A Clinic-Microbiological Study of Mycotic Corneal Ulcers Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

M Nurul Islam Executive Editor Sk Hafizur Rahman Associate Editors Najib Anwar Ekramul Haque Shaikh Graphics Md Golam Kibriya
Al-AmeenZ Mission Advisors Ekram Ali Prof Rafikul Islam Dr Sk Md Hassan Editor M Nurul Islam Executive Editor Sk Hafizur Rahman Associate Editors Najib Anwar Ekramul Haque Shaikh Graphics Md Golam Kibriya Published by M Nurul Islam from 53B Elliot Road, Kolkata 700 016 on behalf of Al- Ameen Mission Trust and printed at Diamond Art Press, 37/A Bentinck Street, Kolkata 700 069. Ph: 033-3297 3580 Fax: 033-2229 3769 e-mail: [email protected] website: www.alameenmission.in facebook.com/alameenmission.newsletter (M Nurul Islam) A R C H I V E School Bells Echo Amidst Paddy Fields In 1986, Nurul Islam set up a hostel with 11 students, collecting one fist of rice from every home in his village, Khalatpur. In January 1987, it was named as Al-Ameen Mission which has today become a model for excellent education standards. By A Staff Reporter are over 300 students following the West Bengal Council of Higher Secondary Education syllabus. The Al-Ameen In a country like India, we cannot leave the less privileged Mission receives over 6000 applications for admissions to the merciless hands of the market forces. The solution from the whole of West Bengal. The admission test is to this problem perhaps lies somewhere, far away from held at 28 centres. The students go through a pre-se- the issue of reservations in higher education that is ter- lection exam, an interview and a test of reasoning. The ribly resented by the more meritorious. In a village called intake of students for the campus is around 500 to 600. -

WEST BENGAL COVID-19 HEALTH BULLETIN – 18Th APRIL 2021
Department of Health & Family Welfare Govt. of West Bengal WEST BENGAL COVID-19 HEALTH BULLETIN – 18th APRIL 2021 Active COVID-19 Cases as on 18th April: 49,638 I S. No Subject Number 1 Total COVID-19 Cases till 17th April 6,51,508 2 New COVID-19 Cases on 18th April 8,419 3 Total COVID-19 Cases till 18th April (1+2) 6,59,927 4 Total Discharged 5,99,721 (+4,053) 5 Total Deaths as on 18th April* 10,568 (+28) 6 Active COVID-19 Cases as on 18th April 49,638 (+4,338) COVID 19 COVID STATUS 7 Discharge Rate (4/3) 90.88% Note: All figures updated till 9AM, 18th April #Daily increase/decrease with respect to previous day is shown as (+/-) *Complete analysis can be referred from Section X, (Page no. 5) S. No Subject Number II 1 Samples Tested till 17th April 97,62,086 2 Samples Tested on 18th April 46,074 3 Total Number of Samples Tested till 18th April (1+2) 98,08,160 4 Tests per Million population 1,08,980 5 % of Positive Cases out of Samples Tested 6.73% 6 Total Testing Laboratories* 105 7 Testing Laboratories added this week 0 TESTING TESTING SNAPSHOT 8 Testing Laboratories pending approval 1 *Detailed breakup of these laboratories is given on Page 4 and Page 5 S. No Subject Number III 1 Total Number of Hospitals dedicated for treating COVID-19 61 2 Total Number of Govt. Hospitals dedicated for treating COVID-19 49 3 Total Number of Pvt. -

Admission Notice
Page - 1 of 3 State Medical Faculty of West Bengal 14-C, Beliaghata Main Road, Kolkata -700 085 2372-0185 / 2372-0181 www.smfwb.in No- 1148 F-4/2021 24th August, 2021 NOTICE FOR ADMISSION TO PARA MEDICAL COURSES SESSION BEGINNING 1st DECEMBER, 2021. I. Online Applications are invited by the State Medical Faculty of West Bengal for admission to under-mentioned Para Medical Courses at different Government and Affiliated Institutes of West Bengal from 26-08-2021 to 10-09-2021. a) “Application Form” is available in the Website: www.smfwb.in / www.smfwb.examflix.in b) The amount of Application Fees to be paid for appearing in the SMFWBEE-2021 is Rs.500/- (Rupees five hundred only). The Application Fees can be paid in cashless mode by ‘Net Banking’/’Debit Card’/Credit Card’. c) Rs.100/- as Registration Fees for participating in Online Counseling and for Choice filling, indicating choice of institute, Course and locking, to be paid by Net Banking’/’Debit Card’/Credit Card’ only. [ Note: Registration will be done Only in first round and Only registered students can participate for further rounds.] d) The above Fees are non-refundable. Sl Name of Courses Short Name of Courses No 1 Diploma in Medical Laboratory Technology DMLT(Tech) 2 Diploma in Radiography [ Diagnostic ] DRD(Tech) 3 Diploma in Physiotherapy DPT 4 Diploma in Radiotherapeutic Technology DRT 5 Diploma in Optometry with Ophthalmic Technique D.OPT 6 Diploma in Neuro Electro Physiology DNEP 7 Diploma in Perfusion Technology DPFT 8 Diploma in Cath-Lab Technician DCLT 9 Diploma in Critical Care Technology DCCT 10 Diploma in Dialysis Technique Dialysis (Tech) 11 Diploma In Operation Theatre Technology DOTT 12 Diploma In Diabetes Care Technology DDCT 13 Diploma In Electrocardiographic Technique ECG (Tech) e) Eligibility For Admission : a) Qualification : Passed Higher Secondary (10+2), or equivalent examination recognized by any Indian university, or duly constituted Board, with pass mark in Physics, Chemistry & Biology individually. -

WEST BENGAL COVID-19 HEALTH BULLETIN – 24Th AUG 2021
Department of Health & Family Welfare Govt. of West Bengal WEST BENGAL COVID-19 HEALTH BULLETIN – 24th AUG 2021 I S. No Subject Number 1 New COVID-19 Cases on 24th Aug 613 2 Total COVID-19 Cases till 24th Aug 15,44,109 3 Total Discharged 15,16,509 (+720) 4 Total Deaths as on 24th Aug* 18,383 (+12) 5 Active COVID-19 Cases as on 24th Aug 9,217 (-119) 6 Discharge Rate (3/2) 98.21% COVID 19 STATUS 19 COVID 7 Fatality Rate (4/2) 1.19% Note: All figures updated till 9AM, 24th Aug #Daily increase/decrease with respect to previous day is shown as (+/-) *Complete analysis can be referred from Section X, (Page no. 5) II S. No Subject Number 1 Samples Tested on 24th Aug 41,262 2 Total Number of Samples Tested till 24th Aug 1,67,30,555 3 Positivity Rate as on 24th Aug 1.49% 4 Tests per Million population 1,85,895 TESTING 5 Total Testing Laboratories* 136 SNAPSHOT 6 RT-PCR/Antigen Test Ratio 42:58 *Detailed breakup of these laboratories is given on Page 3 and Page 4 III S. No Subject Number 1 Total Number of Hospitals dedicated for treating COVID-19 203 2 Total Number of Govt. Hospitals dedicated for treating COVID-19 196 3 Total Number of Pvt. Hospitals requisitioned for treating COVID-19 7 4 Total Number of earmarked COVID-19 Beds 23,947 5 % Occupancy in COVID Beds 2.99% SNAPSHOT TREATMENT TREATMENT 6 Total ICU/HDU Beds in the COVID Hospitals 2,861 INFRASTRUCTURE 7 Total Number of Safe Homes 200 8 Total Number of Beds in Safe Homes 11,507 IV S. -

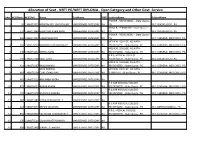
Sl District Hospital Type Hospital Code Hospital Name
#Sl District Hospital Type Hospital Code Hospital Name 1 01-DARJEELING PUBLIC 190100504 DISTRICT HOSPITAL DARJEELING ACTIVE (97) 2 01-DARJEELING PUBLIC 190100278 KHARIBARI RURAL HOSPITAL ACTIVE (834) KURSEONG SUB DIVISIONAL 3 01-DARJEELING PUBLIC 190100020 ACTIVE (35) HOSPITAL 4 01-DARJEELING PUBLIC 190100470 MATIGARA HOSPITAL ACTIVE (121) 5 01-DARJEELING PUBLIC 190100277 NAXALBARI RURAL HOSPITAL ACTIVE (1406) NORTH BENGAL MEDICAL COLLEGE 6 01-DARJEELING PUBLIC 190100477 ACTIVE (2257) & HOSPITAL 7 01-DARJEELING PUBLIC 190100138 PHANSIDEWA BPHC ACTIVE (349) #Sl District Hospital Type Hospital Code Hospital Name 8 01-DARJEELING PUBLIC 190100478 SILIGURI DISTRICT HOSPITAL ACTIVE (575) AVALON HOSPITAL ( A UNIT OF 9 01-DARJEELING PRIVATE 190101524 HEMENDRA SMRITI HEALTH CARE ACTIVE (6) PVT.LTD.) 10 01-DARJEELING PRIVATE 190100602 CENTRE FOR EYE SIGHT ACTIVE (689) 11 01-DARJEELING PRIVATE 190100711 GLOBAL NURSING HOME ACTIVE (148) 12 01-DARJEELING PRIVATE 190101098 HOLY PALACE CHRISTIAN HOSPITAL ACTIVE (16) MEDICA CANCER HOSPITAL (A UNIT 13 01-DARJEELING PRIVATE 190101118 ACTIVE (2655) OF NORTH BENGAL CLINIC PVT LTD) 14 01-DARJEELING PRIVATE 190100454 MEDICA NORTH BENGAL CLINIC ACTIVE (156) #Sl District Hospital Type Hospital Code Hospital Name 15 01-DARJEELING PRIVATE 190101429 MUKHERJEE HOSPITAL ACTIVE (1) NAVJEEVAN HOSPITAL & RURAL 16 01-DARJEELING PRIVATE 190100021 ACTIVE (3636) HEALTH CARE CENTRE NORTH BENGAL NEURO CENTER PVT 17 01-DARJEELING PRIVATE 190100612 ACTIVE (1) LTD 18 01-DARJEELING PRIVATE 190101495 REDDY HEALTHCARE PVT. LTD. -

Saifuddin Molla Sainaz Parvin Md Shabbir Alam Moriam
1 MDFC/12- SAMSUDDIN DIPLOMA IN 13/2297 MOLLA ELECTRICAL SAIFUDDIN ENGINEERING MOLLA 2 MDFC/13- SK GOLAM KADIR GENERAL 14/6834 NURSING AND SAINAZ PARVIN MIDWIFERY 3 MDFC/12- MD KHURSHID B.TECH IN 13/5609 ALAM Mechanical MD SHABBIR Engineering(ME) ALAM 4 MDFC/13- ABDUL MANNAN G.N.M NURSING 14/3431 MORIAM KHAN KHATUN 5 MDFC/13- KHAIRUL SARDAR BACHELOR IN 14/5292 COMPUTER BADARUDDIN APPLICATION SARDAR (BCA) 6 MDFC/13- NAZRUL DIPLOMA IN Civil 14/5703 NAZMA GHARAMI Engineering(CE) 7 MDFC/13- ABDUR ROUF BECHELOR IN 14/6098 GAZI OPTOMETRY(B.O SHARIF PTOM) AHAMMED GAZI 8 MDFC/13- KUTUBUDDIN B.TECH IN Civil 14/1554 AHAMED MOLLICK Engineering(CE) SHAKIR MOLLICK 9 MDFC/13- LT. SK SANOWAR M.TECH IN 14/2414 ALI COMPUTER SK ANAMUL SCIENCE AND SANOWAR ENGINEERING 10 MDFC/13- MD RAFIK SK B.Pharma 14/4605 JUEL SK 11 MDFC/13- YEASUDAS PAUL B.TECH IN Marine 14/4330 NICOLE RAHUL Engineering(MRE) PAUL 12 MDFC/13- FAZLUL HAQUE B.Pharma 14/3603 OLYUL HAQUE 13 MDFC/13- ABDUL HAKIM B.Pharma 14/6986 NABINUR ISLAM 14 MDFC/12- NAZMUL ISLAM Bachelor of 13/5860 Homeopathic NAZNEEN Medicine & SAKHEE Surgery(BHMS) 15 MDFC/12- MOSEN SHAIK B.TECH IN 13/4445 CERAMIC BANARUL SHAIK TECHNOLOGY 16 MDFC/12- BABULAL ALI B.TECH IN Textile 13/3505 KHAN Engineering/Tech IMRAN ALI KHAN nology(TXT) 17 MDFC/12- SIRAFUDDIN B.TECH IN 13/5748 KHAN Electrical Eng.or LILTU KHAN Electrical & Electronics Eng.(EEE) 18 MDFC/12- FARUK HASAN B.TECH IN 13/3685 Information GORIB NAWAZ Technology(IT) 19 MDFC/12- MD KHURSHID B.TECH IN 13/5609 ALAM Mechanical MD SHABBIR Engineering(ME) ALAM 20 MDFC/12- MD WAHID L.L.B. -
Allocation of Seat - NEET PG/NEET DIPLOMA - Open Category and Other Govt
Allocation of Seat - NEET PG/NEET DIPLOMA - Open Category and Other Govt. Service SLNo NEETRank NEETRoll Name CastName PWD InstituteName SubjectName IPGMER - RECOGNIZED - State Quota - 1 26 1966073373 APRATIM ROY CHOUDHURY UNRESERVED CATEGORY NA PG M.D. (RADIOLOGY) - PG IPGMER - PERMITTED - State Quota - 2 131 1966073444 HUMAYUN KABIR KHAN UNRESERVED CATEGORY NA PG M.D. (RADIOLOGY) - PG IPGMER - RECOGNIZED - State Quota - 3 268 1966044219 SUBHANKAR ROY UNRESERVED CATEGORY NA PG M.D. (GENERAL MEDICINE) - PG MEDICAL COLLEGE, KOLKATA - 4 269 1966076003 DEBANSHU CHAKRABORTY UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. (GENERAL MEDICINE) - PG MEDICAL COLLEGE, KOLKATA - 5 340 1966071872 DEBRAJ SAHA UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. (GENERAL MEDICINE) - PG N.R.S, MEDICAL COLLEGE - 6 392 1966075160 SRIJIT SAHA UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. (RADIOLOGY) - PG MEDICAL COLLEGE, KOLKATA - 7 431 1966071167 BABLU NANDI UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. (GENERAL MEDICINE) - PG ARKA PRABHA MEDICAL COLLEGE, KOLKATA - 8 460 1966076198 CHATTOPADHYAY UNRESERVED CATEGORY NA PERMITTED - State Quota - PG M.D. (GENERAL MEDICINE) - PG 9 461 1966071033 ABHINABA HAZRA UNRESERVED CATEGORY NA R.G.KAR MEDICAL COLLEGE - 10 605 1966076153 ARNAB ADHYA UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. (GENERAL MEDICINE) - PG R.G.KAR MEDICAL COLLEGE - 11 772 1966073378 ANAMIKA BHADRA UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. (GENERAL MEDICINE) - PG 12 787 1966071382 DISHA CHAKRABORTY UNRESERVED CATEGORY NA R.G.KAR MEDICAL COLLEGE - 13 923 1966074077 ARPAN SAMANTA UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.S. (ORTHOPAEDICS) - PG N.R.S, MEDICAL COLLEGE - 14 956 1966073857 SAYANTAN CHAKRABORTY UNRESERVED CATEGORY NA RECOGNIZED - State Quota - PG M.D. -
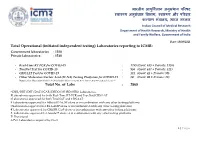
Laboratories Reporting to ICMR
भारतीय आयु셍वज्ञि ान अनुसंधान पररषद वा्य अनुसंधान 셍वभाग, वा्य और पररवार क쥍याण मंत्रालय, भारत सरकार Indian Council of Medical Research Department of Health Research, Ministry of Health and Family Welfare, Government of India Date: 13/08/2021 Total Operational (initiated independent testing) Laboratories reporting to ICMR: Government laboratories : 1320 Private laboratories : 1548 - Real-Time RT PCR for COVID-19 : 1759 (Govt: 633 + Private: 1126) - TrueNat Test for COVID-19 : 958 (Govt: 637 + Private: 321) - CBNAAT Test for COVID-19 : 131 (Govt: 42 + Private: 89) - Other Molecular-Nucleic Acid (M-NA) Testing Platforms for COVID-19 : 20 (Govt: 08 + Private: 12) Note: Other Molecular-Nucleic Acid includes Abbott ID NOW, RT-LAMP, CRISPR-Cas9 and Accula™ Total No. of Labs : 2868 *CSIR/DBT/DST/DAE/ICAR/DRDO/MHRD/ISRO Laboratories. #Laboratories approved for both Real-Time RT-PCR and TrueNat/CBNAAT $Laboratories approved for both TrueNAT and CBNAAT ¥ Laboratories approved for Abbott ID NOW alone or in combination with any other testing platforms @Laboratories approved for RT-LAMP alone or in combination with any other testing platforms € Laboratories approved for CRISPR-Cas9 alone or in combination with any other testing platforms δ Laboratories approved for Accula™ alone or in combination with any other testing platforms P: Provisional Δ Pvt. Laboratories acquired by Govt. 1 | P a g e S. Test Names of States Names of Government Institutes Names of Private Institutes No. Category 1. Andhra Pradesh RT-PCR 1. Sri Venkateswara Institute of Medical 1. Manipal Hospital, Tadepalli, Guntur (133) Sciences, Tirupati 2. -

Solidarity Statement Against Police Brutality at Jamia Millia Islamia University and Aligarh Muslim University
Solidarity Statement Against Police Brutality at Jamia Millia Islamia University and Aligarh Muslim University We, the undersigned, condemn in the strongest possible terms the police brutality in Jamia Millia Islamia University, New Delhi, and the ongoing illegal siege and curfew imposed on Aligarh Muslim University, Aligarh. On 15th December 2019 Delhi police in riot-gear illegally entered the Jamia Millia campus and attacked students who are peacefully protesting the Citizenship Amendment Act. The Act bars Muslims from India’s neighboring countries from the acquisition of Indian citizenship. It contravenes the right to equality and secular citizenship enshrined in the Indian constitution. On the 15th at JMIU, police fired tear gas shells, entered hostels and attacked students studying in the library and praying in the mosque. Over 200 students have been severely injured, many who are in critical condition. Because of the blanket curfew and internet blockage imposed at AMU, we fear a similar situation of violence is unfolding, without any recourse to the press or public. The peaceful demonstration and gathering of citizens does not constitute criminal conduct. The police action in the Jamia Millia Islamia and AMU campuses is blatantly illegal under the constitution of India. We stand in unconditional solidarity with the students, faculty and staff of Jamia Millia Islamia and Aligarh Muslim University, and express our horror at this violent police and state action. With them, we affirm the right of citizens to peaceful protest and the autonomy of the university as a non-militarized space for freedom of thought and expression. The brutalization of students and the attack on universities is against the fundamental norms of a democratic society. -

WEST BENGAL COVID-19 HEALTH BULLETIN – 17Th APRIL 2021
Department of Health & Family Welfare Govt. of West Bengal WEST BENGAL COVID-19 HEALTH BULLETIN – 17th APRIL 2021 Active COVID-19 Cases as on 17th April: 45,300 I S. No Subject Number 1 Total COVID-19 Cases till 16th April 6,43,795 2 New COVID-19 Cases on 17th April 7,713 3 Total COVID-19 Cases till 17th April (1+2) 6,51,508 4 Total Discharged 5,95,668 (+3,426) 5 Total Deaths as on 17th April* 10,540 (+34) 6 Active COVID-19 Cases as on 17th April 45,300 (+4,253) COVID 19 COVID STATUS 7 Discharge Rate (4/3) 91.43% Note: All figures updated till 9AM, 17th April #Daily increase/decrease with respect to previous day is shown as (+/-) *Complete analysis can be referred from Section X, (Page no. 5) S. No Subject Number II 1 Samples Tested till 16th April 97,15,115 2 Samples Tested on 17th April 46,971 3 Total Number of Samples Tested till 17th April (1+2) 97,62,086 4 Tests per Million population 1,08,468 5 % of Positive Cases out of Samples Tested 6.67% 6 Total Testing Laboratories* 105 7 Testing Laboratories added this week 0 TESTING TESTING SNAPSHOT 8 Testing Laboratories pending approval 1 *Detailed breakup of these laboratories is given on Page 4 and Page 5 S. No Subject Number III 1 Total Number of Hospitals dedicated for treating COVID-19 61 2 Total Number of Govt. Hospitals dedicated for treating COVID-19 49 3 Total Number of Pvt. -

360089 Samim Resume.Pdf
Dr. SK SAMIM FERDOWS Sk Samim Ferdows teaches Bio-Statistics, at the IQ City Medical College, West Bengal. He is a Doctorate from University of Burdwan. He has written on issues related to Statistical Analysis, Environmental Impact, Regional Development, Knowledge Management, and Industrialisation. His works have been published in Various Journals like ZENITH International Journal, International Journal of Multidisciplinary Research, Journal of Knowledge Management, Economics and Information Technology, Research Vistas, CLEAR International Journal of Research in Engineering and Technology, NJMRA, The IASMS Journal, Rabindra Bharati University Journal of Economics, The Alternative Journal of Management Science and Research, BIT Mesra etc. as also in various edited volumes. He has one book to his credit. Current Position: Associate Professor [from 1st Oct. 2014] EDUCATION PhD on Environmental Cost of Industrialization in West Bengal: A Study in Durgapur Region, 2012, from University of Burdwan [ Guide: Dr. Rajarshi Majumder]. M.Sc in Statistics, 2000, from University of Burdwan [1st Class (Marks obtained 62.9%)]. One-year Diploma Course in Computer from TULEC at Burdwan. B.Sc (Honours) in Statistics, 1998, From University of Kalyani [2nd Class]. Higher Secondary,1993, First Division, From Bhanderhati B.M Institution., under WBCHSE board (Marks obtained 72.9%). Madhyamik, 1991, First Division, under WBBME board (Marks obtained 76.4%). 1 Areas of Teaching: Statistics, Econometrics, Quantitative Methods, Research methodology and Operation Research. Areas of Research Interest: Industrialisation, Statistics, Environmental Impact. Publications: Research Publications in Journals : 19 (nineteen), Books: 02 (Two) Books: 1. “Fundamentals of Quantitative Methods” – Dr. Sk Samim Ferdows . Published by Binoy Prakashani Publishers [ISBN- 81-903768-0-10], Burdwan, West Bengal. -

IQ City Medical College
IQ City Medical College Durgapur An exclusive Guide by IQ City Medical College Cutoff 2020/2019/2018 Every year IQ City Medical College admissions are conducted for the students on the basis of cut off declared by IQ City Medical College. At Shiksha.com you can find IQ City Medical College 2021 cut offs, for all 8 courses offered by the college. Cut off data available on Shiksha will help you to apply for MBBS,MD courses in IQ City Medical College, Durgapur Cut-Offs for Last Round (General Category) Showing Cut off values only for the years for which we have data MBBS - Bachelor of Medicine and Bachelor of Surgery Durgapur Offered by WBUHS - The West Bengal University of Health Sciences NEET 2020 Round Cut-off by rank 1 40986 2 39014 Click to see NEET Cut-Off for All Rounds WEST BENGAL NEET 2020 Round Cut-off by rank Disclaimer: This PDF is auto-generated based on the information available on Shiksha as on 26-Sep-2021. 1 40986 2 39014 Click to see West Bengal NEET Cut-Off for All Rounds MD in Community Medicine Durgapur Offered by WBUHS - The West Bengal University of Health Sciences WEST BENGAL NEET PG 2020 Round Cut-off by rank 1 96963 Click to see West Bengal NEET PG Cut-Off for All Rounds Know more about this College IQ City Medical College Scholarship Details IQ City Medical College Courses & Fees 2021 IQ City Medical College Placement Trends & Updates Disclaimer: This PDF is auto-generated based on the information available on Shiksha as on 26-Sep-2021.