Hypokalemic Periodic Paralysis with Arrhythmia a Case Report and Review of Literature
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congenital Chloride Diarrhea in a Bartter Syndrome Misdiagnosed
Case Report iMedPub Journals Journal of Rare Disorders: Diagnosis & Therapy 2019 www.imedpub.com ISSN 2380-7245 Vol.5 No.2:4 DOI: 10.36648/2380-7245.5.2.196 Congenital Chloride Diarrhea in a Bartter Maria Helena Vaisbich*, Juliana Caires de Oliveira Syndrome Misdiagnosed Brazilian Patient Achili Ferreira, Ana Carola Hebbia Lobo Messa and Abstract Fernando Kok The differential diagnosis in children with hypokalemic hypochloremic alkalosis Department of Pediatric Nephrology, include a group of an inherited tubulopathies, such as Bartter Syndrome (BS) Instituto da Criança, University of São Paulo, and Gitelman Syndrome (GS). However, some of the clinically diagnosed São Paulo, Brasil patients present no pathogenic mutation in BS/GS known genes. Therefore, one can conclude that a similar clinical picture may be caused by PseudoBartter Syndrome (PBS) conditions. PBS include acquired renal problems (ex.: use of diuretics) as well as genetic or acquired extrarenal problems such as cystic *Corresponding author: fibrosis or cyclic vomiting, respectively. The accurate diagnosis of BS/GS needs Maria Helena Vaisbich a rational investigation. First step is to rule out PBS and confirm the primary renal tubular defect. However, it is not easy in some situations. In this sense, Department of Pediatric Nephrology, we reported a patient that was referred to our service with the diagnosis Instituto da Criança, University of São Paulo, of BS, but presented no mutation in BS/GS known genes. The whole-exome São Paulo, Brasil. sequencing detected a SCL26A3 likely pathogenic mutation leading to the final diagnosis of Congenital Chloride Diarrhea (CCD). Reviewing the records, the [email protected] authors noticed that liquid stools were mistaken for urine. -

Pseudo-Bartter Syndrome As the Initial Presentation of Cystic Fibrosis in Infants: a Paediatrics Section Paediatrics Series of Three Cases and Review of Literature
DOI: 10.7860/JCDR/2018/36189.11965 Case Series Pseudo-bartter Syndrome as the Initial Presentation of Cystic Fibrosis in Infants: A Paediatrics Section Paediatrics Series of Three cases and Review of Literature PRAWIN KUMAR1, NEERAJ GUPTA2, DAISY KHERA3, KULDEEP SINGH4 ABSTRACT Cystic Fibrosis (CF) is predominantly a disease of Caucasians, but it is increasingly being recognised in India. The typical presentations of CF are recurrent pneumonia and malabsorption. Atypical presentations are also increasingly being reported from India due to the differences in genotype and environmental factors. Pseudo-Bartter syndrome (PBS) is one of these atypical presentations which can present at any time after the diagnosis of CF but its presentation as an initial manifestation is rare. We hereby report three infants who presented with dehydration without obvious external losses. The investigations revealed metabolic alkalosis with hypochloraemia. A stepwise approach towards metabolic alkalosis revealed possibility of cystic fibrosis which was confirmed by sweat chloride test. All infants completely recovered with initial fluid and electrolyte therapy, following which supportive therapy for CF was started and subsequently they were discharged from the hospital. Keywords: Hypochloraemia, Metabolic alkalosis, Pseudo-Bartter Syndrome CASE SERIES sweat chloride test was not available at our centre so they were sent In this case series, we have described three infants in the age group to paediatric pulmonology division, AIIMS, New Delhi where sweat of 5-10 months from western Rajasthan, India, who presented with chloride test was performed (pilocarpine iontophoresis method), features of dehydration, without any evidence of obvious external which turned out to be positive (sweat chloride >60 mEq/L) in all fluid loss. -

Hypokalemic Periodic Paralysis - an Owner's Manual
Hypokalemic periodic paralysis - an owner's manual Michael M. Segal MD PhD1, Karin Jurkat-Rott MD PhD2, Jacob Levitt MD3, Frank Lehmann-Horn MD PhD2 1 SimulConsult Inc., USA 2 University of Ulm, Germany 3 Mt. Sinai Medical Center, New York, USA 5 June 2009 This article focuses on questions that arise about diagnosis and treatment for people with hypokalemic periodic paralysis. We will focus on the familial form of hypokalemic periodic paralysis that is due to mutations in one of various genes for ion channels. We will only briefly mention other �secondary� forms such as those due to hormone abnormalities or due to kidney disorders that result in chronically low potassium levels in the blood. One can be the only one in a family known to have familial hypokalemic periodic paralysis if there has been a new mutation or if others in the family are not aware of their illness. For more general background about hypokalemic periodic paralysis, a variety of descriptions of the disease are available, aimed at physicians or patients. Diagnosis What tests are used to diagnose hypokalemic periodic paralysis? The best tests to diagnose hypokalemic periodic paralysis are measuring the blood potassium level during an attack of paralysis and checking for known gene mutations. Other tests sometimes used in diagnosing periodic paralysis patients are the Compound Muscle Action Potential (CMAP) and Exercise EMG; further details are here. The most definitive way to make the diagnosis is to identify one of the calcium channel gene mutations or sodium channel gene mutations known to cause the disease. However, known mutations are found in only 70% of people with hypokalemic periodic paralysis (60% have known calcium channel mutations and 10% have known sodium channel mutations). -

Inherited Renal Tubulopathies—Challenges and Controversies
G C A T T A C G G C A T genes Review Inherited Renal Tubulopathies—Challenges and Controversies Daniela Iancu 1,* and Emma Ashton 2 1 UCL-Centre for Nephrology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF, UK 2 Rare & Inherited Disease Laboratory, London North Genomic Laboratory Hub, Great Ormond Street Hospital for Children National Health Service Foundation Trust, Levels 4-6 Barclay House 37, Queen Square, London WC1N 3BH, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-2381204172; Fax: +44-020-74726476 Received: 11 February 2020; Accepted: 29 February 2020; Published: 5 March 2020 Abstract: Electrolyte homeostasis is maintained by the kidney through a complex transport function mostly performed by specialized proteins distributed along the renal tubules. Pathogenic variants in the genes encoding these proteins impair this function and have consequences on the whole organism. Establishing a genetic diagnosis in patients with renal tubular dysfunction is a challenging task given the genetic and phenotypic heterogeneity, functional characteristics of the genes involved and the number of yet unknown causes. Part of these difficulties can be overcome by gathering large patient cohorts and applying high-throughput sequencing techniques combined with experimental work to prove functional impact. This approach has led to the identification of a number of genes but also generated controversies about proper interpretation of variants. In this article, we will highlight these challenges and controversies. Keywords: inherited tubulopathies; next generation sequencing; genetic heterogeneity; variant classification. 1. Introduction Mutations in genes that encode transporter proteins in the renal tubule alter kidney capacity to maintain homeostasis and cause diseases recognized under the generic name of inherited tubulopathies. -

Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -
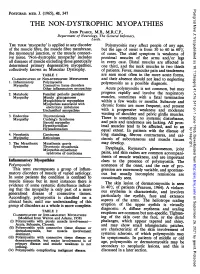
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Periodic Paralysis
Periodic Paralysis In Focus Dear Readers Fast Facts This “In Focus” report is the third in a series of MDA’s three-year commitment for all Hypokalemic periodic paralysis MDA comprehensive reports about the latest in periodic paralysis research as of March Hypokalemic PP can begin anywhere from neuromuscular disease research and manage- 2009 is $1,938,367. The Association’s early childhood to the 30s, with periodic ment. allocation for research on hyperkalemic attacks of severe weakness lasting hours This report focuses on the periodic and hypokalemic periodic paralysis to days. The frequency of attacks gener- paralyses, a group of disorders that result from research since 1950 is $8,125,341. ally lessens in the 40s or 50s. Permanent malfunctions in so-called ion channels, micro- MDA’s allocation for the recently weakness may persist between attacks, scopic tunnels that make possible high-speed identified Andersen-Tawil syndrome usually beginning in middle age and pro- movement of electrically charged particles is $515,430 since 2001. MDA is cur- gressing slowly over years. across barriers inside cells and between cells rently funding 11 grants in the periodic The most common underlying cause and their surroundings. paralyses. is any of several genetic mutations in When ion channels fail to open or close The periodic paralyses are gener- a gene on chromosome 1 that carries according to an exquisitely fine-tuned program, ally divided into hyperkalemic periodic instructions for a calcium channel protein episodes of paralysis of the skeletal muscles paralysis, hypokalemic periodic paralysis in skeletal muscle fibers. When this chan- and even temporary irregularities in the heart- and Andersen-Tawil syndrome. -

Facilitations and Hurdles of Genetic Testing in Neuromuscular Disorders
diagnostics Review Facilitations and Hurdles of Genetic Testing in Neuromuscular Disorders Andrea Barp 1,*, Lorena Mosca 2 and Valeria Ada Sansone 1 1 The NEMO Clinical Center in Milan, Neurorehabilitation Unit, University of Milan, Piazza Ospedale Maggiore 3, 20162 Milano, Italy; [email protected] 2 Medical Genetics Unit, ASST Grande Ospedale Metropolitano Niguarda, Piazza Ospedale Maggiore 3, 20162 Milano, Italy; [email protected] * Correspondence: [email protected] Abstract: Neuromuscular disorders (NMDs) comprise a heterogeneous group of disorders that affect about one in every thousand individuals worldwide. The vast majority of NMDs has a genetic cause, with about 600 genes already identified. Application of genetic testing in NMDs can be useful for several reasons: correct diagnostic definition of a proband, extensive familial counselling to identify subjects at risk, and prenatal diagnosis to prevent the recurrence of the disease; furthermore, identification of specific genetic mutations still remains mandatory in some cases for clinical trial enrollment where new gene therapies are now approaching. Even though genetic analysis is catching on in the neuromuscular field, pitfalls and hurdles still remain and they should be taken into account by clinicians, as for example the use of next generation sequencing (NGS) where many single nucleotide variants of “unknown significance” can emerge, complicating the correct interpretation of genotype-phenotype relationship. Finally, when all efforts in terms of molecular analysis have been carried on, a portion of patients affected by NMDs still remain “not genetically defined”. In the present review we analyze the evolution of genetic techniques, from Sanger sequencing to NGS, and we discuss “facilitations and hurdles” of genetic testing which must always be balanced by clinicians, Citation: Barp, A.; Mosca, L.; in order to ensure a correct diagnostic definition, but taking always into account the benefit that the Sansone, V.A. -

Identification of Gene Mutations in Patients with Primary Periodic
Luo et al. BMC Neurology (2019) 19:92 https://doi.org/10.1186/s12883-019-1322-6 RESEARCH ARTICLE Open Access Identification of gene mutations in patients with primary periodic paralysis using targeted next-generation sequencing Sushan Luo1†, Minjie Xu2†, Jian Sun1, Kai Qiao3, Jie Song1, Shuang Cai1, Wenhua Zhu1, Lei Zhou1, Jianying Xi1, Jiahong Lu1, Xiaohua Ni2, Tonghai Dou4 and Chongbo Zhao1,5* Abstract Background: Primary periodic paralysis is characterized by recurrent quadriplegia typically associated with abnormal serum potassium levels. The molecular diagnosis of primary PP previously based on Sanger sequencing of hot spots or exon-by-exon screening of the reported genes. Methods: We developed a gene panel that includes 10 ion channel-related genes and 245 muscular dystrophy- and myopathy-related genes and used this panel to diagnose 60 patients with primary periodic paralysis and identify the disease-causing or risk-associated gene mutations. Results: Mutations of 5 genes were discovered in 39 patients (65.0%). SCN4A, KCNJ2 and CACNA1S variants accounted for 92.5% of the patients with a genetic diagnosis. Conclusions: Targeted next-generation sequencing offers a cost-effective approach to expand the genotypes of primary periodic paralysis. A clearer genetic profile enables the prevention of paralysis attacks, avoidance of triggers and the monitoring of complications. Keywords: Primary periodic paralysis, Targeted next-generation sequencing, Gene panel, Gene mutation distribution, Calcium homeostasis. Background (SCN4A) and potassium voltage-gated channel subfamily Periodic paralysis (PP) is characterized by episodes of J member 2 (KCNJ2), that encode voltage-gated chan- muscle weakness that occur at irregular intervals due to nels in muscle membranes that generate or sustain skeletal muscle ion channelopathies. -

Cerebral Hypotonia by Mihee Bay MD (Dr
Cerebral hypotonia By Mihee Bay MD (Dr. Bay of Kennedy Krieger Institute and Johns Hopkins School of Medicine has no relevant financial relationships to disclose.) Originally released July 12, 2006; last updated February 1, 2016; expires February 1, 2019 Introduction This article includes discussion of cerebral hypotonia, central hypotonia, essential hypotonia, benign congenital hypotonia, and floppy infant. The foregoing terms may include synonyms, similar disorders, variations in usage, and abbreviations. Overview Hypotonia is a clinical manifestation of numerous diseases affecting the central and/or peripheral motor nervous system. The key to accurate diagnosis involves integral steps of evaluation that include a detailed history, examination, and diagnostic tests. “Cerebral” (or central) hypotonia implies pathogenesis from abnormalities from the central nervous system, and related causal disorders include cerebral dysgenesis and genetic or metabolic disorders. Patients with central hypotonia generally have hypotonia without associated weakness, in contrast to the peripheral (lower motor neuron) causes, which typically produce both hypotonia and muscle weakness. Hypotonia is a clinical manifestation of over 500 genetic disorders; thus, a logical, stepwise approach to diagnosis is essential. With recent advances in the field of genetic testing, diagnostic yield will undoubtedly improve. There is no cure, but treatment includes supportive therapies, such as physical and occupational therapy, and diagnosis-specific management. Key points • Hypotonia is reduced tension or resistance of passive range of motion. • The first step in the evaluation of a child with hypotonia is localization to the central (“cerebral”) or peripheral nervous system, or both. • Central hypotonia is more likely to be noted axially with normal strength and hyperactive to normal deep tendon reflexes. -

The Role of Potassium Recirculation in Cochlear Amplification
The role of potassium recirculation in cochlear amplification Pavel Mistrika and Jonathan Ashmorea,b aUCL Ear Institute and bDepartment of Neuroscience, Purpose of review Physiology and Pharmacology, UCL, London, UK Normal cochlear function depends on maintaining the correct ionic environment for the Correspondence to Jonathan Ashmore, Department of sensory hair cells. Here we review recent literature on the cellular distribution of Neuroscience, Physiology and Pharmacology, UCL, Gower Street, London WC1E 6BT, UK potassium transport-related molecules in the cochlea. Tel: +44 20 7679 8937; fax: +44 20 7679 8990; Recent findings e-mail: [email protected] Transgenic animal models have identified novel molecules essential for normal hearing Current Opinion in Otolaryngology & Head and and support the idea that potassium is recycled in the cochlea. The findings indicate that Neck Surgery 2009, 17:394–399 extracellular potassium released by outer hair cells into the space of Nuel is taken up by supporting cells, that the gap junction system in the organ of Corti is involved in potassium handling in the cochlea, that the gap junction system in stria vascularis is essential for the generation of the endocochlear potential, and that computational models can assist in the interpretation of the systems biology of hearing and integrate the molecular, electrical, and mechanical networks of the cochlear partition. Such models suggest that outer hair cell electromotility can amplify over a much broader frequency range than expected from isolated cell studies. Summary These new findings clarify the role of endolymphatic potassium in normal cochlear function. They also help current understanding of the mechanisms of certain forms of hereditary hearing loss. -

Date: 1/9/2017 Question: Botulism Is an Uncommon Disorder Caused By
6728 Old McLean Village Drive, McLean, VA 22101 Tel: 571.488.6000 Fax: 703.556.8729 www.clintox.org Date: 1/9/2017 Question: Botulism is an uncommon disorder caused by toxins produced by Clostridium botulinum. Seven subtypes of botulinum toxin exist (subtypes A, B, C, D, E, F and G). Which subtypes have been noted to cause human disease and which ones have been reported to cause infant botulism specifically in the United States? Answer: According to the cited reference “Only subtypes A, B, E and F cause disease in humans, and almost all cases of infant botulism in the United States are caused by subtypes A and B. Botulinum-like toxins E and F are produced by Clostridium baratii and Clostridium butyricum and are only rarely implicated in infant botulism” (Rosow RK and Strober JB. Infant botulism: Review and clinical update. 2015 Pediatr Neurol 52: 487-492) Date: 1/10/2017 Question: A variety of clinical forms of botulism have been recognized. These include wound botulism, food borne botulism, and infant botulism. What is the most common form of botulism reported in the United States? Answer: According to the cited reference, “In the United States, infant botulism is by far the most common form [of botulism], constituting approximately 65% of reported botulism cases per year. Outside the United States, infant botulism is less common.” (Rosow RK and Strober JB. Infant botulism: Review and clinical update. 2015 Pediatr Neurol 52: 487-492) Date: 1/11/2017 Question: Which foodborne pathogen accounts for approximately 20 percent of bacterial meningitis in individuals older than 60 years of age and has been associated with unpasteurized milk and soft cheese ingestion? Answer: According to the cited reference, “Listeria monocytogenes, a gram-positive rod, is a foodborne pathogen with a tropism for the central nervous system.