Overview of Neo-Vascular Lesions After Delivery Or Miscarriage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
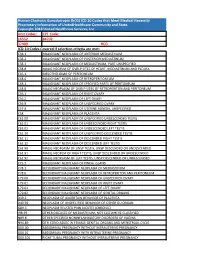
Human Chorionic Gonadotropin (Hcg) ICD 10 Codes That Meet Medical Necessity Proprietary Information of Unitedhealthcare Community and State
Human Chorionic Gonadotropin (hCG) ICD 10 Codes that Meet Medical Necessity Proprietary Information of UnitedHealthcare Community and State. Copyright 2018 United Healthcare Services, Inc Unit Codes: CPT Code: 16552 84702 37409 HCG ICD-10 Codes Covered if selection criteria are met: C38.1 MALIGNANT NEOPLASM OF ANTERIOR MEDIASTINUM C38.2 MALIGNANT NEOPLASM OF POSTERIOR MEDIASTINUM C38.3 MALIGNANT NEOPLASM OF MEDIASTINUM, PART UNSPECIFIED C38.8 MALIG NEOPLM OF OVRLP SITES OF HEART, MEDIASTINUM AND PLEURA C45.1 MESOTHELIOMA OF PERITONEUM C48.0 MALIGNANT NEOPLASM OF RETROPERITONEUM C48.1 MALIGNANT NEOPLASM OF SPECIFIED PARTS OF PERITONEUM C48.8 MALIG NEOPLASM OF OVRLP SITES OF RETROPERITON AND PERITONEUM C56.1 MALIGNANT NEOPLASM OF RIGHT OVARY C56.2 MALIGNANT NEOPLASM OF LEFT OVARY C56.9 MALIGNANT NEOPLASM OF UNSPECIFIED OVARY C57.4 MALIGNANT NEOPLASM OF UTERINE ADNEXA, UNSPECIFIED C58 MALIGNANT NEOPLASM OF PLACENTA C62.00 MALIGNANT NEOPLASM OF UNSPECIFIED UNDESCENDED TESTIS C62.01 MALIGNANT NEOPLASM OF UNDESCENDED RIGHT TESTIS C62.02 MALIGNANT NEOPLASM OF UNDESCENDED LEFT TESTIS C62.10 MALIGNANT NEOPLASM OF UNSPECIFIED DESCENDED TESTIS C62.11 MALIGNANT NEOPLASM OF DESCENDED RIGHT TESTIS C62.12 MALIGNANT NEOPLASM OF DESCENDED LEFT TESTIS C62.90 MALIG NEOPLASM OF UNSP TESTIS, UNSP DESCENDED OR UNDESCENDED C62.91 MALIG NEOPLM OF RIGHT TESTIS, UNSP DESCENDED OR UNDESCENDED C62.92 MALIG NEOPLASM OF LEFT TESTIS, UNSP DESCENDED OR UNDESCENDED C75.3 MALIGNANT NEOPLASM OF PINEAL GLAND C78.1 SECONDARY MALIGNANT NEOPLASM OF MEDIASTINUM C78.6 SECONDARY -

Histomorphological Study of Chorionic Villi in Products of Conception Following First Trimester Abortions
November, 2018/ Vol 4/ Issue 7 Print ISSN: 2456-9887, Online ISSN: 2456-1487 Original Research Article Histomorphological study of chorionic villi in products of conception following first trimester abortions Shilpa MD1, Supreetha MS2, Varshashree3 1Dr. Shilpa, MD, Assistant Professor, 2Dr. Supreetha, MS, Assistant Professor, 3Dr. Varshashree, Post graduate, all authors are affiliated with Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Corresponding Author: Dr. Shilpa, MD, Assistant Professor, Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Email id: [email protected] ………………………………………………………………………………………………………………………………... Abstract Background: The common problem which occurs in first trimester of pregnancy is miscarriage. Retained products of conception are commonly received specimen for histopathological examination. Apart from confirmation of pregnancy, a careful examination can provide some additional information about the cause or the conditions associated with abortion. Aim: 1. To study various histopathological changes occurring in chorionic villi in first trimester spontaneous abortions and to know the pathogenesis of abortions. Materials and methods: This was a cross sectional retrospective study carried out for over a period of 3 years from January 2015 to January 2018. A total of 235biopsies were obtained from patient with the diagnosis of the first trimester spontaneous abortions were included in this study. Results: In our study most common age group of the abortion was between 21-30 years (63%). Incomplete abortion was the commonest type of abortion (47.7%). Many dysmorphic features were observed in this study like hydropic change (67%), stromal fibrosis (62%), villi with reduced blood vessels (52.7%) and perivillous fibrin deposition. -

Medical Abortion Reference Guide INDUCED ABORTION and POSTABORTION CARE at OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas
Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas ISBN: 1-933095-97-0 Citation: Edelman, A. & Mark, A. (2018). Medical Abortion Reference Guide: Induced abortion and postabortion care at or after 13 weeks gestation (‘second trimester’). Chapel Hill, NC: Ipas. Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. We believe in a world where every woman and girl has the right and ability to determine her own sexuality and reproductive health. Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1-919-967-7052 [email protected] www.ipas.org Cover photo: © Ipas The photographs used in this publication are for illustrative purposes only; they do not imply any particular attitudes, behaviors, or actions on the part of any person who appears in the photographs. Printed on recycled paper. Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) Alison Edelman Senior Clinical Consultant, Ipas Professor, OB/GYN Oregon Health & Science University Alice Mark Associate Medical Director National Abortion Federation About Ipas Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. -

Miscarriage Or Early Pregnancy Loss- Diagnosis and Management (Version 5)
Miscarriage or early pregnancy loss- diagnosis and management (Version 5) Guideline Readership This guideline applies to all women diagnosed with miscarriage in early pregnancy (up to 13 completed weeks) within the Heart of England Foundation Trust and to attending clinicians, sonographers and nursing staff on Gynaecology ward and early pregnancy unit. All care is tailored to individual patient needs, with an in-depth discussion of the intended risks and benefits for any intervention offered to woman with early pregnancy loss. Guideline Objectives The objective of this guideline is to enable all clinicians to recognise the different types of miscarriages and to follow a recognised management pathway so that all women with actual or suspected miscarriage receive, an appropriate and individualised care. Other Guidance Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guidance Dec 2012 Ratified Date: Insert Date Launch Date: 16 March 2018 Review Date: 16 March 2021 Guideline Author: Dr Rajmohan, Dr Cheema Contents & page numbers: 1. Flowcharts Flowchart 1 – Management of complete miscarriage p3 Flowchart 2 – Management of incomplete miscarriage p4 Flowchart 3 – Management of Missed miscarriage p5 Flowchart 4 - Management of Early fetal demise p6 Flowchart 5 – Medical management of miscarriage p7 Flowchart 6 - Surgical management (SMM) pathway p8 2. Executive summary and Overview p9 3. Body of guideline Types of miscarriage p9 Threatened miscarriage p9 Complete miscarriage p9 Incomplete miscarriage p9 Missed miscarriage -

Ectopic Pregnancy Management: Tubal and Interstitial SIGNS / SYMPTOMS DIAGNOSIS
8/29/19njm Ectopic Pregnancy Management: Tubal and interstitial SIGNS / SYMPTOMS Pain and vaginal bleeding are the hallmark symptoms of ectopic pregnancy. Pain is almost universal; it is generally lower abdominal and unilateral. Bleeding is also very common following a short period of amenorrhea. Physical exam may reveal a tender adnexal mass, often mentioned in texts, but noted clinically only 20 percent of the time. Furthermore, it may easily be confused with a tender corpus luteum of a normal intrauterine pregnancy. Finally signs and symptoms of hemoperitoneum and shock can occur, including a distended, silent, “doughy” abdomen, shoulder pain, bulging cul de sac into the posterior fornix of the vagina, and hypotension. DIAGNOSIS Initially, serum hCG rises, but then usually plateaus or falls. Transvaginal ultrasound scanning is a key diagnostic tool and can rapidly make these diagnoses: 1. Ectopic is ruled out by the presence of an intrauterine pregnancy with the exception of rare heterotopic pregnancy 2. Ectopic is proven when a gestational sac and an embryo with a heartbeat is seen outside of the uterus 3. Ectopic is highly likely if ANY adnexal mass distinct from the corpus luteum or a significant amount of free pelvic fluid is seen. When ultrasound is not definitive, correlation of serum hCG levels is important. If the hCG is above the “discriminatory zone” of 3000 mIU/ml IRP, a gestational sac should be visible on transvaginal ultrasound. The discriminatory zone varies by ultrasound machine and sonographer. If an intrauterine gestational sac is not visible by the time the hCG is at, or above, this threshold, the pregnancy has a high likelihood of being ectopic. -
Clinical Correlates of Histopathological Entities of the Placenta
Clinical Clinical correlates of histopathological entities of the placenta Admire Matsika PLACENTAL EXAMINATION has a critical research on the understanding of the role in understanding adverse fetal clinical implications of placental lesions in and maternal outcomes in pregnancy. obstetric and neonatal care. Background General and allied health practitioners However, progress in correlating placental This review provides medical caring for pregnant women and neonates pathology with clinical phenotypes has practitioners with an update on new often encounter placental histopathological been hampered by methodological issues terminology and status quo of research on reports with esoteric diagnostic entities of in many studies published.1 Additionally, placental entities of clinical significance contentious clinical significance such as there appears to be a knowledge disparity that may recur in subsequent pregnancy chronic villitis, massive perivillous fibrin between perinatal pathologists reporting and for which alteration of obstetric care deposition, chronic histiocytic intervillositis, microscopic changes seen in the organ and may improve outcomes. With the advent materno-fetal vascular malperfusion and delayed villous maturation. These lesions understanding of the clinical significance of the electronic My Health Record may recur in subsequent pregnancies. of placental histopathological diagnoses by system implemented Australia-wide, obstetric care providers.2 When reported patients will have direct access to their Objective and interpreted -
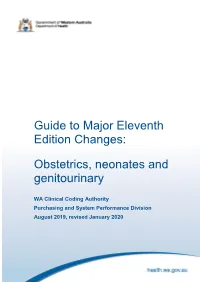
Guide to Major Eleventh Edition Changes: Obstetrics, Neonates And
Guide to Major Eleventh Edition Changes: Obstetrics, neonates and genitourinary WA Clinical Coding Authority Purchasing and System Performance Division August 2019, revised January 2020 1 Contents Chapter 15 Pregnancy, childbirth and the puerperium 3 ACS 1500 Diagnosis sequencing in obstetric episodes of care 3 ACS 1505 Delivery and assisted delivery codes 3 Delivery of baby prior to the admitted episode of care 5 ACS 1550 Discharge/transfer in labour 7 Transfer in first stage of labour 7 Transfer in third stage of labour 7 Failed induction of labour 9 Postpartum haemorrhage 9 ACS 1551 Obstetric perineal lacerations/grazes 11 ACS 1511 Termination of pregnancy (abortion) 11 ACS 1544 Complications following pregnancy with abortive outcome 14 Complications following abortion 14 Admission for retained products of conception following abortion 16 Hypoglycaemia in gestational diabetes mellitus 16 Mental Health and pregnancy 16 Neonates 16 Genitourinary 17 Acknowledgement 17 2 This guide was updated in January 2020 with creation of Examples 6, 7 and 19. Chapter 15 Pregnancy, childbirth and the puerperium Amendments include: Changes to code titles to specify ‘in pregnancy, childbirth and the puerperium.’ Changes to ACS titles for 1500 Diagnosis sequencing in obstetric episodes of care, 1511 Termination of pregnancy (abortion) and 1544 Complications following pregnancy with abortive outcome. Deletion of Excludes notes throughout ICD-10-AM to promote multiple condition coding. Clarification that codes from other chapters may be assigned to add specificity. Creation of four character codes to classify failed medical and surgical induction of labour. Indexing amendments to clarify code assignment for failed trial of labour and failure to progress unspecified, with or without identification of an underlying cause. -
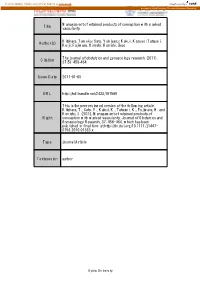
Title Management of Retained Products of Conception with Marked
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Management of retained products of conception with marked Title vascularity. Kitahara, Tomoko; Sato, Yukiyasu; Kakui, Kazuyo; Tatsumi, Author(s) Keiji; Fujiwara, Hiroshi; Konishi, Ikuo The journal of obstetrics and gynaecology research (2011), Citation 37(5): 458-464 Issue Date 2011-01-05 URL http://hdl.handle.net/2433/197589 This is the peer reviewed version of the following article: Kitahara, T., Sato, Y., Kakui, K., Tatsumi, K., Fujiwara, H. and Konishi, I. (2011), Management of retained products of Right conception with marked vascularity. Journal of Obstetrics and Gynaecology Research, 37: 458‒464, which has been published in final form at http://dx.doi.org/10.1111/j.1447- 0756.2010.01363.x Type Journal Article Textversion author Kyoto University 1 Management of Retained Products of Conception with Marked Vascularity 2 3 Tomoko Kitahara, Yukiyasu Sato*, Kazuyo Kakui, Keiji Tatsumi, Hiroshi Fujiwara, and 4 Ikuo Konishi 5 6 Department of Gynecology and Obstetrics, Kyoto University Graduate School of 7 Medicine 8 9 *Address correspondence and reprint requests to: Yukiyasu Sato, M.D., Ph.D. 10 Department of Gynecology and Obstetrics, Kyoto University Graduate School of 11 Medicine, Sakyo-ku, Kyoto 606-8507, Japan. 12 Tel; 81-75-751-3269: Fax; 81-75-761-3967: E-mail; [email protected] 13 14 Short title; Management of Hypervascular RPOC 15 Keywords; color Doppler, uterine artery embolization, expectant management 16 1 1 Abstract 2 3 Cases of retained products of conception (RPOC) with marked vascularity present a 4 clinical challenge because simple dilation and curettage (D&C) can lead to 5 life-threatening hemorrhage. -

Associations Between Phenotypes of Preeclampsia and Thrombophilia
European Journal of Obstetrics & Gynecology and Reproductive Biology 194 (2015) 199–205 Contents lists available at ScienceDirect European Journal of Obstetrics & Gynecology and Reproductive Biology jou rnal homepage: www.elsevier.com/locate/ejogrb Associations between phenotypes of preeclampsia and thrombophilia a, a a b Durk Berks *, Johannes J. Duvekot , Hillal Basalan , Moniek P.M. De MAAT , a a Eric A.P. Steegers , Willy Visser a Department of Obstetrics and Gynecology, Division of Obstetrics and Prenatal Medicine, Erasmus MC, University Medical Center Rotterdam, The Netherlands b Department of Hematology, Erasmus MC, University Medical Center Rotterdam, The Netherlands A R T I C L E I N F O A B S T R A C T Article history: Objectives: Preeclampsia complicates 2–8% of all pregnancies. Studies on the association of preeclampsia Received 29 July 2015 with thrombophilia are conflicting. Clinical heterogeneity of the disease may be one of the explanations. Received in revised form 4 September 2015 The present study addresses the question whether different phenotypes of preeclampsia are Accepted 17 September 2015 associated with thrombophilia factors. Study design We planned a retrospective cohort study. From 1985 until 2010 women with Keywords: preeclampsia were offered postpartum screening for the following thrombophilia factors: anti- Fetal growth restriction phospholipid antibodies, APC-resistance, protein C deficiency and protein S deficiency, hyperhomo- HELLP syndrome cysteineamia, factor V Leiden and Prothrombin gene mutation. Hospital records were used to obtain Pre-eclampsia information on phenotypes of the preeclampsia and placental histology. Retrospective study Thrombophilia Results: We identified 844 women with singleton pregnancies who were screened for thrombophilia factors. -

Superb Microvascular Imaging of Retained Placenta with Placenta
PICTURE OF THE MONTH Superb Microvascular Imaging of Retained Placenta with Placenta Accreta Spectrum Toshiyuki Hata1, Uiko Hanaoka2, Ayumi Mori3, Kenta Yamamoto4, Chiaki Tenkumo5, Nobuhiro Mori6, Kenji Kanenishi7, Hirokazu Tanaka8 ABSTRACT We present our first experience of using superb microvascular imaging (SMI) with an 18-MHz linear probe to diagnose placenta accreta spectrum (PAS) in the retained placenta after vaginal delivery. In the first case, irregular minimal invasion of the retained placenta into the anterior myometrium and a thin uterine wall were clearly noted. In the second case, SMI clearly demonstrated the loss of myometrium anterior to fundal lesions and abnormally dilated, torturous, stem villous vessels invading until the uterine serosa. SMI with the use of an 18-MHz linear probe may be a novel diagnostic tool for the diagnosis of PAS in the retained placenta after delivery. Keywords: 18-MHz linear probe, High-resolution ultrasound, Placenta accreta spectrum, Retained placenta, Superb microvascular imaging. Donald School Journal of Ultrasound in Obstetrics and Gynecology (2019): 10.5005/jp-journals-10009-1600 INTRODUCTION 1–8 Department of Perinatology and Gynecology, Kagawa University A placenta accreta spectrum (PAS) is one of the most serious and Graduate School of Medicine, Miki, Kagawa, Japan potentially life-threatening conditions for both a pregnant woman 1 Corresponding Author: Toshiyuki Hata, Department of Perinatology and fetus. The precise prenatal diagnosis of PAS improves the and Gynecology, Kagawa University Graduate School of Medicine, prognosis of the patient and reduces maternal morbidity.2 The Miki, Kagawa, Japan, Phone: +81-87-891-2174, e-mail: toshi28@med. European Working Group on PAS has proposed standardized kagawa-u.ac.jp 3 ultrasound descriptors of this spectrum. -

Operative Hysteroscopy for Retained Products of Conception: Efficacy and Subsequent Fertility
Journal of Gynecology Obstetrics and Human Reproduction 48 (2019) 151–154 Available online at ScienceDirect www.sciencedirect.com Original Article Operative hysteroscopy for retained products of conception: Efficacy and subsequent fertility a,b, a a a Perrine Capmas *, Anina Lobersztajn , Laura Duminil , Tiphaine Barral , a,c a,b,c Anne-Gaëlle Pourcelot , Hervé Fernandez a AP-HP, Department of Gynecology and Obstetrics, Hospital Bicêtre, GHU Sud, F-94276, Le Kremlin Bicêtre, France b INSERM, U1018, Centre of research in Epidemiology and population health (CESP), F-94276, Le Kremlin Bicêtre, France c Faculty of medicine, University Paris Saclay, F-94276, Le Kremlin Bicêtre, France A R T I C L E I N F O A B S T R A C T Article history: Retained product of conception complicates nearly 1% of pregnancies and can lead to synechiae and Received 18 June 2018 compromise ulterior fertility. The aim of this study is to evaluate efficiency of operative hysteroscopy in Received in revised form 11 December 2018 management of retained products of conception (RPOC). Secondary objectives are assessments of intra- Accepted 12 December 2018 uterine adhesions rate and later fertility. Available online 12 December 2018 This unicentric retrospective study includes women who undertook an operative hysteroscopy for retained products of conception between January 2012 and March 2014. Assessment of the efficiency of Keywords: operative hysteroscopy is defined by a complete resection of retained products of conception confirmed Hysteroscopy by office hysteroscopy. Retained product of conception One hundred fourteen women were included in the study. Efficiency of operative hysteroscopy for Intra-uterine adhesions Fertility retained products of conception is 91% for women with a postoperative office hysteroscopy. -

Pathological Examination of the Placenta: Raison D'être, Clinical
Review Article Singapore Med J 2009; 50(12) : 1123 Pathological examination of the placenta: Raison d’être, clinical relevance and medicolegal utility Chang K T E ABSTRACT pregnancy outcome; Formal pathological examination of the (3) Improved management of subsequent pregnancies placenta provides valuable information to by the identification of conditions known to have the obstetrician, neonatologist, paediatrician recurrence risks or which may be either treatable or and family. This article aims to provide the preventable; clinician with an overview of the significance of (4) Identification of a pathological condition requiring placental examination in relation to common or timely clinical intervention; important pathological processes, and the utility (5) Understanding of antenatal and intrapartum events of information obtained therein in explaining that contribute to long-term neurodevelopmental adverse outcomes, management of subsequent sequelae, with early identification of such changes pregnancies, and assessment of newborn risk for making possible early interventions and improvement the development of short- or long-term sequelae. in long-term outcome; General guidelines for placental examination, and (6) Assessment of factors contributing to poor outcome logistical and practical issues are also discussed. as a factual basis for resolving medicolegal issues. Finally, the role of the placenta in the defence of The multidisciplinary team approach is well obstetricians and other healthcare workers in established in oncology.(4) A similar model for perinatal cases of poor neonatal outcome is described. medicine is appropriate,(5) and may involve obstetricians, neonatologists, ultrasonographers, obstetrical Keywords: medicolegal, placenta, placental anaesthetists, clinical geneticists, paediatric surgeons and pathological examination, poor neonatal paediatric pathologists. This may serve both as a working outcome conference to review and discuss current case issues, and Singapore Med J 2009; 50(12): 1123-1133 as a teaching conference.