of that same year, Mayo Clinic had initiated use of the apparatus for human subjects and reported on the outcome in 8 cases.2 These patients had the following conditions: (1) ventricular septal defect, (2) Tetralogy of Fallot, or (3) persistent common atrioventricular canal. Four of the patients survived the surgery, one died shortly after the procedure, two died 3 hours postoperatively, and one died 6 days postoperatively.2 Mayo Clinic continued to study and develop successful surgical treatments in cardiology throughout the ensuing years. More than 60 years have passed since these first attempts, and success in cardiac surgery is directly related to these courageous research pioneers and patients. 1,2,3 This historical line of research in In the March 13, 1955, issue of The Proceedings cardiology also represents another successful of the Staff Meetings of the Mayo Clinic, Dr collaboration between the field of medicine John W. Kirklin and colleagues shared a and industry. International Business Machines preliminary report of their research from the (IBM) aided in the design and development of previous 3 years which tackled the challenges the Mayo Gibbon Heart-Lung Bypass of cardiac surgery. While other types of Machine.1,2,3 surgeries have their own impediments, cardiac surgery is dominated by the need to keep a References patient alive during the procedure while 1. Jones RE, Donald DE, Swan HJ, Harshbarger HG, maintaining the function of the circulatory Kirklin JW, Wood EH. -

New York State Surgical and Invasive Procedure Protocol (NYSSIPP)
State of New York Department of Health Office of Health Systems Management Division of Primary and Acute Care Services New York State Surgical and Invasive Procedure Protocol for Hospitals ~ Diagnostic and Treatment Centers Ambulatory Surgery Centers ~ Individual Practitioners Antonia C. Novello, M.D., M.P.H., Dr.P.H. Commissioner of Health Hon. George E. Pataki Governor – State of New York September 2006 Surgical and Invasive Procedure Protocol September 2006 NEW YORK STATE SURGICAL AND INVASIVE PROCEDURE PROTOCOL (FOR THE PREVENTION OF WRONG PATIENT, WRONG SITE, WRONG SIDE & WRONG INVASIVE PROCEDURE EVENTS) I. STATEMENT OF PURPOSE The State of New York is committed to providing its residents access to quality health care. Hon. George E. Pataki, Governor and Antonia C. Novello M.D., M.P.H., Dr.P.H., Commissioner of Health, continue to work toward a system that reduces medical and surgical errors by commitment to a safe and protected patient care environment. Key to achieving this goal is promoting a culture of safety and strengthening open communication among health care providers, individual practitioners and the patients they serve. One of the goals of Governor Pataki and Commissioner Novello, is the elimination of wrong patient, wrong site, wrong side and wrong invasive procedures, through the development of comprehensive systems that ensure the correct procedure is done on the correct patient on the correct site. Increased practitioner awareness combined with strong provider protocols and standardization will enhance the patient safety measures currently in place. The New York State Surgical and Invasive Procedure Protocol (NYSSIPP) developed by the Procedural and Surgical Site Verification Panel (PSSVP) is intended for all patient care settings and for all individual practitioners. -
Fluorescein Angiography: Preventing and Responding to Complications
Fluorescein Angiography: Preventing and Responding to Complications Jacqueline G. Jaffee, J.D. OMIC Risk Management Specialist PURPOSE OF RISK MANAGEMENT RECOMMENDATIONS OMIC regularly analyzes its claims experience to determine loss prevention measures that our insured ophthalmologists can take to reduce the likelihood of professional liability lawsuits. OMIC policyholders are not required to implement these risk management recommendations. Use your professional judgment in determining the applicability of a given recommendation to their particular patients and practice situation. These loss prevention documents may refer to clinical care guidelines such as the American Academy of Ophthalmology’s Preferred Practice Patterns, peer-reviewed articles, or to federal or state laws and regulations. However, our risk management recommendations do not constitute the standard of care nor do they provide legal advice. If legal advice is desired or needed, consult an attorney. Information contained here is not intended to be a modification of the terms and conditions of the OMIC professional and limited office premises liability insurance policy. Please refer to the OMIC policy for these terms and conditions. Version 1/24/08 Fluorescein angiography (FA) is a diagnostic procedure in which a rapid sequence of photographs is taken to document the blood circulation of the retina/choroid. The dye is usually injected into a vein in the arm, forearm, or hand. While generally well tolerated, angiography is an invasive procedure with associated risks, very rarely but notably of a life-threatening allergic reaction. The following risk management recommendations have been compiled to assist you and your staff so that you may both prevent and better respond to the risks of the procedure. -

Perfusionist
40th Anniversary Edition Perfusionist Bi-monthly publication of The Society of Clinical Perfusion Scientists of Great Britain and Ireland Volume 41, Number 5 September/October 2017 A new high performance heat exchanger intended for precise blood and crystalloid cardioplegia delivery. The ParaCor has a static priming volume of only 28ml and a heat exchanger performance factor of 0.9 @ 500mlpm*. Fully transparent to allow complete visibility. A 100µ filter located on the blood outlet. 100% test regime of the water and blood phase integrity. 7HVWFRQGXFWHGXQGHU$PHULFDQ1DWLRQDO6WDQGDUG*XLGHOLQHV$16,$$0,,62 5 $ 5 &DUGLRYDVFXODULPSODQWVDQGDUWLILFLDORUJDQVr%ORRGJDVH[FKDQJHUV (oxygenators). Scan for more Tel: 01909 470 777 | Email: [email protected] | Web: chalicemedical.com | @ChaliceMedical Perfusionist 1 Publication of The Society of Clinical Perfusion Scientists of Great Britain and Ireland SCPS e-mail address: [email protected] CONTENTS SCPS web site: www.scps.org.uk EDITORIAL 3 The contents of this publication are the property of the FÀILTE, CROESO, DYNNARGH, FAILT ORT, WELCOME 4 Society, and may not be reproduced without its permission. COLLEGE COUNCIL VACANCY 4 NEWS FROM THE EXECUTIVE COMMITTEE 6 Published bi-monthly, this journal is issued free to all entitled NATIONAL SAFETY STANDARDS FOR INVASIVE to it. The views expressed in it are solely those of the PROCEDURES (NATSSIP’S) 7 contributors. Articles of scientific interest related to perfusion MESSAGE TO ALL NESCOT STUDENTS 7 are welcome, as are letters to the Editor regarding -

Principles of Oxygenator Function: Gas Exchange, Heat Transfer, and Operation
Thoracic Key Fastest Thoracic Insight Engine Home Log In Register Categories » More References » About Gold Membership Contact Search... Principles of Oxygenator Function: Gas Exchange, Heat Transfer, and Operation Principles of Oxygenator Function: Gas Exchange, Heat Transfer, and Operation Michael H. Hines INTRODUCTION Since the early 1950s when the development of a heart-lung machine first began, there has been a tremendous evolution of devices and machinery for cardiac support (1,2). However, despite the diversity in designs through the years, they all contain three essential components: a mechanism to circulate the blood, a method of gas exchange for oxygen and carbon dioxide, and some mechanism for temperature control. Chapter 2 has covered the first important component, and we will now focus on the two subsequent elements: gas exchange and heat transfer. And while it is referred to as the “oxygenator,” we must recognize that it is responsible for the movement of both oxygen in, as well as carbon dioxide out. The discussion will start with a basic review of the principles of physics, and then we will apply those principles to the devices used specifically in extracorporeal support, including cardiopulmonary bypass (CPB) and extracorporeal membrane oxygenation (ECMO). You may notice as you go through this chapter that there is a scarcity of trade and manufacturer names. The author has intentionally avoided using these. The intent was primarily to focus on the physiology, physics, and chemistry of the oxygenator and heat exchanger, but also to emphasize the fact that there are a large number of manufacturers producing many products that have all been shown to function extremely well. -
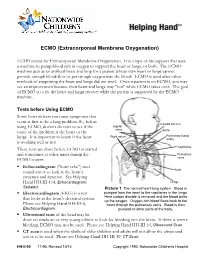
ECMO (Extracorporeal Membrane Oxygenation)
ECMO (Extracorporeal Membrane Oxygenation) ECMO stands for Extracorporeal Membrane Oxygenation. It is a type of life support that uses a machine to pump blood rich in oxygen to support the heart or lungs, or both. The ECMO machine acts as an artificial heart and lung for a patient whose own heart or lungs cannot provide enough blood flow or get enough oxygen into the blood. ECMO is used after other methods of supporting the heart and lungs did not work. Once a patient is on ECMO, you may see an improvement because their heart and lungs may "rest" while ECMO takes over. The goal of ECMO is to let the heart and lungs recover while the patient is supported by the ECMO machine. Tests before Using ECMO Some heart defects can cause symptoms that seem at first to be a lung problem. So, before Carotid arteries using ECMO, doctors do tests to see if the Jugular veins cause of the problem is the heart or the Aorta Right atrium Pulmonary (lung) lungs. It is important to know if the heart artery is working well or not. Capillaries These tests are done before ECMO is started and sometimes at other times during the Pulmonary ECMO course: veins . Echocardiogram ("heart echo") uses Heart sound waves to look at the heart’s structure and function. See Helping Hand HH-III-114, Echocardiogram: Lungs Sedated. Picture 1 The normal heart-lung system. Blood is . Electrocardiogram (EKG) is a test pumped from the heart to the capillaries in the lungs. that looks at the heart's electrical system. -

Cardiopulmonary Bypass Machine Works and Be Able to Help Trouble- Shoot Problems
CCAS CPB Workshop Curriculum Outline Perfusion: What you might not know Scott Lawson, CCP Carrie Striker, CCP Disclosure: Nothing to disclose Objectives: * Demonstrate how the cardiopulmonary bypass machine works and be able to help trouble- shoot problems. * Explain some of the different techniques of cardiopulmonary bypass. I. Heart Lung Machine Brief Overview a. Review blood flow through the heart lung machine (Andropoulos, D. Anesthesia for Congenital Heart Disease. 2nd Ed. 2010, p. 96) Page 1 of 7 II. Anatomy of the Pump a. Propulsion i. Arterial Pump 1. Roller Pump 2. Centrifugal Pump ii. Cardioplegia Pump iii. MUF Pump iv. Vent Pump(s) v. Field Sucker Pump (s) vi. Vacuum: Negative pressure on the venous line for drainage purposes b. Ventilation and Oxygenation i. Blender – Oxygenation Fraction ii. Sweep Gas – Ventilation iii. Exogenous CO2 iv. Vaporizer – Volatile anesthetics c. Monitoring i. Pressures: Arterial, Cardioplegia, MUF ii. Blood Flow: Pump Display, Doppler reading iii. Saturations: Venous, Arterial, Somatic/Cerebral, Flank/Renal iv. Temperatures: Arterial, Venous, Cardioplegia, MUF 1. Temperature Control: a. Heater Cooler v. Air bubble Protection: Bubble Detector, Level Detector vi. Blood Gas/Electrolyte/Hemoglobin and Hematocrit/ACT/Whole Blood Hemostasis Testing: Point of Care Blood Gas and Activated Clotting Time machine, In-line monitoring (CDI, Saturation/Hematocrit), TEG or ROTEM d. Disposables i. Venous Reservoir ii. Oxygenator 1. Integrated Arterial Line Filter 2. Standalone Arterial Line Filter iii. Arterial Venous Loop Size iv. Arterial Raceway size for Roller Pump v. Tubing vi. Cardioplegia vii. Hemoconcentrator viii. Cannulae e. Route of Blood Flow through the actual Heart Lung Machine Page 2 of 7 III. -

Anti-Apolipoprotein A-1 Igg Influences Neutrophil Extracellular Trap
International Journal of Molecular Sciences Article Anti-Apolipoprotein A-1 IgG Influences Neutrophil Extracellular Trap Content at Distinct Regions of Human Carotid Plaques Rafaela F. da Silva 1,2 , Daniela Baptista 1, Aline Roth 1, Kapka Miteva 1 , Fabienne Burger 1, Nicolas Vuilleumier 3,4, Federico Carbone 5,6 , Fabrizio Montecucco 5,6 , François Mach 1 and Karim J. Brandt 1,* 1 Division of Cardiology, Foundation for Medical Researches, Department of Medicine Specialties, Faculty of Medicine, University of Geneva, Av. de la Roseraie 64, 1211 Geneva, Switzerland; [email protected] (R.F.d.S.); [email protected] (D.B.); [email protected] (A.R.); [email protected] (K.M.); [email protected] (F.B.); [email protected] (F.M.) 2 Department of Physiology and Biophysics, Institute of Biological Sciences, Federal University of Minas Gerais, 31270-901 Belo Horizonte, Brazil 3 Department of Diagnostics, Division of Laboratory Medicine, Geneva University Hospitals, 1211 Geneva, Switzerland; [email protected] 4 Department of Medical Specialities, Division of Laboratory Medicine, Faculty of Medicine, 1211 Geneva, Switzerland 5 First Clinic of Internal Medicine, Department of Internal Medicine, University of Genoa, viale Benedetto XV n6, 16132 Genoa, Italy; [email protected] (F.C.); [email protected] (F.M.) 6 IRCCS Ospedale Policlinico San Martino Genoa-Italian Cardiovascular Network, Largo Rosanna Benzi n10, 16132 Genoa, Italy * Correspondence: [email protected]; Tel.: +41-2237-94-647 Received: 9 September 2020; Accepted: 13 October 2020; Published: 19 October 2020 Abstract: Background: Neutrophils accumulate in atherosclerotic plaques. Neutrophil extracellular traps (NET) were recently identified in experimental atherosclerosis and in complex human lesions.