2016 Message from the Dean
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

I. Council Roll Call A. 17 Councils in Attendance II. Special Guests A
GENERAL ASSEMBLY MINUTES FOR MEETING OF NOVEMBER 21, 2019 I. Council Roll Call A. 17 Councils in Attendance II. Special Guests A. Kate Lower, SHIFT Director i. Interested in joining the SHIFT Student Advisory Board? Email [email protected] to learn more. III. Special Reports IV. Organizational Announcements A. Habitat for Humanity UT Campus Chapter: Adhrit Srivastav ([email protected]) i. Act! Speak! Build! Week ● Events on the Horizon: a. Holiday Craft Night | December 5 i. PCL Learning Lab #1 - 6-8 PM ii. Destress by drinking hot chocolate and making some crafts for Habitat homeowners in our community b. Advocacy Open Forum | December 6 i. WCH 1.120 - 7-8 PM ii. Learn and ask about current campaigns against gentrification in ATX from guest speakers c. 2019 Blitz Build | December 7 i. 7025 Zachary Drive - 8 AM - 4 PM ii. Volunteer to help build houses at a construction site. Must be an active UT Habitat Member to sign-up. ii. Contact Information: ● Email: [email protected] ● Instagram: @utexashabitat ● Facebook: UT Habitat for Humanity V. Regular Guests A. The Office of the Dean of Students: Marcus Mayes ([email protected]) B. Student Government: Camron Goodman ([email protected]) i. Michael Pontikes ([email protected]) ● A.R. 6 In support of the creation of a non-traditional student center on campus ● A.B. 6 In Support of defining focus of Student Government ● J.R. 19-01 Passed through SG ● J.R. 19-04 Passed through SG ● J.R. 19-03, really redo the bill C. Graduate Student Assembly: Christina Baze ([email protected]) i. -

Beta Mu Review PI KAPPA ALPHA • UNIVERSITY of TEXAS • FALL 2016
THE BETA MU REVIEW PI KAPPA ALPHA • UNIVERSITY OF TEXAS • FALL 2016 Beta Mu Receives Orians Award for Third Consecutive Year Academics and Alumni Relations Priorities he Texas Pikes are concluding a great fall T2016 focused on academics, philanthropy, athletics and brotherhood. We have had a great time connecting with many alumni and their families this semester at various events recapped in this newsletter. We were pleased to initiate 34 new members in December. Meet these new brothers on page 7. Awards Abound at Above: Peggy and John Rathmell ’76 and Anne and Meade Bauer ’78 enjoyed being together National Convention at the Texas-Oklahoma game in October. Beta Mu received a number of awards at Pike’s 2016 National Convention in New Orleans. For Left: Pike freshman new members Cole Martinez, the third successive year, Beta Mu received the Arthur Gorling, and Landon Hackley enjoyed Raymond L. Orians Chapter Excellence Award. meeting U.T. President Greg Fenves at a The Orians Award is given to only 20 chapters, campus reception in September. signifying Pike’s highest performing chapters. Our men also received the Best Alumni Relations Program Award, the Scholarship Award, the 100 Active in Academics Man Chapter Award and an award for commit- and Philanthropy ment to Pike University. The Beta Mu Alumni Academics remain a priority at the Pike house. Advisory Board was also selected for the third The overall Pike membership GPA is 3.2 per year running as one of the top 20 operating the University’s most recent semester rankings, alumni boards in the fraternity. -

ASH Brain Health System Redesign Communications Strategy Plan
10/22/18 ASH Brain Health System Redesign Communications Strategy Plan, version 4.0 1 10/22/18 Executive Summary The Design Institute for Health, in collaboration with the Communications Subcommittee, has prepared a Communications Strategy Plan for the preplannning and planning phases of the ASH Brain Health System Redesign. The plan identifies seven communications objectives and two core audience segments: internal and external. The internal audience focuses on project leadership and their networks. The external audience segment prioritizes five groups for these early phases: public officials, law enforcement, professional organizations and associations, mental health justice system, and media. Three core communications strategies are idenitifed to reach the audiences and meet the objectives using modern methodologies. A digital toolbox will serve to align the internal audience. For the external audience, a set of outreach opportunities coupled with an online final report are designed to inform the five key audiences across the large service area. Next steps are to build and launch the components in November and December 2018. The plan includes the current version (4.0) of approved initial messages and FAQ’s which will continue to be updated. 2 10/22/18 Introduction One in five Texans – more than five million people – experience a mental health condition each year, requiring increasing investment by Texas to help to address these conditions and improve the lives of its citizens. As part of that response, the Texas Legislature invested $300 million during the last legislative session for improvements to the state’s psychiatric hospitals. The Texas Health and Human Services Commission (HHSC) contracted with Dell Medical School at the University of Texas at Austin (Dell Med) to lead a collaborative, $15.5 million preplanning and planning phases of redesigning the Austin State Hospital (ASH) that serves 38 counties for adults, 57 counties for adolescents, and 75 counties for children. -

Quarterly Update Summary - 5/15/14 Austin 102-282 Redesignate Project to Welch Hall Renovation Phase 2 - Robert A
FY 2014-2019 Capital Improvement Program Quarterly Update Summary - 5/15/14 Austin 102-282 Redesignate project to Welch Hall Renovation Phase 2 - Robert A. Welch Hall Phase 2 (AVC Memo) 102-556 Approve an increase in Total Project Cost from Engineering Education and Research $310,000,000 to $311,600,000 with $1,600,000 from Center Available University Funds. (Chancellor Memo) 102-772 Approve an increase in Total Project Cost from Dell Medical School - Phase I $334,500,000 to $341,261,000 with $6,761,000 from RFS. (Chancellor Memo) 102-777 Approve an increase in Total Project Cost from Renovate Moore Hill Dormitory $8,000,000 to $8,800,000 with $800,000 additional funding from DHFS Auxiliary Enterprises Balances (President Memo) 102-719 Approve Design Development and increase in Total Robert B. Rowling Hall Project Cost from $155,000,000 to $176,300,000 with funding of $113,050,000 from RFS, $42,450,000 from Gifts, $15,800,000 from Unexpended Plant Funds and $5,000,000 from Auxiliary Enterprises Balances (BOR 5/15/14) 102-783 Approve a decrease in Total Project Cost from Medical District Utility System $96,000,000 to $87,589,000 with $8,411,000 from Infrastructure RFS. (Chancellor Memo) 102-788 Approve Design Development with Total Project Tennis Center Replacement Facility Cost of $15,000,000 with funding from Auxiliary Enterprises Balances (BOR 5/15/14) Dallas 302-828 Approve design development documents and Campus Upgrades and Renovations authorize expenditure of funds (President Memo) 302-842 Add project to CIP with Total Project Cost -
Legislative Appropriations Request the University of Texas at Austin
L EGISLATIVE A PPROPRIATIONS R EQUEST F I S C A L Y EAR S 2020 A N D 2021 Submitted to the Governor’s Office A nd the Legislative Budget Board T H E U NIVERSITY OF T E X A S A T A USTIN A u g u s t 2 0 1 8 TABLE OF CONTENTS I. SCHEDULES NOT INCLUDED ........................................................................................................................................................................................................................ 1 1. ADMINISTRATOR’S STATEMENT ................................................................................................................................................................................................................ 2 A. ORGANIZATIONAL CHART ................................................................................................................................................................................................................................... 9 B. DESCRIPTION OF FUNCTIONAL UNITS ................................................................................................................................................................................................................ 10 C. BUDGET OVERVIEW – BIENNIAL AMOUNTS....................................................................................................................................................................................................... 12 2. SUMMARIES OF REQUEST A. SUMMARY OF BASE REQUEST BY STRATEGY .................................................................................................................................................................................................... -
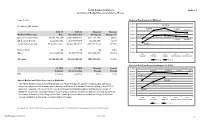
Section 1 Health Related Institutions Summary of Budget
Health Related Institutions Section 1 Summary of Budget Recommendations - House Page III-168 Historical Funding Levels (Millions) $1,800.0 Colin Brock, LBB Analyst $1,736.9 $1,750.0 $1,707.6 $1,680.3 $1,674.3 2020-21 2022-23 Biennial Biennial $1,700.0 Method of Financing Base Recommended Change ($) Change (%) $1,650.0 $1,592.0 $1,633.0 $1,641.5 General Revenue Funds $3,052,133,697 $3,028,007,561 ($24,126,136) (0.8%) $1,600.0 $1,626.0 $1,619.9 GR Dedicated Funds $222,341,504 $217,875,808 ($4,465,696) (2.0%) $1,550.0 Total GR-Related Funds $3,274,475,201 $3,245,883,369 ($28,591,832) (0.9%) $1,538.1 $1,500.0 $1,450.0 Federal Funds $0 $0 $0 0.0% Other $169,987,790 $108,757,199 ($61,230,591) (36.0%) $1,400.0 2019 2020 2021 2022 2023 Expended Estimated Budgeted Recommended Recommended All Funds $3,444,462,991 $3,354,640,568 ($89,822,423) (2.6%) All Funds GR/GR-D Historical Full-Time-Equivalent Employees (FTEs) FY 2021 FY 2023 Biennial Percent 14,000.0 13,720.8 13,630.6 Budgeted Recommended Change Change 13,800.0 13,715.3 13,630.6 FTEs 13,318.4 13,630.6 312.2 2.3% 13,600.0 13,400.0 13,084.9 13,200.0 13,318.4 Agency Budget and Policy Issues and/or Highlights 13,000.0 12,800.0 The Health Related Institutions (HRIs) Summary of Recommendations packet includes budget and policy 12,949.5 recommendations for the thirteen Health Related Institutions that received formula funding in the 2020-21 12,600.0 12,400.0 biennium, including The University of Texas (UT) at Austin Dell Medical School and the Baylor College of 12,462.7 Medicine. -

The University of Texas at Austin Response to House Higher Education Committee Formal Request for Information COVID-19 Interim Charge
The University of Texas at Austin Response to House Higher Education Committee Formal Request for Information COVID-19 Interim Charge 1. Are institutions of higher education ensuring the health and safety of students, faculty, and staff during the 2020 Fall Semester? When applicable, please speak directly to classroom and lab setting, dormitories, and dining halls. The health of our students, faculty, staff, and visitors remains at the forefront of all planning for the fall semester. In April, UT Austin established six workgroups to provide plans for a phased re- opening of the campus, covering Academics, Health and Wellness, Student Life, Operations, Research, and Athletics. The result of those extensive planning sessions, released in June, is the Protect Texas Together plan. While online learning will be critical to the continuity of education, the on-campus experience plays a central role in the university’s mission – even with the restrictions that the pandemic will place on campus life. As such, highlights of the plan include extensive online or hybrid online/in-person class offerings, wearing face coverings when inside buildings (except in a private office or personal dorm room, or while eating), strong hygiene practices, frequent building inspection and cleaning protocols, a request for students to self-quarantine for 14 days prior to arrival, and suggested daily symptom screenings through the Protect Texas Together smartphone app. Approximately 77% of classroom seats will be online this semester, and for those classes or labs with an in-person component, classrooms will be limited to 40% capacity and seating will be spread out according to social distancing guidelines. -
2020 Program Report
Joint Admission Medical Program 2020 Program Report Report to the Governor, Lieutenant Governor, and the Speaker of the House Pursuant to Chapter 51, Texas Education Code, Subchapter V, Section 51.834 Making the path to medical school a reality for Texans. Joint Admission Medical Program Table of Contents 4 What is JAMP? 6 JAMP Council Members 7 Message from Council Chair 8 Message from Executive Director 9 Enrollment Report 15 Featured JAMP Alumnus 16 Student Profiles 18 JAMP Physicians 26 COVID-19 Response from JAMP 27 Outreach Report 28 Faculty Director Profiles 29 Medical Schools Report 32 Financial Report 36 Audit Report 38 Program Modifications 3 What is JAMP? Joint Admission Medical Program The Joint Admission Medical Program (JAMP) is a JAMP students who meet all continuing eligibility special pipeline program established by the Texas criteria are guaranteed admission to one of the medical Legislature in 2001 to assist highly motivated, schools in Texas. Once admitted, JAMP continues to economically disadvantaged students in preparing for support the medical education of the student through and succeeding in medical school. Funded by the Texas scholarships and mentorship with other medical Legislature through a trusteed program administered at students and medical faculty. the Texas Higher Education Coordinating Board, JAMP constitutes a unique partnership between eleven Texas The program is administered through the Texas medical schools and seventy public and private four- Medical and Dental Schools Application Service year undergraduate institutions. (TMDSAS), housed at The University of Texas System Administration offices in Austin. Pursuant to Chapter The program provides scholarships, summer medical 51 of the Texas Education Code, JAMP is governed by enrichment internships and stipends, and MCAT a council of faculty representatives from each of the preparation programming for undergraduate students participating medical schools in Texas. -

Strategic Plan for Population Health Innovation and Improvement University of Texas at Austin
Strategic Plan for Population Health Innovation and Improvement University of Texas at Austin — Prepared by — Monique Vasquez Ethan D’Silva Jaionn Griner Jayne C. Nussbaum, MPA William M. Tierney, MD ——— Department of Population Health, Dell Medical School University of Texas at Austin January 27, 2017 1 | Page Table of Contents: Page Introduction 3 Section 1: Identified Catchment Area for the Health Institutions 3 Section 2: Compiled Data on Health of the Population and Health Disparities 5 Section 3: Community Needs and Priorities Assessment 14 Section 4: Identified Resources in the Community 19 Section 5: Identified Health Priorities 22 Section 6: Identified Availability and Gaps in Technology and Infrastructure 25 Section 7: Identified Availability and Gaps in the Health Institution 27 Section 8: Assessment of Additional Needs 31 Section 9: Plan and Strategy to Implement Population Health 32 Section 10: Environment and Impact Assessment 37 References 38 Appendix: Questions: University of Texas Faculty and Staff Population Health Survey 45 Appendix: Results: University of Texas Faculty and Staff Population Health Survey 47 Appendix: Questions for Key Informant CST Members 60 Appendix: Questions for CST Applicant Dinner and Discussion Forum 61 2 | Page INTRODUCTION In 2011, Texas Senator Kirk Watson proposed building a medical school from the ground up as part of a 10 year plan to improve the health of Austin and Travis County residents; this would be the first medical school built at a top tier research university in nearly 50 years.1 One year later, these residents voted for Proposition 1, committing $35 million annually from increased property taxes as investment in the school, with the promise of improved health outcomes. -

The University of Texas at Austing Dell Medical School, Austin, Texas
Accreditation Period: 2021-2022 THE UNIVERSITY OF TEXAS AT AUSTING DELL MEDICAL SCHOOL, AUSTIN, TEXAS MARIAN YVETTE WILLIAMS-BROWN, MD MICHAEL BREEN, MD Program Director Associate Program Director FACULTY Tomas Antonini, Alison Brooks, April Fox, George Macones, Winnie Mak, Michael Phillips, Christina Salazar, Emily Vinas, Amanda White 2-Year Program Optional Degrees: MPH MBA MS Other: None Number of Faculty GYN Faculty: 5 UROGYN Faculty: 2 REI Faculty: 1 ONCOLOGY Faculty: 1 GU Faculty: 0 General Surgery Faculty: 0 Colorectal Faculty: 1 Other: 2 Residency Program Affiliation: Yes No Computer Simulation Center: Yes No Training Labs Cadaver lab Animal Lab None Dry Lab Robotics Office Surgery: Yes No Contract/Agreement Letter: Yes No Stipend PGY-5 or 6: Yes No Resident Teaching Yes No Benefit Package: Yes No OB obligation: Yes No If yes, please describe obligation. Junior Faculty Yes No Attending Privileges Yes No Moonlighting: Yes No Non-compete clause: Yes No Malpractice: Yes No Meeting support: Yes No Malpractice tail coverage: Other coverage obligations- specify: Yes No Accept J1 Visa applicants Yes No Accept H1Visa applicants Yes No Dedicated Research Hours: Hours/per week: 35 *during dedicated 3 months research Hours/per month: 140 *during dedicated 3 months research Protected Academic: Hours/per week: 5 Hours/per month: 20 Clinical Focus/Special Interest Reproductive Surgery Oncology Endometriosis/Pelvic Pain Pelvic Reconstruction Robotic Surgery Pediatric/Adolescent Hysteroscopic Surgery Other: 1.4.2021 Description of Program: The overarching educational goals for the Dell Medical School Minimally Invasive Gynecologic Fellowship are to provide training to academic gynecologic surgeons in order to attain comprehensive knowledge of advanced gynecologic disorders and extensive surgical and clinical expertise focused on laparoscopic and robotic surgical techniques that leads to a board-approved focused practice designation, as well as the ability to contribute research to the field of minimally invasive gynecologic surgery. -

UTAUS Human Subject Research at Dell Medical School Report
Human Subject Research Dell Medical School November 2019 The University of Texas at Austin Office of Internal Audits UTA 2.302 (512) 471-7117 The University of Texas at Austin - Institutional Audit Committee, December 16, 2019 7-57 OFFICE OF INTERNAL AUDITS THE UNIVERSITY OF TEXAS AT AUSTIN 1616 Guadalupe St. Suite 2.302 · Austin, Texas 78701 · (512) 471-7117 · FAX (512) 471-8099 audit.utexas.edu • [email protected] November 27, 2019 President Gregory L. Fenves The University of Texas at Austin Office of the President P.O. Box T Austin, Texas 78713 Dear President Fenves, We have completed our audit of human subject research at Dell Medical School (Dell Med). This audit was part of our fiscal year 2019 Audit Plan. The objectives of the audit were to determine whether Principal Investigators (PIs) were obtaining key elements of the consent form from human subjects and whether PIs completed required training prior to receiving approval to perform research. The report is attached for your review. Overall, Dell Med researchers working in human subject research are obtaining consent from participants, and researchers completed their University of Texas at Austin (UT Austin) required training. Please let me know if you have questions or comments regarding this audit. Sincerely, Sandy Jansen, CIA, CCSA, CRMA Chief Audit Executive cc: Dr. S. Claiborne Johnston, VP for Medical Affairs and Dean of the Dell Medical School Ms. Rosemaria Martinelli, Chief of Staff, Office of the Executive VP and Provost Mr. Carlos Martinez, Chief of -

Capital Expenditure Plans FY 2021
Strategic Planning and Funding Capital Expenditure Plan Report Fiscal Years 2021-2025 September 2020 Texas Higher Education Coordinating Board Stuart W. Stedman, CHAIR Houston Fred Farias III, O.D., VICE CHAIR McAllen Ricky A. Raven, SECRETARY OF THE BOARD Sugar Land S. Javaid Anwar Midland Cody C. Campbell Fort Worth Emma W. Schwartz El Paso R. Sam Torn Houston Donna N. Williams Dallas Welcome W. Wilson, Jr. Houston Levi D McClenny, STUDENT REPRESENTATIVE College Station Harrison Keller, COMMISSIONER OF HIGHER EDUCATION Agency Mission The mission of the Texas Higher Education Coordinating Board (THECB) is to provide leadership and coordination for the Texas higher education system and to promote access, affordability, quality, success, and cost efficiency through 60x30TX, resulting in a globally competitive workforce that positions Texas as an international leader. Agency Vision The THECB will be recognized as an international leader in developing and implementing innovative higher education policy to accomplish our mission. Agency Philosophy The THECB will promote access to and success in quality higher education across the state with the conviction that access and success without quality is mediocrity and that quality without access and success is unacceptable. The Coordinating Board’s core values are: Accountability: We hold ourselves responsible for our actions and welcome every opportunity to educate stakeholders about our policies, decisions, and aspirations. Efficiency: We accomplish our work using resources in the most effective manner. Collaboration: We develop partnerships that result in student success and a highly qualified, globally competent workforce. Excellence: We strive for preeminence in all our endeavors. The Texas Higher Education Coordinating Board does not discriminate on the basis of race, color, national origin, gender, religion, age or disability in employment or the provision of services.