Revised Communicable Disease Reporting Rule Effective December
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mind the Gaps: Investigating Collective Health Aggression
ACTA SCIENTIFIC MICROBIOLOGY (ISSN: 2581-3226) Volume 3 Issue 3 March 2020 Case Review Mind the Gaps: Investigating Collective Health Aggression Victor Lage de Araujo* Received: January 27, 2020 Laboratory Medicine, International Fellow, College of American Pathologist, MSC, Evidence-Based Healthcare (UCL), Brazil Published: February 05, 2020 © All rights are reserved by Victor Lage de *Corresponding Author: Victor Lage de Araújo, Laboratory Medicine, International Fellow, College of American Pathologist, MSC, Evidence-Based Healthcare (UCL), Araujo. Brazil. DOI: 10.31080/ASMI.2020.03.0505 Abstract localise its source – especially if it is an event hitting big numbers of patients, with high severity and quick development of symptoms Whenever one suspects some intoxication, infective epidemics or other collective health harm, it is paramount first to define and [23,24]. An outbreak investigation routine must be early established, with a comprising strategy and pragmatical objectives oriented towards precise diagnosis. Those will grant a realistic assessing of risks for the community, curative measures needed towards the ill and prevention directed to future cases. Healthcare professionals must have great attention towards novel aggressions to men's health and their clinical manifestations; a careful analysis of the available data is needed, in order to avoid being misled by some false assumption that may impair the accuracy of the diagnoses and might delay the needful curative and preventive courses directed towards the population [25]. The determinants of emerging diseases and unusual behaviour of the known microorganisms, health-aggressive mediums and artefacts are multiple; therefore, epidemiologists must consider every item of evidence for each upsurge, including the ecology and environmental issues [1,2]. -

Terrible Typhoid Mary.” Much of What We Know About the Deadly Cook (CCSS ELA-LITERACY.RI 6-10.1-3; CCSS ELA-L.6-10.4-6; Comes from Other People
educator’s guide Terribleby Susan Typhoid Campbell Bartoletti Mary About the Author Susan Campbell Bartoletti is the award winning author of several books for young readers, includ- ing Black Potatoes: The Story of the Great Irish Famine, 1845–1850, winner of the Robert F. Sibert Medal. She lives in Moscow, Pennsylvania. Pre-Reading Activities Ask students to work in small groups and use print and online resources to define the following nine- teenth-century American terms: Industrial Revolution, Urbanization, First Wave of Immigration, Second Wave of Immigration, Tenement Housing, Infectious Disease, Sewage Systems, Germ Theory of Disease, and Personal Hygiene. (CCSS ELA-LITERACY.L.6-10.4-5) The Common Core State Standards (CCSS) are included with the discussions and activities. You can locate the standards at: www.corestandards.org/the- About the Book standards H “Energetic, even charming prose will easily engage Discussion Questions readers.” —School Library Journal, starred review CCSS.ELA-LITERACY.SL.6-10.1 applies to each discussion question. H “Completely captivating.”—Booklist, starred review • Discuss the meaning of the similes, metaphors, H “Excellent nonfiction.” —Horn Book, starred review and allusions that comprise the book’s old-fash- With clarity, verve, and intelligence, Bartoletti presents ioned chapter titles both separately and in rela- the tale of “Typhoid Mary” Mallon, the Irish immigrant tionship to the body of the text. (CCSS ELA-LITERA- cook identified in the early 1900s as the first symptom- CY.L.6-10.5,6; CCSS ELA-LITERACY.RI.6-10.2,4) free carrier of an infectious disease. The author kicks off Mallon’s story with an outbreak of typhoid fever • Based on the information in the book’s early chap- in the Long Island home where she worked as a cook. -

Mary Mallon (1869-1938) and the History of Typhoid Fever
HISTORY IN GASTROENTEROLOGY Annals of Gastroenterology (2013) 26, 1-3 Mary Mallon (1869-1938) and the history of typhoid fever Filio Marineli, Gregory Tsoucalas, Marianna Karamanou, George Androutsos Medical School, University of Athens, Athens, Greece Abstract Mary Mallon was born in 1869 in Ireland and emigrated to the US in 1884. She had worked in a variety of domestic positions for wealthy families prior to settling into her career as a cook. As a healthy carrier of Salmonella typhi her nickname of “Typhoid Mary” had become synonymous with the spread of disease, as many were infected due to her denial of being ill. She was forced into quarantine on two separate occasions on North Brother Island for a total of 26 years and died alone without friends, having evidently found consolation in her religion to which she gave her faith and loyalty. Keywords Typhoid fever, salmonella, Mary Mallon, carrier, New York Ann Gastroenterol 2013; 26 (2): 1-3 Isolating Salmonella Salmonella thus became new scientific knowledge and therefore the contagion mechanisms, as well as the existence Long before the bacillus responsible for the disease was of healthy carriers were relatively in status nascendi [4]. discovered in 1880, Karl Liebermeister had already assumed that the condition was due to a microorganism. He also tried, with his colleagues, to demonstrate that the spread of epidemic was related The contagion to drinking water contaminated by the excrement of patients with typhoid fever [1]. William Budd, a doctor in Bristol who was interested in cholera and in intestinal fevers, demonstrated in Mary Mallon was born in Ireland in 1869 and emigrated 1873, that typhoid fever could be transmitted by a specific toxin to the United States in 1883 or 1884. -

1A Health & Hygiene (H&H) Disease and Prevention
1a Health & Hygiene (H&H) Disease and Prevention 1a Health & Hygiene (H&H)! Disease and Prevention 5 minutes Attendance, Breath of Arrival, and Reminders 50 minutes Lecture 5 minutes Flex time 60 minutes total class time 1a Health & Hygiene (H&H)! Disease and Prevention! Class Reminders Assignments: ! 3a Student Handbook Review Questions (A: 115-118) ! 4a Autobiography and Photo (B-4) ! 7a Written Exam Review Questions (A: 119-130) Quizzes: ! 1b H&H Disease and Prevention Quiz TODAY! ! 5b Kinesiology Quiz (A-73, and A: 75-80) – 25 multiple-choice questions in 20 minutes – Study terms on page A-51 and – AOIs for deltoid, traps, lats, teres major, rhomboids, triceps, and erectors Preparation for upcoming classes: ! 2a Kinesiology: Names and Locations of Bones and Posterior Muscles – Trail Guide: Trapezius – Salvo: Pages 374-375 – Packet E: 17 – RQ Packet A: 120 ! 2b H&H: Tools of the Trade – Salvo: Chapter 3 – Packet F: 1-16 – RQ Packet A: 121-122 Classroom Rules Punctuality - everybody’s time is precious ! Be ready to learn at the start of class; we’ll have you out of here on time ! Tardiness: arriving late, returning late after breaks, leaving during class, leaving early The following are not allowed: ! Bare feet ! Side talking ! Lying down ! Inappropriate clothing ! Food or drink except water ! Phones that are visible in the classroom, bathrooms, or internship You will receive one verbal warning, then you’ll have to leave the room. 1a Health & Hygiene (H&H) Disease and Prevention H-37 Definitions " Miriam-Webster calls Disease-! " a condition -

From “Destroying Angel” to “The Most Dangerous Woman in America”: A
University of Washington Tacoma UW Tacoma Digital Commons History Undergraduate Theses History Spring 6-2016 From “Destroying Angel” to “The oM st Dangerous Woman in America”: A Study of Mary Mallon’s Depiction in Popular Culture Claire Sandoval-Peck [email protected] Follow this and additional works at: https://digitalcommons.tacoma.uw.edu/history_theses Part of the American Popular Culture Commons, Diseases Commons, Public Health Commons, Social History Commons, and the Women's History Commons Recommended Citation Sandoval-Peck, Claire, "From “Destroying Angel” to “The osM t Dangerous Woman in America”: A Study of Mary Mallon’s Depiction in Popular Culture" (2016). History Undergraduate Theses. 25. https://digitalcommons.tacoma.uw.edu/history_theses/25 This Undergraduate Thesis is brought to you for free and open access by the History at UW Tacoma Digital Commons. It has been accepted for inclusion in History Undergraduate Theses by an authorized administrator of UW Tacoma Digital Commons. From “Destroying Angel” to “The Most Dangerous Woman in America”: A Study of Mary Mallon’s Depiction in Popular Culture A Senior Paper Presented in Partial Fulfillment of the Requirements for Graduation Undergraduate History Program of the University of Washington Tacoma by Claire Sandoval-Peck University of Washington Tacoma June 2016 Advisor: Dr. Libi Sundermann 2 Acknowledgments This paper would not have been possible without the support of Diane, my parents and siblings, James in the TLC, Ari, and last but not least, Dr. Libi Sundermann. Thank you for all the encouragement, advice, proofreading, and tea. 1 “Typhoid” Mary Mallon: “A special guest of the City of New York”1 Introduction: If you say the name Mary Mallon to someone today, there is a good chance they will not know who you are talking about. -

Asymptomatic Carriers and Uncertainty the Debate About Asymptomatic Carriers of COVID-19 Began at the Very Beginning of the Pandemic
ARTICLES Hidden Perils Diagnosing asymptomatic disease carriers Ilana Löwy Received: 9 July 2020; Accepted: 19 February 2021; Published: 16 July 2021 Abstract COVID-19, a disease induced by SARS-CoV-2, became a worldwide pandemic while SARS, a disease induced by a closely related virus, SARS-CoV, was successfully contained. This is because COVID-19, unlike SARS, can be spread by people who do not display any symptoms of disease, either because they are in the early stages of the infection or because their infection remains clinically silent. This research article traces the complex history of the diagnosis of symptom-free (or asymptomatic) carriers of pathogens, a term inseparably linked to the rise of the laboratory diagnosis of pathogens. Only such a diagnosis can reveal that an apparently healthy individual harbours dangerous bacteria, parasites, or viruses. The article begins with the iconic story of ‘Typhoid Mary’, a New York cook found to be an asymptomatic carrier of typhoid fever microbes. It then discusses divergent approaches to the treatment of symptom-free carriers of hookworm and controversies around the screening of HIV carriers, especially before the development of anti-retroviral treatments. It concludes with a presentation of the debates on the role of asymptomatic carriers in the spread of COVID-19 and of the differences between the approaches of countries seeking to eliminate this disease, a goal that itself entails tracing and isolation of all asymptomatic carriers of coronavirus, and those trying to contain it, an approach that tolerates the presence of a limited number of ‘invisible’ virus carriers. Keywords Asymptomatic carrier, Typhoid fever, Typhoid Mary, Hookworm, AIDS, COVID-19. -

CST 2008 Released Test Questions, Grade 11 English-Language Arts
CALIFORNIA STANDARDS TEST GRADE Released Test Questions English–Language Arts 11 Introduction - Grade 11 English–Language Arts The following released test questions are taken from the Grade 11 English–Language Arts Standards Test. This test is one of the California Standards Tests administered as part of the Standardized Testing and Reporting (STAR) Program under policies set by the State Board of Education. All questions on the California Standards Tests are evaluated by committees of content experts, including teachers and administrators, to ensure their appropriateness for measuring the California academic content standards in Grade 11 English–Language Arts. In addition to content, all items are reviewed and approved to ensure their adherence to the principles of fairness and to ensure no bias exists with respect to characteristics such as gender, ethnicity, and language. This document contains released test questions from the California Standards Test forms in 2003, 2004, 2005, 2006, 2007, and 2008. First on the pages that follow are lists of the standards assessed on the Grade 11 English–Language Arts Test. Next are released passages and test questions. Following the questions is a table that gives the correct answer for each question, the content standard that each question is measuring, and the year each question last appeared on the test. The following table lists each strand/reporting cluster, the number of items that appear on the exam, and the number of released test questions that appear in this document. NUMBER OF NUMBER -

CPQ Women and Child Health (2019) 1:5 Review Article
CPQ Women and Child Health (2019) 1:5 Review Article CIENT PERIODIQUE School Health Programme: An Indispensable Programme in Child Health Obeagu Getrude Uzoma1 & Obeagu Emmanuel Ifeanyi2,3* 1Department of Nursing Science, Ebonyi State University, Abakaliki, Nigeria 2Medical Laboratory Science, University Health Services, Michael Okpara University of Agriculture, Umudike, Nigeria 3Department of Medical Laboratory Science, Imo State University, Owerri, Nigeria *Correspondence to: Dr. Obeagu Emmanuel Ifeanyi, Department of Medical Laboratory Science, Imo State University, Owerri and University Health Services, Michael Okpara University of Agriculture, Umudike, Nigeria. Copyright © 2019 Dr. Obeagu Emmanuel Ifeanyi, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Received: 12 April 2019 Published: 30 April 2019 Keywords: Indispensable Programme; School Health Programme; Child Health Abstract This study deals with school health programme: an indispensable programme in child health. School health programme could be defined as initiation, maintenance and improvement of the health of school children and school personnel. The objectives of the study were discussed which include components of school health programme like health education, assessment of handicapped children and treatment of minor ailments. Common diseases that may occur among school children were discussed among which were dental disease, Gastroenteritis, scabies and worm infestation. The roles of health workers in school health programme were also analyzed. The relevance of school health programme in child health was highlighted in details. Therefore it is paramount that a healthy environment is required to provide children with the best opportunity to make appropriate adjustment during critical periods because the rapid physical and mental development that children undergo occurs during school age. -

The Sad and Tragic Life of Typhoid Mary
THE SAD AND TRAGIC LIFE OF TYPHOID MARY Janet Brooks six came down with the high and ex- 2: -.-! :.::.::...,: !.: .,!.! j!:..:.l.:.! ., 1 ,,; tended fever characteristic of typhoid. Before the arrival of antibiotics, the mortality rate was at least 10%. Typhoid fever was first identified early in the 19th century, but it wasn't until the 1880s that Salmonella typhi was isolated. The bacteria was spread mainly by contaminated drinking water, and the incidence of typhoid fever decreased as clean wa- ter became more widely available. Still, in 1900 the fever claimed the lives of 20 000 Americans, often striking groups of people in a single location even though the drinking water was known to be pure. A 11 Mary Mallon ever wanted to schools, jobs, the military, profes- When Long Island public-health be was a good plain cook. Yet sional basketball leagues and even officials failed to identify the cause of one wintry New York afternoon in crossing some national borders, it is the Oyster Bay outbreak, the owner 1907, she found herself bundled probably useful to re-examine the of the house, concerned that no one against her will into the back of a case of Typhoid Mary, as Mallon was would rent it again, hired sanitary city ambulance and, subdued only by soon labelled. Her case shows how engineer George Soper of New the weight of the female doctor sit- an earlier age resolved the conflict York's Department of Health to in- ting on top of her, removed from her that arises when society's right to vestigate. -
Presentation
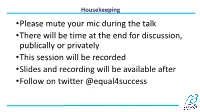
Housekeeping •Please mute your mic during the talk •There will be time at the end for discussion, publically or privately •This session will be recorded •Slides and recording will be available after •Follow on twitter @equal4success Queer scientists through history Elizabeth Wynn She/her 19/11/2020 The Great Geysers of California by Laura De Force Gordon If this little book should see the light after its 100 years of entombment, I would like its readers to know that the author was a lover of her own sex and devoted the best years of her life in striving for the political equality and social and moral elevation of women. Wouldn’t it be wonderful if all our letters could be published in the future in a more enlightened time. Then all the world could see how in love we are. Gordon Bowsher to Gilbert Bradley, 1940s James Barry • c. 1789 – 25 July 1865 • Irish surgeon • Qualified as a doctor in 1812 and joined the British army the following year • Served in many parts of the British Empire including South Africa, Jamaica, Malta and Canada where he promoted sanitation and nutritional reforms for troops and local residents • Performed one of the first recorded successful Caesarean sections outside of Europe James Barry • He was named Margaret Ann Bulkley at birth and was known as female in childhood • He changed his name before university and lived as a man for the rest of his life • Despite requesting “in the event of his death, strict precautions should be adopted to prevent any examination of his person”, the woman laying out the body described him as ‘a perfect female’ • The doctor who signed the death certificate wrote, “it was none of my business whether Dr Barry was a male or a female, and I thought she might be neither, viz. -

Fighting for Final Txt Crx.Indd
I*+,-./0+1-* The Lower East Side of New York was one of the most densely populated square miles on the face of the earth in the !"#$s. %e photo-essayist Jacob Riis famously described it as a world of bad smells, scooting rats, ash barrels, dead goats, and little boys drinking beer out of milk cartons. Six thousand people might be packed into a single city block, many in tenements with sanitary facilities so foul as to repel anyone who dared approach. City health inspectors called the neighborhood “the suicide ward”; one tenement was referred to—in an o&cial New York City Health Department report, no less—as an “out and out hog pen.”* Diarrhea epidemics blazed through the slums each summer, killing thousands of children every week. In the sweatshops of what was then known as “Jewtown,” children with smallpox and typhus dozed in heaps of garments destined for fashionable Broad- way shops. Desperate mothers paced the streets trying to soothe their feverish children, and white mourning cloths hung from every story of every building. A third of the children born in the slums died before their '(h birthday. In the European farming villages where many of these immi- grants came from, people spent most of their time outdoors in the fresh air and sunshine and seldom encountered more than a few hundred people in the course of lifetime. “Crowd diseases”— *Oscar Handlin, !e Uprooted: !e Epic Story of the Great Migrations !at Made the American People (University of Pennsylvania Press, )$$)). [ vii ] INTRODUCTION measles, dysentery, typhoid, diphtheria, trachoma, and so on— were rare, and the immigrants had little idea of how to prevent them. -

Tracking Down Typhoid Mary
GRAB & GO EXCERPTS TO WRITE ABOUT Fatal Fever: Tracking Down Typhoid Mary by Gail Jarrow Directions: Read the lead to the book and think about what the author’s argument is. What is the author’s purpose? What is her perspective? Highlight where you find clues to those questions and annotate your thinking. The Lead: Hidden “I am an innocent human being.” —Mary Mallon Early on a damp March morning in 1907, Mary Mallon answered the knock at the servants’ entrance of a New York brownstone house. She took one look at the visitors and lunged at them with her sharp fork. As they flinched, she ran toward the kitchen. Mary knew why they were there. A few weeks earlier, a well-dressed man with a mustache had shown up, accusing her of outrageous and horrible things. Later, he followed her. Cornered her at her friend’s home. Acted as though he had the right to stick her with a needle and steal her blood. Yesterday, a woman in a tailored suit and stiff collar had come to the kitchen. She claimed to have the authority to do exactly that . and more. The woman refused to take Mary’s “no” for an answer. Now she was back with the police. Mary was sure that this time, if they caught her, they wouldn’t let her go. She should have disappeared when she had the chance. They had no right to threaten her or touch her body. Even if she was only a cook, Mary wasn’t going to let them do it.