Diseases of Motor Neuron and Skeletal Muscle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Spinraza™ (Nusinersen)
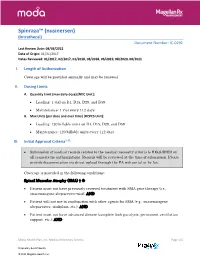
Spinraza™ (nusinersen) (Intrathecal) Document Number: IC-0291 Last Review Date: 08/03/2021 Date of Origin: 01/31/2017 Dates Reviewed: 01/2017, 02/2017, 01/2018, 08/2018, 06/2019, 08/2020, 08/2021 I. Length of Authorization Coverage will be provided annually and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Loading: 1 vial on D1, D15, D29, and D59 • Maintenance: 1 vial every 112 days B. Max Units (per dose and over time) [HCPCS Unit]: • Loading: 120 billable units on D1, D15, D29, and D59 • Maintenance: 120 billable units every 112 days III. Initial Approval Criteria1-12 • Submission of medical records related to the medical necessity criteria is REQUIRED on all requests for authorizations. Records will be reviewed at the time of submission. Please provide documentation via direct upload through the PA web portal or by fax. Coverage is provided in the following conditions: Spinal Muscular Atrophy (SMA) † Ф • Patient must not have previously received treatment with SMA gene therapy (i.e., onasemnogene abeparvovec-xioi); AND • Patient will not use in combination with other agents for SMA (e.g., onasemnogene abeparvovec, risdiplam, etc.); AND • Patient must not have advanced disease (complete limb paralysis, permanent ventilation support, etc.); AND Moda Health Plan, Inc. Medical Necessity Criteria Page 1/5 Proprietary & Confidential © 2021 Magellan Health, Inc. • Patient must have the following laboratory tests at baseline and prior to each administration*: platelet count, prothrombin time; activated -

2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make Every Day Count at PTC, Patients Are at the Center of Everything We Do
20 YEARS OF COMMITMENT 2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make every day count At PTC, patients are at the center of everything we do. We have the opportunity to support patients and families living with rare disorders through their journey. We know that every day matters and we are committed to making a difference. OUR SCIENCE Our scientists are finding new ways to regulate biology to control disease We have several scientific research platforms focused on modulating protein expression within the cell that we believe have the potential to address many rare genetic disorders. OUR PEOPLE Care for each other, our community, and for the needs of our patients At PTC, we are looking at drug discovery and development in a whole new light, bringing new technologies and approaches to developing medicines for patients living with rare disorders and cancer. We strive every day to be better than we were the day before. At PTC Therapeutics, it is our mission to provide access to best-in-class treatments for patients who have an unmet need. We are a science-led, global biopharmaceutical company focused on the discovery, development and commercialization of clinically-differentiated medicines that provide benefits to patients with rare disorders. Founded 20 years ago, PTC Therapeutics has successfully launched two rare disorder products and has a global commercial footprint. This success is the foundation that drives investment in a robust pipeline of transformative medicines and our mission to provide access to best-in-class treatments for patients who have an unmet medical need. As we celebrate our 20th year of bringing innovative therapies to patients affected by rare disorders, we reflect on our unwavering commitment to our patients, our science and our employees. -

Spinraza® (Nusinersen)
UnitedHealthcare® Commercial Medical Benefit Drug Policy Spinraza® (Nusinersen) Policy Number: 2021D0059I Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Community Plan Policy Coverage Rationale ....................................................................... 1 • Spinraza® (Nusinersen) Documentation Requirements ...................................................... 3 Applicable Codes .......................................................................... 3 Background.................................................................................... 4 Benefit Considerations .................................................................. 5 Clinical Evidence ........................................................................... 5 U.S. Food and Drug Administration ............................................. 8 References ..................................................................................... 9 Policy History/Revision Information ........................................... 10 Instructions for Use ..................................................................... 11 Coverage Rationale See Benefit Considerations Spinraza® (nusinersen) is proven and medically necessary for the treatment of spinal muscular atrophy (SMA) in patients who meet all of the following criteria: 1-4,22,23 Initial Therapy Diagnosis of spinal muscular atrophy by, or in consultation with, a neurologist with expertise in the diagnosis of SMA; and Submission of medical records (e.g., chart notes, laboratory values) -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

New Brunswick Drug Plans Formulary
New Brunswick Drug Plans Formulary August 2019 Administered by Medavie Blue Cross on Behalf of the Government of New Brunswick TABLE OF CONTENTS Page Introduction.............................................................................................................................................I New Brunswick Drug Plans....................................................................................................................II Exclusions............................................................................................................................................IV Legend..................................................................................................................................................V Anatomical Therapeutic Chemical (ATC) Classification of Drugs A Alimentary Tract and Metabolism 1 B Blood and Blood Forming Organs 23 C Cardiovascular System 31 D Dermatologicals 81 G Genito Urinary System and Sex Hormones 89 H Systemic Hormonal Preparations excluding Sex Hormones 100 J Antiinfectives for Systemic Use 107 L Antineoplastic and Immunomodulating Agents 129 M Musculo-Skeletal System 147 N Nervous System 156 P Antiparasitic Products, Insecticides and Repellants 223 R Respiratory System 225 S Sensory Organs 234 V Various 240 Appendices I-A Abbreviations of Dosage forms.....................................................................A - 1 I-B Abbreviations of Routes................................................................................A - 4 I-C Abbreviations of Units...................................................................................A -

Circulating Biomarkers in Neuromuscular Disorders: What Is Known, What Is New
biomolecules Review Circulating Biomarkers in Neuromuscular Disorders: What Is Known, What Is New Andrea Barp 1,* , Amanda Ferrero 1, Silvia Casagrande 1,2 , Roberta Morini 1 and Riccardo Zuccarino 1 1 NeuroMuscular Omnicentre (NeMO) Trento, Villa Rosa Hospital, Via Spolverine 84, 38057 Pergine Valsugana, Italy; [email protected] (A.F.); [email protected] (S.C.); [email protected] (R.M.); [email protected] (R.Z.) 2 Department of Neurosciences, Drug and Child Health, University of Florence, Largo Brambilla 3, 50134 Florence, Italy * Correspondence: [email protected] Abstract: The urgent need for new therapies for some devastating neuromuscular diseases (NMDs), such as Duchenne muscular dystrophy or amyotrophic lateral sclerosis, has led to an intense search for new potential biomarkers. Biomarkers can be classified based on their clinical value into different categories: diagnostic biomarkers confirm the presence of a specific disease, prognostic biomarkers provide information about disease course, and therapeutic biomarkers are designed to predict or measure treatment response. Circulating biomarkers, as opposed to instrumental/invasive ones (e.g., muscle MRI or nerve ultrasound, muscle or nerve biopsy), are generally easier to access and less “time-consuming”. In addition to well-known creatine kinase, other promising molecules seem to be candidate biomarkers to improve the diagnosis, prognosis and prediction of therapeutic response, such as antibodies, neurofilaments, and microRNAs. However, there are some criticalities that can complicate their application: variability during the day, stability, and reliable performance metrics Citation: Barp, A.; Ferrero, A.; (e.g., accuracy, precision and reproducibility) across laboratories. In the present review, we discuss Casagrande, S.; Morini, R.; Zuccarino, the application of biochemical biomarkers (both validated and emerging) in the most common NMDs R. -

Refreshing the Biologic Pipeline 2020
news feature Credit: Science Lab / Alamy Stock Photo Refreshing the biologic pipeline 2020 In the absence of face-to-face meetings, FDA and industry implemented regulatory workarounds to maintain drug and biologics approvals. These could be here to stay. John Hodgson OVID-19 might have been expected since 1996) — a small miracle in itself “COVID-19 confronted us with the need to severely impair drug approvals (Fig. 1 and Table 1). to better triage sponsors’ questions,” says Cin 2020. In the event, however, To the usual crop of rare disease and Peter Marks, the director of the Center for industry and regulators delivered a small genetic-niche cancer treatments, 2020 Biologics Evaluation and Research (CBER) miracle. They found workarounds and also added a chimeric antigen receptor at the FDA. “That was perhaps the single surrogate methods of engagement. Starting (CAR)-T cell therapy with a cleaner biggest takeaway from the pandemic related in January 2020, when the outbreak veered manufacturing process and the first to product applications.” Marks says that it westward, the number of face-to face approved blockbuster indication for a became very apparent with some COVID- meetings declined rapidly; by March, small-interfering RNA (siRNA) — the 19-related files that resolving a single they were replaced by Webex and Teams. European Medicines Agency’s (EMA) issue can help a sponsor enormously and (Secure Zoom meeting are to be added registration of the RNA interference accelerate the development cycle. Before this year.) And remarkably, by 31 December, (RNAi) therapy Leqvio (inclisiran) for COVID-19, it was conceivable that a small the US Food and Drug Administration cardiovascular disease. -

NHS England Risdiplam EAMS Framework
FRAMEWORK OF ADVICE ON THE RISDIPLAM EARLY ACCESS TO MEDICINES SCHEME Background On 17 September 2020, Risdiplam was made available via the Early Access to Medicines Scheme (EAMS), details of which can be found at: https://www.gov.uk/government/publications/risdiplam-in-the-treatment-of-type-1- and-type-2-spinal-muscular-atrophy-sma-in-patients-2-months-of-age-and-older The EAMS scientific opinion issued to Roche Products Limited is for Risdiplam 0.75 mg/ml powder for oral solution in the treatment of type 1 and type 2 Spinal Muscular Atrophy (SMA) in patients 2 months and older who are not suitable for authorised treatments. The questions in the NHS England Blueteq form are attached for reference at Appendix A. The NHS England Nusinersen Clinical Panel, which is also established to offer advice more generally on the treatment and care of patients with spinal muscular atrophy, was asked to develop a framework of advice for clinicians to assist in interpreting the EAMS scientific opinion. The information below is a framework of advice for clinicians to assist in interpreting the EAMS scientific opinion and is not a directive from NHS England. The Clinical Panel understands that each patient case has unique factors and the treating physician must acknowledge that the patient fits the EAMS indication of not suitable for authorised treatments. This is in the context of nusinersen being available to eligible patients through a managed access agreement and onasemnogene abeparvovec being evaluated by NICE. The Clinical Panel is also able to offer advice on individual cases. -

Rxoutlook® 1St Quarter 2019
® RxOutlook 1st Quarter 2020 optum.com/optumrx a RxOutlook 1st Quarter 2020 Orphan drugs continue to feature prominently in the drug development pipeline In 1983 the Orphan Drug Act was signed into law. Thirty seven years later, what was initially envisioned as a minor category of drugs has become a major part of the drug development pipeline. The Orphan Drug Act was passed by the United States Congress in 1983 in order to spur drug development for rare conditions with high unmet need. The legislation provided financial incentives to manufacturers if they could demonstrate that the target population for their drug consisted of fewer than 200,000 persons in the United States, or that there was no reasonable expectation that commercial sales would be sufficient to recoup the developmental costs associated with the drug. These “Orphan Drug” approvals have become increasingly common over the last two decades. In 2000, two of the 27 (7%) new drugs approved by the FDA had Orphan Designation, whereas in 2019, 20 of the 48 new drugs (42%) approved by the FDA had Orphan Designation. Since the passage of the Orphan Drug Act, 37 years ago, additional regulations and FDA designations have been implemented in an attempt to further expedite drug development for certain serious and life threatening conditions. Drugs with a Fast Track designation can use Phase 2 clinical trials to support FDA approval. Drugs with Breakthrough Therapy designation can use alternative clinical trial designs instead of the traditional randomized, double-blind, placebo-controlled trial. Additionally, drugs may be approved via the Accelerated Approval pathway using surrogate endpoints in clinical trials rather than clinical outcomes. -

CP.PHAR.477 Risdiplam (Evrysdi)
Clinical Policy: Risdiplam (Evrysdi) Reference Number: CP.PHAR.477 Effective Date: 08.07.20 Last Review Date: 08.20 Line of Business: Commercial, HIM, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Risdiplam (Evrysdi™) is a survival motor neuron 2 (SMN2) gene pre-mRNA splicing modifier. FDA Approved Indication(s) Evrysdi is indicated for the treatment of spinal muscular atrophy (SMA) in patients 2 months of age and older. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Evrysdi is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Spinal Muscular Atrophy (must meet all): 1. Diagnosis of SMA with documentation of both of the following (a and b): a. Genetic testing quantifying number of copies of SMN2 gene ≥ 1 but ≤ 4; b. Member is symptomatic; 2. Genetic testing confirms the presence of one of the following (a, b, or c): a. Homozygous deletions of SMN1 gene (e.g., absence of the SMN1 gene); b. Homozygous mutation in the SMN1 gene (e.g., biallelic mutations of exon 7); c. Compound heterozygous mutation in the SMN1 gene [e.g., deletion of SMN1 exon 7 (allele 1) and mutation of SMN1 (allele 2)]; 3. Prescribed by or in consultation with a neurologist; 4. Age ≥ 2 months; 5. Documentation of one of the following baseline scores (see Appendix D) (a or b): a. -

Corporate Medical Policy
Corporate Medical Policy Nusinersen (Spinraza™) File Name: nusinersen_spinraza Origination: 03/2017 Last CAP Review: 10/2020 Next CAP Review: 10/2021 Last Review: 10/2020 Description of Procedure or Service Spinal muscular atrophy (SMA) is an inherited disorder caused by homozygous deletions or variants in the SMN1 gene. As a consequence of low levels of SMN1 protein, the motor neurons in spinal cord degenerate, resulting in atrophy of the voluntary muscles of the limbs and trunk. Nusinersen is a synthetic antisense oligonucleotide designed to bind to a specific sequence in exon 7 of the SMN2 transcript causing the inclusion of exon 7 in the SMN2 transcript, leading to production of full length functional SMN2 protein, which demonstrates similarity to SMN1. SPINAL MUSCULAR ATROPHY Spinal muscular atrophy (SMA) is a rare autosomal recessive genetic disorder caused by homozygous deletions or variants in the SMN1 gene in chromosome 5. This gene is responsible for producing the “survival of motor neuron” protein (SMN1). As a consequence of absent or low levels of this protein, the motoneurons in the spinal cord degenerate, resulting in atrophy of the voluntary muscles of the limbs and trunk. During early development, these muscles are necessary for crawling, walking, sitting up, and head control. The more severe types of SMA can also affect muscles involved in feeding, swallowing, and breathing. The exact role of the SMN protein in motoneurons has not been completely elucidated and levels of the SMN protein required for optimal functioning are unknown. SMN2 is a nearly identical modifying gene capable of producing compensatory SMN protein. -

Innovationsreport 2020 Kurzfassung
Innovationsreport 2020 Auswertungsergebnisse von Routinedaten der Techniker Krankenkasse aus den Jahren 2017 bis 2018 Herausgeber: Gerd Glaeske Erstellt mit freundlicher Unterstützung der Techniker Krankenkasse (TK) 3 Herausgeber Prof. Dr. Gerd Glaeske Experten für ausgewählte Kapitel Prof. Dr. med. Janbernd Kirschner, Bonn Prof. Dr. med. Dieter Ukena, Bremen Prof. Dr. med. Barbara Schmalfeldt, Hamburg Prof. Dr. med. Wolfgang Schramm, München Autoren Prof. Dr. med. Karl Broich, Dr. Stanislava Dicheva‐Radev, Dörte Fuchs, Prof. Dr. Gerd Glaeske, Dr. Marion Haberkamp, Dr. Iris Hinneburg, Friederike Höfel, Prof. Dr. Janbernd Kirschner, Dr. Wiebke Löbker, Anja Lübs, Dr. André S. Morawetz, Lutz Muth, Dr. Frauke Naumann‐Winter, Linda Richter, Saskia Ritter, Dr. Kristin Sauer, Dr. Birgit Schindler unter Mitarbeit von Esra Aksoy, Friederike Höfel, Berit Marquardt, Linda Richter, Marle Wilhelm Anschrift: Universität Bremen, SOCIUM, Mary‐Somerville‐Str. 5, 28359 Bremen Aus Gründen der besseren Lesbarkeit wurde auf die Nennung beider geschlechtsspezifischer Formen verzichtet. Im Allgemeinen ist aber das jeweils andere Geschlecht ebenfalls gemeint. 2 Glossar .......................................................................................... 7 Vorwort zum Innovationsreport 2020 ...........................................15 Vorwort des Herausgebers ............................................................17 1 Einleitung ................................................................................19 2 Ziele und Methodik..................................................................33