Pharmacological Management of Dysautonomia Following Traumatic Brain Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hitting a Wall: an Ambiguous Case of Wallenberg Syndrome
Open Access Case Report DOI: 10.7759/cureus.16268 Hitting a Wall: An Ambiguous Case of Wallenberg Syndrome James R. Pellegrini 1 , Rezwan Munshi 1 , Bohao Cao 1 , Samuel Olson 2 , Vincent Cappello 1 1. Internal Medicine, Nassau University Medical Center, East Meadow, USA 2. Physical Medicine and Rehabilitation, Stony Brook University, Stony Brook, USA Corresponding author: Bohao Cao, [email protected] Abstract Wallenberg syndrome is the most common stroke of the posterior circulation. Diagnosis of Wallenberg syndrome is often overlooked as initial MRI may show no visible lesion. We present an atypical case of Wallenberg syndrome in which the initial MRI of the brain was normal. Our patient is a 65-year-old male who was brought in by emergency medical services complaining of right- sided facial droop, slurred speech, and left-sided weakness for one day. Physical examination showed decreased left arm and leg strength compared to the right side, decreased left facial temperature sensations, decreased left arm and leg temperature sensations, and difficulty sitting upright with an associated leaning towards the left side. An initial magnetic resonance imaging (MRI) of the brain with and without contrast revealed no abnormality. In light of such a high suspicion for stroke based on the patient’s neurologic deficits, a repeat MRI of the brain was performed three days later and exposed a small focus of bright signal (hyperintensity) on T2-weighted fluid-attenuated inversion recovery and diffusion-weighted imaging (DWI) in the left posterior medulla. Wallenberg syndrome, also known as lateral medullary syndrome or posterior inferior cerebellar artery syndrome, is a constellation of symptoms caused by posterior vascular accidents. -

A Sign It's Time for BOTOX®
When OAB* due to MS† makes matters worse… A sign it’s time for BOTOX® Ask your patients if they still have leakage or can’t tolerate their current OAB medication *Overactive bladder. †Multiple sclerosis. Indication Detrusor Overactivity Associated With a Neurologic Condition BOTOX® for injection is indicated for the treatment of urinary incontinence due to detrusor overactivity associated with a neurologic condition (eg, SCI, MS) in adults who have an inadequate response to or are intolerant of an anticholinergic medication. IMPORTANT SAFETY INFORMATION, INCLUDING BOXED WARNING WARNING: DISTANT SPREAD OF TOXIN EFFECT Postmarketing reports indicate that the effects of BOTOX® and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening, and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity, but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have an underlying condition that would predispose them to these symptoms. In unapproved uses and in approved indications, cases of spread of effect have been reported at doses comparable to those used to treat Cervical Dystonia -
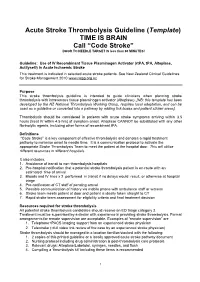
Acute Stroke Thrombolysis Guideline (Template) TIME IS BRAIN Call “Code Stroke” DOOR to NEEDLE TARGET IS Less Than 60 MINUTES!
Acute Stroke Thrombolysis Guideline (Template) TIME IS BRAIN Call “Code Stroke” DOOR TO NEEDLE TARGET IS less than 60 MINUTES! Guideline: Use of IV Recombinant Tissue Plasminogen Activator (rtPA, tPA, Alteplase, Actilyse®) in Acute Ischaemic Stroke This treatment is indicated in selected acute stroke patients. See New Zealand Clinical Guidelines for Stroke Management 2010 www.nzgg.org.nz Purpose This stroke thrombolysis guideline is intended to guide clinicians when planning stroke thrombolysis with intravenous tissue plasminogen activator (Alteplase). [NB: this template has been developed by the NZ National Thrombolysis Working Group, requires local adaptation, and can be used as a guideline or converted into a pathway by adding tick boxes and patient sticker areas]. Thrombolysis should be considered in patients with acute stroke symptoms arriving within 3.5 hours (treat IV within 4.5 hrs) of symptom onset. Alteplase CANNOT be substituted with any other fibrinolytic agents, including other forms of recombinant tPA. Definitions “Code Stroke” is a key component of effective thrombolysis and denotes a rapid treatment pathway to minimise onset to needle time. It is a communication protocol to activate the appropriate Stroke Thrombolysis Team to meet the patient at the hospital door. This will utilise different resources in different hospitals. It also includes: 1. Avoidance of transit to non-thrombolysis hospitals 2. Pre-hospital notification that a potential stroke thrombolysis patient is en-route with an estimated time of arrival 3. Bloods and IV lines x 2 performed in transit if no delays would result, or otherwise at hospital triage 4. Pre-notification of CT staff of pending arrival 5. -

Autonomic Dysreflexia – a Medical Emergency a Guide for Patients
Autonomic Dysreflexia – A Medical Emergency A guide for patients Only applicable to T6 level and above Key Points • Autonomic Dysreflexia (AD) is a medical emergency that occurs due to a rapid rise in blood pressure in response to a harmful or painful stimulus below the level of your Spinal Cord Injury (SCI) • It occurs in people with SCI at T6 and above but has in rare occasions been reported in individuals with SCI as low as T8 • If left untreated your blood pressure can rise to dangerous levels, risking stroke, cardiac problems, seizures, even death • Typically there is a pounding headache as your blood pressure rises. Other symptoms can include redness and sweating above the level of your SCI, slow heart rate, goosebumps, nausea, nasal congestion, blurred vision, shortness of breath and anxiety • Some or all of the symptoms may be present • AD can be triggered by any continuous painful or irritating stimulus below the level of your lesion. The most common causes are related to the bladder or bowel • Relieving the cause of the AD will resolve your AD episode • If the cause cannot be found or treated, medication is required to lower your blood pressure which may require a visit to your nearest emergency department • All people with SCI at T6 and above should carry their Autonomic Dysreflexia Medical Emergency Card at all times • The best treatment for AD is prevention • People at risk of AD often carry an ‘AD Kit’ with them – items useful to resolve AD such as catheters and prescribed medication 1 What is Autonomic Dysreflexia? Autonomic Dysreflexia (AD) is a medical emergency. -

Treatment of Autonomic Dysreflexia for Adults & Adolescents with Spinal
Treatment of Autonomic Dysreflexia for Adults & Adolescents with Spinal Cord Injuries Authors: Dr James Middleton, Director, State Spinal Cord Injury Service, NSW Agency for Clinical Innovation. Dr Kumaran Ramakrishnan, Honorary Fellow, Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney, and Consultant Rehabilitation Physician & Senior Lecturer, Department of Rehabilitation Medicine, University Malaya. Dr Ian Cameron, Head of the Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney. Reviewed and updated in 2013 by the authors. AGENCY FOR CLINICAL INNOVATION Level 4, Sage Building 67 Albert Avenue Chatswood NSW 2067 PO Box 699 Chatswood NSW 2057 T +61 2 9464 4666 | F +61 2 9464 4728 E [email protected] | www.aci.health.nsw.gov.au Produced by the NSW State Spinal Cord Injury Service. SHPN: (ACI) 140038 ISBN: 978-1-74187-972-8 Further copies of this publication can be obtained from the Agency for Clinical Innovation website at: www.aci.health.nsw.gov.au Disclaimer: Content within this publication was accurate at the time of publication. This work is copyright. It may be reproduced in whole or part for study or training purposes subject to the inclusion of an acknowledgment of the source. It may not be reproduced for commercial usage or sale. Reproduction for purposes other than those indicated above, requires written permission from the Agency for Clinical Innovation. © Agency for Clinical Innovation 2014 Published: February 2014 HS13-136 ACKNOWLEDGEMENTS This document was originally published as a fact sheet for the Rural Spinal Cord Injury Project (RSCIP), a pilot healthcare program for people with a spinal cord injury (SCI) conducted within New South Wales involving the collaboration of Prince Henry & Prince of Wales Hospitals, Royal North Shore Hospital, Royal Rehabilitation Centre Sydney, Spinal Cord Injuries Australia and the Paraplegic & Quadriplegic Association of NSW. -
Robert Jenkinson, MD
8/26/14 LIFE-THREATENING, INTRAOPERATIVE HEMODYNAMIC INSTABILITY IN A QUADRAPLEGIC Robert H. Jenkinson, M.D. Department of Anesthesiology University of Wisconsin Madison, WI Background o 57 year old quadraplegic male, remote C4-C5 spinal injury presenting for cystoscopy. n PMHx: Autonomic dysreflexia, OSA, neurogenic bowel/bladder. n Allergies: Sulfa drugs o Prior history of systolic blood pressure (SBP) near or above 200 mmHg while under GA for cystoscopy on multiple occasions. n Required nitroglycerine infusions. n Stable blood pressure with spinal anesthesia on one prior occasion. Case Description o L4-L5 spinal performed in OR n Intravenous midazolam (2mg) & fentanyl (50 mcg) n Intrathecal hyperbaric bupivacaine (12.5 mg) n Intravenous cefazolin (2g) o On return to supine position: n SBP rapidly decreased from baseline of 140 mmHg to 60 mmHg. n The patient became tachycardic. n Breathing pattern became shallow and bradypneic. n Level of responsiveness quickly decreased. 1 8/26/14 Case Description o Vasopressin and epinephrine boluses given. o Trachea intubated. Intra- arterial BP monitoring & central venous access established. § Vasopressin & epinephrine infusions started. o Diffuse blanching erythema noted. n No mucosal edema or wheezing. Case Description o Procedure cancelled. n Transported to medical ICU. n Weaned off vasopressors & extubated in 3 hours. n Serum tryptase 125 mcg/L (reference range 0.4 – 10.9). o Skin testing to bupivacaine: n No cutaneous, gastrointestinal, cardiovascular or respiratory symptoms. n No evidence of IgE-mediated hypersensitivity to bupivacaine. Discussion o Initial working diagnosis was a high or total spinal. o Tachycardia, skin changes and markedly elevated tryptase most consistent with anaphylactic reaction. -

Cognitive Behaviour Therapy (CBT) and Stroke Rehabilitation
Cognitive Behaviour Therapy (CBT) and Stroke Rehabilitation Amy Quilty OT Reg. (Ont.), Occupational Therapist Cognitive Behavioural Therapy (CBT) Certificate Program, University of Toronto Quinte Health Care: [email protected] Learning Objectives • To understand that CBT: • has common ground with neuroscience • principles are consistent with stroke best practices • treats barriers to stroke recovery • is an opportunity to optimize stroke recovery Question? Why do humans dominate Earth? The power of THOUGHT • Adaptive • Functional behaviours • Health and well-being • Maladaptive • Dysfunctional behaviours • Emotional difficulties Emotional difficulties post-stroke • “PSD is a common sequelae of stroke. The occurrence of PSD has been reported as high as 30–60% of patients who have experienced a stroke within the first year after onset” Canadian Stroke Best Practice Recommendations: Mood, Cognition and Fatigue Following Stroke practice guidelines, update 2015 http://onlinelibrary.wiley.com/doi/10.1111/ijs.12557/full • Australian rates: (Kneeborne, 2015) • Depression ~31% • Anxiety ~18% - 25% • Post Traumatic Stress ~10% - 30% • Emotional difficulties post-stroke have a negative impact on rehabilitation outcomes. Emotional difficulties post-stroke: PSD • Post stroke depression (PSD) is associated with: • Increased utilization of hospital services • Reduced participation in rehabilitation • Maladaptive thoughts • Increased physical impairment • Increased mortality Negative thoughts & depression • Negative thought associated with depression has been linked to greater mortality at 12-24 months post-stroke Nursing Best Practice Guideline from RNAO Stroke Assessment Across the Continuum of Care June : http://rnao.ca/sites/rnao- ca/files/Stroke_with_merged_supplement_sticker_2012.pdf Cognitive Behavioral Therapy (CBT) https://www.youtube.com/watch?v=0ViaCs0k2jM Cognitive Behavioral Therapy - CBT A Framework to Support CBT for Emotional Disorder After Stroke* *Figure 2, Framework for CBT after stroke. -

Autonomic Hyperreflexia Associated with Recurrent Cardiac Arrest
Spinal Cord (1997) 35, 256 ± 257 1997 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/97 $12.00 Autonomic hyperre¯exia associated with recurrent cardiac arrest: Case Report SC Colachis, III1 and DM Clinchot2 1Associate Professor and 2Assistant Professor, Department of Physical Medicine and Rehabilitation1, Director, SCI Rehabilitation, The Ohio State University, College of Medicine, Columbus, Ohio, USA Autonomic hyperre¯exia is a condition which may occur in individuals with spinal cord injuries above the splanchnic sympathetic out¯ow. Noxious stimuli can produce profound alterations in sympathetic pilomotor, sudomotor, and vasomotor activity, as well as disturbances in cardiac rhythm. A case of autonomic hyperre¯exia in a patient with C6 tetraplegia with recurrent ventricular ®brillation and cardiac arrest illustrates the profound eects of massive paroxysmal sympathetic activity associated with this condition. Keywords: autonomic hyperre¯exia; spinal cord injury; ventricular ®brillation Introduction Autonomic hyperre¯exia is a condition of paroxysmal by excessive sweating and ¯ushing. Past episodes of re¯ex sympathetic activity which occurs in response to autonomic hyperre¯exia were generally attributed to noxious stimuli in patients with spinal cord injuries re¯ex voiding, position changes and the presence of above the major splanchnic sympathetic out¯ow.1±3 pressure sores. The heightened sympathetic activity during an episode The attendant had completed the patient's morning of autonomic hyperre¯exia accounts for several of the bowel program, hygiene and dressing activities, and clinical features commonly observed including sudo- started to exit the apartment when he heard gasping. motor and pilomotor phenomenon,1,4 ± 6 vasomotor He returned to ®nd him pulseless, apneic, and sequelae,1 ± 4,7 and alterations in cardiac inotropic and cyanotic. -

What Is the Autonomic Nervous System?
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.suppl_3.iii31 on 21 August 2003. Downloaded from AUTONOMIC DISEASES: CLINICAL FEATURES AND LABORATORY EVALUATION *iii31 Christopher J Mathias J Neurol Neurosurg Psychiatry 2003;74(Suppl III):iii31–iii41 he autonomic nervous system has a craniosacral parasympathetic and a thoracolumbar sym- pathetic pathway (fig 1) and supplies every organ in the body. It influences localised organ Tfunction and also integrated processes that control vital functions such as arterial blood pres- sure and body temperature. There are specific neurotransmitters in each system that influence ganglionic and post-ganglionic function (fig 2). The symptoms and signs of autonomic disease cover a wide spectrum (table 1) that vary depending upon the aetiology (tables 2 and 3). In some they are localised (table 4). Autonomic dis- ease can result in underactivity or overactivity. Sympathetic adrenergic failure causes orthostatic (postural) hypotension and in the male ejaculatory failure, while sympathetic cholinergic failure results in anhidrosis; parasympathetic failure causes dilated pupils, a fixed heart rate, a sluggish urinary bladder, an atonic large bowel and, in the male, erectile failure. With autonomic hyperac- tivity, the reverse occurs. In some disorders, particularly in neurally mediated syncope, there may be a combination of effects, with bradycardia caused by parasympathetic activity and hypotension resulting from withdrawal of sympathetic activity. The history is of particular importance in the consideration and recognition of autonomic disease, and in separating dysfunction that may result from non-autonomic disorders. CLINICAL FEATURES c copyright. General aspects Autonomic disease may present at any age group; at birth in familial dysautonomia (Riley-Day syndrome), in teenage years in vasovagal syncope, and between the ages of 30–50 years in familial amyloid polyneuropathy (FAP). -

39 Voiding Dysfunction in Patients with Dysautonomia
39 Shridharani A1, Guralnick M1, Barboi A1, Jaradeh S1, Prieto T1, Yellick M1, O'Connor R C1 1. Medical College of Wisconsin VOIDING DYSFUNCTION IN PATIENTS WITH DYSAUTONOMIA Hypothesis / aims of study Dysautonomia, or autonomic dysfunction, is a primary neurologic condition resulting from failure of the sympathetic or parasympathetic nervous systems. The disorder has a myriad of clinical presentations including dysregulation of body temperature, orthostatic intolerance, gastrointestinal motility disorders and chronic pain syndromes. Urologically, while sexual dysfunction has been recognized as part of the autonomic dysfunction spectrum, voiding symptoms have been inadequately characterized. We present the chief urologic complaints, results of urodynamic studies and treatments of patients with a known history of dysautonomia referred to our neuro-urology clinic. Study design, materials and methods Retrospective chart review was performed on all patients seen between 2003 and 2008 in the neuro-urology clinic for voiding dysfunction with the concomitant diagnosis of dysautonomia. Patients with other neurologic diagnoses, such a multiple sclerosis or a history of spinal surgery, were excluded from the analysis. All patients underwent focused history and physical examination as well as video urodynamic studies. Upper tract imaging by renal ultrasound or computerized tomography of the abdomen/pelvis was performed on select patients. Treatment modalities that subjectively and objectively improved the patient’s symptoms were recorded. Objective improvements were measured via post void residual bladder volume, uroflowmetry and/or urodynamic studies. Results Of 443 patients with the diagnosis of dysautonomia, 37 (8%) were referred for evaluation of voiding dysfunction. Mean age was 47 years (range 12 - 80) and 31/37 (84%) patients were female. -
Neuromuscular Weakness in The
Neuromuscular Disorders in the Intensive Care Unit -when and how M. S. Damian, Addenbrookes Hospital, Cambridge Background to this talk? • Neuromuscular admissions to the ICU are increasing • The incidence of individual conditions is not clear • The true outcomes of these patients are unclear • Mortality rates in patients treated with Myasthenia and Guillain Barre Syndrome have not significantly improved in the last 20 years, neither have treatments [Damian MS, Howard R, Int Care Med 2013] • Bad medicine is expensive (Example: An MG case with recurrent crises. 1 year pre-Rituximab: £39,810 costs incl. 14d ICU stay 1 year on Rituximab: ca. £8,000 total costs, no ICU stay M. S. Damian, Addenbrookes Hospital, Cambridge Which neuromuscular symptoms may require treatment in the ICU? • Severe respiratory weakness • Bulbar weakness and aspiration • Cardiomyopathy and heart failure • Arrhythmia • Dysautonomia • Acute rhabdomyolysis and renal failure M. S. Damian, Addenbrookes Hospital, Cambridge 3 main groups of patients with neuromuscular disease may require treatment in the ICU I. Patients with severe new onset of neuromuscular disease II. Patients with pre-existing chronic neuromuscular conditions who develop acute complications III. Patients whose neuromuscular disorder arises in the ICU M. S. Damian, Addenbrookes Hospital, Cambridge Severe new onset neuromuscular disease in the ICU • Guillain Barre Syndrome • Severe acute neuropathy • Acute flaccid paralysis syndrome (WNV, enterovirus 71- mostly with encephalitis) • Myasthenic crisis and -

REVIEW Autonomic Assessment of Animals with Spinal Cord
Spinal Cord (2009) 47, 2–35 & 2009 International Spinal Cord Society All rights reserved 1362-4393/09 $32.00 www.nature.com/sc REVIEW Autonomic assessment of animals with spinal cord injury: tools, techniques and translation JA Inskip1,2,4, LM Ramer1,2,4, MS Ramer1,2 and AV Krassioukov1,3 1International Collaboration on Repair Discoveries, University of British Columbia, Vancouver, British Columbia, Canada; 2Department of Zoology, University of British Columbia, Vancouver, British Columbia, Canada and 3Department of Medicine, Division of Physical Medicine and Rehabilitation, University of British Columbia, Vancouver, British Columbia, Canada Study design: Literature review. Objectives: To present a comprehensive overview of autonomic assessment in experimental spinal cord injury (SCI). Methods: A systematic literature review was conducted using PubMed to extract studies that incorporated functional motor, sensory or autonomic assessment after experimental SCI. Results: While the total number of studies assessing functional outcomes of experimental SCI increased dramatically over the past 27 years, studies with motor outcomes dramatically outnumber those with autonomic outcomes. Within the areas of autonomic dysfunction (cardiovascular, respiratory, gastrointestinal, lower urinary tract, sexual function and thermoregulation), not all aspects have been characterized to the same extent. Studies focusing on bladder and cardiovascular function greatly outnumber those on sexual function, gastrointestinal function and thermoregulation. This review addresses the disparity between well-established motor-sensory testing presently used in experimental animals and the lack of standardized autonomic testing following experimental SCI. Throughout the review, we provide information on the correlation between existing experimental and clinically used autonomic tests. Finally, the review contains a comprehensive set of tables and illustrations to guide the reader through the complexity of autonomic assessment and dysfunctions observed following SCI.