Osteoarthritis of the Hand and Wrist Information Booklet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Study on the Absence of Palmaris Longus in a Multi-Racial Population
108472 NV-OA7 pg26-28.qxd 11/05/2007 05:02 PM Page 26 (Black plate) Malaysian Orthopaedic Journal 2007 Vol 1 No 1 SA Roohi, etal A Study on the Absence of Palmaris Longus in a Multi- racial Population SA Roohi, MS (Ortho) (UKM), L Choon-Sian, MD (UKM), A Shalimar, MS (Ortho) (UKM), GH Tan, MS (Ortho) (UKM), AS Naicker, M Med Rehab (UM) Hospital Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia ABSTRACT Most standard textbooks of hand surgery quote the prevalence of absence of palmaris longus at around 15%3-5. Palmaris longus is a dispensable muscle with a long tendon However, this figure varies considerably in different ethnic which is very useful in reconstructive surgery. It is absent groups. A study by Thompson et al6 on 300 Caucasian 2.8 to 24% of the population depending on the race/ethnicity subjects found that palmaris longus was absent unilaterally in studied. Four hundred and fifty healthy subjects (equally 16%, and bilaterally in 9% of the study sample for an overall distributed among Malaysia’s 3 major ethnic groups) were prevalence of absence of 24%. Similarly, George7 noted on clinically examined for the presence or absence of palmaris 276 cadavers of European descent that its absence was 13% longus. This tendon was found to be absent unilaterally in unilaterally, 8.7% bilaterally for an overall absence of 15.2%. 6.4% of study subjects, and bilaterally in 2.9% of study Another cadaveric study by Vanderhooft8 in Seattle, USA participants. Malays have a high prevalence of palmaris reported its overall absence to be 12%. -

Wrist Fracture – Advice Following Removal of Your Cast
Wrist Fracture – advice following removal of your cast A plaster cast usually prevents a fracture from moving, but allows your fingers to move. The cast also reduces pain. What to expect It usually takes four to six weeks for new bone to form to heal your fracture. When the cast is removed most people find that their wrist is stiff, weak and uncomfortable to start with. It may also be prone to swelling and the skin dry or flaky, this is quite normal. It is normal to get some pain after your fracture. If you need painkillers you should take them as prescribed as this will allow you to do your exercises and use your wrist for light activities. You can ask a Pharmacist about over the counter painkillers. If your pain is severe, continuous or excessive you should contact your GP. The new bone gradually matures and becomes stronger over the next few months. It is likely to be tender and may hurt if you bang it. The muscles will be weak initially, but they should gradually build up as you start to use your hand and wrist. When can I start to use my hand and wrist? It is important to try and use your hand and wrist as normally as possible. Start with light activities like fastening buttons, washing your face, eating, turning the pages of books over etc. Build up as pain allows. Avoid lifting a kettle for 4 weeks If I have been given a Wrist splint You may have been given a wrist splint to wear. -

Complex Regional Pain Syndrome Type I (Shoulder-Hand Syndrome) in an Elderly Patient After Open Cardiac Surgical Intervention; a Case Report
Eastern Journal of Medicine 16 (2011) 56-58 L. Ediz et al / CRPS type I after open cardiac Surgery Case Report Complex regional pain syndrome type I (shoulder-hand syndrome) in an elderly patient after open cardiac surgical intervention; a case report Levent Ediza*, Mehmet Fethi Ceylanb , Özcan Hıza, İbrahim Tekeoğlu c a Department of Physical Medicine and Rehabilitation, Yüzüncü Yıl University Medical Faculty, Van, Turkey b Department of Orthopaedics and Traumatology,Yüzüncü Yıl University Medical Faculty, Van, Turkey c Department of Rheumatology, Yüzüncü Yıl University Medical Faculty, Van, Turkey Abstract. We described the first case report in the literature who developed Complex Regional Pain Syndrome (CRPS type I) symptoms in his right shoulder and right hand within 15 days after open cardiac surgery and discussed shoulder-hand syndrome (CRPS type I) and frozen shoulder diagnosis along with the reasons of no report of CRPS type I in these patients. We also speculated whether frozen shoulder seen in postthoracotomy and postcardiac surgery patients might be CRPS type I in fact. Key words: Complex regional pain syndrome, cardiac surgery, frozen shoulder 1. Introduction Improper patient positioning, muscle division, perioperative nerve injury, rib spreading, and Complex Regional Pain Syndrome (CRPS) is consequent postoperative pain influence the complication of injuries which is seen at the patient's postoperative shoulder function and distal end of the affected area characterized by quality of life (5). In a study Tuten HR et al pain, allodyni, hyperalgesia, edema, abnormal retrospectively evaluated for the incidence of vasomotor and sudomotor activity, movement adhesive capsulitis of the shoulder of two disorders, joint stiffness, regional osteopenia, and hundred fourteen consecutive male cardiac dystrophic changes in soft tissue (1,2). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

PE1897 Wrist and Hand Stretches
Patient and Family Education Wrist and Hand Stretches How can I help my child do the stretches? Use these exercises to help stretch the You play an important role in your child’s therapy. Older children may need wrist and hand. reminders to do their stretches every day. You may need to help position your younger child for the stretches. Or you may need to help stretch your child’s hand or arm. Be sure to pay attention to your child’s alignment and posture to make sure each stretch is performed correctly. How often should my child do the stretches? These stretches should be done twice a day, or as instructed by your therapist: ______________________________________________________________ Stretches Wrist extension Hold arm out in front Use opposite hand to bend wrist up with fingers straight Option to straighten elbow for increased stretch Hold for 30 seconds or _______ Repeat 2 times or ___________ VHI Wrist extension Sit with elbows on table Place palms together Slowly lower wrists to table Hold for 30 seconds or ______ Repeat 2 times or __________ VHI Wrist flexion Hold arm out in front Use opposite hand to bend wrist down Option to straighten elbow for increased stretch Option to curl fingers for increased stretch Hold for 30 seconds or ______ VHI Repeat 2 times or __________ 1 of 2 Wrist and Hand Stretches Wrist radial/ulnar deviation To Learn More Hold arm at side of body with palm • Occupational/Physical facing forward Therapy 206-987-2113 Use opposite hand to straighten wrist toward the thumb side Do not allow the wrist to flex forward to extend backward Free Interpreter Hold for 30 seconds or ______ Services Repeat 2 times or __________ • In the hospital, ask BioEx Systems Inc.* your child’s nurse. -

Hand, Elbow, Wrist Pain
Physical and Sports Therapy Hand, Elbow, Wrist Pain The hand is a wondrously complex structure of tiny bones, muscles, ligaments, and tendons which work together to perform tasks. The wrist and elbow are stabilizing joints that support the steady use of the hand and provide attachment points for the muscles that control the hand and wrist. All three of these areas are prone to injury from overuse or trauma. Their complexity requires the skills of an expert for proper rehabilitation from injury. Some Hand, Wrist, and Elbow Issues Include: Tennis/Golfer’s Elbow: Tendonitis, or inflammation of the tendons, at the muscular attachments near the elbow. Symptoms typically include tenderness on the sides of the elbow, which increase with use of the wrist and hand, such as shaking hands or picking up a gallon of milk. Tendonitis responds well to therapy, using eccentric exercise, stretching, and various manual therapy techniques. Carpal Tunnel Syndrome: Compression of the Median Nerve at the hand/base of your wrist. Symptoms include pain, numbness, and tingling of the first three fingers. The condition is well-known for waking people at night. Research supports the use of therapy, particularly in the early phase, for alleviation of the compression through stretching and activity modification. Research indicates that the longer symptoms are present before initiating treatment, the worse the outcome for therapy and surgical intervention due to underlying physiological changes of the nerve. What can Physical or Occupational therapy do for Hand, Wrist, or Elbow pain? Hand, wrist, and elbow injuries are commonly caused by trauma, such as a fall or overuse. -

REVIEW ARTICLE Osteoarthritis of the Wrist
REVIEW ARTICLE Osteoarthritis of the Wrist Krista E. Weiss, Craig M. Rodner, MD From Harvard College, Cambridge, MA and Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Osteoarthritis of the wrist is one of the most common conditions encountered by hand surgeons. It may result from a nonunited or malunited fracture of the scaphoid or distal radius; disruption of the intercarpal, radiocarpal, radioulnar, or ulnocarpal ligaments; avascular necrosis of the carpus; or a developmental abnormality. Whatever the cause, subsequent abnormal joint loading produces a spectrum of symptoms, from mild swelling to considerable pain and limitations of motion as the involved joints degenerate. A meticulous clinical and radiographic evaluation is required so that the pain-generating articulation(s) can be identi- fied and eliminated. This article reviews common causes of wrist osteoarthritis and their surgical treatment alternatives. (J Hand Surg 2007;32A:725–746. Copyright © 2007 by the American Society for Surgery of the Hand.) Key words: Wrist, osteoarthritis, arthrodesis, carpectomy, SLAC. here are several different causes, both idio- of events is analogous to SLAC wrist and has pathic and traumatic, of wrist osteoarthritis. been termed scaphoid nonunion advanced collapse Untreated cases of idiopathic carpal avascular (SNAC). Wrist osteoarthritis can also occur second- T 1 2 necrosis, as in Kienböck’s or Preiser’s disease, may ary to an intra-articular fracture of the distal radius or result in radiocarpal arthritis. Congenital wrist abnor- ulna or from an extra-articular fracture resulting in malities, such as Madelung’s deformity,3,4 can lead malunion and abnormal joint loading. -

Wrist and Hand Examina[On
Wrist and Hand Examinaon Daniel Lueders, MD Assistant Professor Physical Medicine and Rehabilitaon Objecves • Understand the osseous, ligamentous, tendinous, and neural anatomy of the wrist and hand • Outline palpable superficial landmarks in the wrist and hand • Outline evaluaon of and differen.aon between nerves to the wrist and hand • Describe special tes.ng of wrist and hand Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Inspec.on • Ecchymosis • Erythema • Deformity • Laceraon Inspec.on • Common Finger Deformies • Swan Neck Deformity • Boutonniere Deformity • Hypertrophic nodules • Heberden’s, Bouchard’s Inspec.on • Swan Neck Deformity • PIP hyperextension, DIP flexion • Pathology is at PIP joint • Insufficiency of volar/palmar plate and suppor.ng structures • Distally, the FDP tendon .ghtens from PIP extension causing secondary DIP flexion • Alternavely, extensor tendon rupture produces similar deformity Inspec.on • Boutonniere Deformity • PIP flexion, DIP hyperextension • Pathology is at PIP joint • Commonly occurs from insufficiency of dorsal and lateral suppor.ng structures at PIP joint • Lateral bands migrate volar/palmar, creang increased flexion moment • Results in PIP “buTon hole” effect dorsally Inspec.on • Nodules • Osteoarthri.c • Hypertrophic changes of OA • PIP - Bouchard’s nodule • DIP - Heberden’s nodule • Rheumatoid Arthri.s • MCP joints affected most • Distal radioulnar joint can also be affected -

Readingsample
Color Atlas of Human Anatomy Vol. 1: Locomotor System Bearbeitet von Werner Platzer 6. durchges. Auflage 2008. Buch. ca. 480 S. ISBN 978 3 13 533306 9 Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 130 Upper Limb: Bones, Ligaments, Joints Radiocarpal and Midcarpal Joints Ligaments in the Region of the Wrist (A–E) (A–E) Four groups of ligaments can be distin- The radiocarpal or wrist joint is an ellip- guished: soid joint formed on one side by the radius (1) and the articular disk (2) and on the Ligaments which unite the forearm bones with other by the proximal row of carpal bones.Not the carpal bones (violet). These include the all the carpal bones of the proximal row are ulnar collateral ligament (8), the radial col- in continual contact with the socket- lateral ligament (9), the palmar radiocarpal shaped articular facet of the radius and the ligament (10), the dorsal radiocarpal liga- disk. The triquetrum (3), only makes close ment (11), and the palmar ulnocarpal liga- contact with the disk during ulnar abduc- ment (12). tion and loses contact on radial abduction. Ligaments which unite the carpal bones with The capsule of the wrist joint is lax, dorsally one another,orintercarpal ligaments (red). These comprise the radiate carpal ligament Upper Limb relatively thin, and is reinforced by numer- ous ligaments. -

Musculoskeletal Ultrasound Technical Guidelines III. Wrist
European Society of MusculoSkeletal Radiology Musculoskeletal Ultrasound Technical Guidelines III. Wrist Ian Beggs, UK Stefano Bianchi, Switzerland Angel Bueno, Spain Michel Cohen, France Michel Court-Payen, Denmark Andrew Grainger, UK Franz Kainberger, Austria Andrea Klauser, Austria Carlo Martinoli, Italy Eugene McNally, UK Philip J. O’Connor, UK Philippe Peetrons, Belgium Monique Reijnierse, The Netherlands Philipp Remplik, Germany Enzo Silvestri, Italy Wrist Note The standard US examination of the wrist begins with evaluation of its dorsal aspect, followed by the palmar one. Depending on the specific clinical presentation, US images can be obtained in different position of the wrist (flexion and extension, radial and ulnar deviation, pronation and supination), with the patient seated in front of the examiner. 1 DORSAL WRIST: compartments of extensor tendons Place the transducer on a transverse plane over the dorsal aspect of the wrist to allow proper identification of the extensor tendons. In general, one should first recognize a given tendon and then follow it on short-axis planes down to the distal insertion. Long- axis US images of the extensor tendons are less useful: they may help to evaluate the integrity of tendons and assess their dynamic motion in detail. Dynamic scanning of the extensor tendons can be performed by placing the hand on a gel tube with the fingers hanging outside its edge to allow easy fingers movements. Legend: APL, abductor pollicis longus; EPB, extensor pollicis brevis; ECRL, extensor carpi radialis longus; EPCB, extensor carpi radialis brevis; EPL, extensor pollicis longus; EIP, extensor indicis proprius; EDC, extensor digitorum longus; EDQ, extensor digiti quinti proprius; ECU, extensor carpi ulnaris 2 first compartment Keeping the patient’s wrist halfway between pronation and supination, place the probe over the lateral aspect of the radial styloid to examine the first compartment of the extensor tendons - abductor pollicis longus (ventral) and extensor pollicis brevis (dorsal). -
Stretching and Positioning Regime for Upper Limb
Information for patients and visitors Stretching and Positioning Regime for Upper Limb Physiotherapy Department This leaflet has been designed to remind you of the exercises you Community & Therapy Services have been taught, the correct techniques and who to contact with any queries. For more information about our Trust and the services we provide please visit our website: www.nlg.nhs.uk Information for patients and visitors Muscle Tone Muscle tone is an unconscious low level contraction of your muscles while they are at rest. The purpose of this is to keep your muscles primed and ready to generate movement. Several neurological causes may change a person’s muscle tone to increase or decrease resulting in a lack of movement. Over time, a lack of movement can cause stiffness, pain, and spasticity. In severe cases this may also lead to contractures. Spasticity Spasticity can be defined as a tightening or stiffness of the muscle due to increased muscle tone. It can interfere with normal functioning. It can also greatly increase fatigue. However, exercise, properly done, is vital in managing spasticity. The following tips may prove helpful: • Avoid positions that make the spasticity worse • Daily stretching of muscles to their full length will help to manage the tightness of spasticity, and allow for optimal movement • Moving a tight muscle to a new position may result in an increase in spasticity. If this happens, allow a few minutes for the muscles to relax • When exercising, try to keep head straight • Sudden changes in spasticity may -
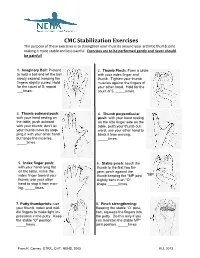
CMC Stabilization Exercises the Purpose of These Exercises Is to Strengthen Your Muscles Around Your Arthritic Thumb Joint Making It More Stable and Less Painful
CMC Stabilization Exercises The purpose of these exercises is to strengthen your muscles around your arthritic thumb joint making it more stable and less painful. Exercises are to be performed gently and never should be painful! 1. Imaginary Ball: Pretend 2. Thumb Pinch: Form a circle to hold a ball and let the ball with your index finger and slowly expand, keeping the thumb. Tighten your thumb fingers slightly curled. Hold muscles against the fingers of for the count of 5, repeat your other hand. Hold for the ___times. count of 5, _____times. 3. Thumb outward push: 4. Thumb perpendicular with your hand resting on push: with your hand resting the table, push outward on the little finger side on the with your thumb; don’t let table, push your thumb out- your thumb move by stop- ward; use your other hand to ping it with your other hand block it from moving. but tense the muscles. _____times. _____times. 5. Index finger push: 6. Stable pinch: touch the with your hand lying flat thumb to the first two fin- on the table, move the gers; pinch against the index finger toward your thumb keeping the *MP joint *MP thumb; use your other slightly bent in an “O” hand to stop it from mov- shape. _____times. ing. _____times. 7. Putty thumbprints: use 8. Pinch strengthening: your thumb, index and mid- Keeping the stable “O” posi- dle fingers to make light im- tion, squeeze the fingers into pressions in the putty. Keep the putty. Do this only if you the stable “O” position.