Pediatric Headache Management and Considerations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bronson Healthcare Midwest Epic Review of Systems 10.3
Bronson HealthCare Midwest Epic Review of Systems 10.3 Constitution Endocrine Activity Change Y N Cold intolerance Y N Appetite Change Y N Heat intolerance Y N Chills Y N Polydipsia Y N Diaphoresis Y N Polyuria Y N Fatigue Y N GU Fever Y N Difficulty urinating Y N Unexpctd wt chnge Y N Dyspareunia Y N HENT Dysuria Y N Facial Swelling Y N Enuresis Y N Neck pain Y N Flank pain Y N Neck stiffness Y N Frequency Y N Ear Discharge Y N Genital Sore Y N Hearing loss Y N Hematuria Y N Ear pain Y N Menstrual problem Y N Tinnitus Y N Pelvic pain Y N Nosebleeds Y N Urgency Y N Congestion Y N Urine decreased Y N Rhinorrhea Y N Vaginal bleeding Y N Postnasal drip Y N Vaginal discharge Y N Sneezing Y N Vaginal pain Y N Sinus Pressure Y N Musc Dental problem Y N Arthralgias Y N Drooling Y N Back pain Y N Mouth sores Y N Gait problem Y N Sore throat Y N Joint swelling Y N Trouble swallowing Y N Myalgias Y N Voice Change Y N Skin Eyes Color change Y N Eye Discharge Y N Pallor Y N Eye itching Y N Rash Y N Eye pain Y N Wound Y N Last Name: ___________________________________ First Name: ______________________________________ Date of Birth: _____________________________ Today’s Date: __________________________________________ Bronson HealthCare Midwest Epic Review of Systems 10.3 Eye redness Y N Allergy/Immuno Photophobia Y N Env allergies Y N Visual disturbance Y N Food Allergies Y N Respiratory Immunocompromised Y N Apnea Y N Neurological Chest tightness Y N Dizziness Y N Choking Y N Facial asymmetry Y N Cough Y N Headaches Y N Shortness of breath Y N Light-headedness -

W10: Causes and Co-Morbidities of Nocturia Workshop Chair: An-Sofie Goessaert, Belgium 12 September 2017 09:00 - 10:30
W10: Causes and Co-morbidities of Nocturia Workshop Chair: An-Sofie Goessaert, Belgium 12 September 2017 09:00 - 10:30 Start End Topic Speakers 09:00 09:20 Phenotyping Nocturia – Judge a Book by its Cover? An-Sofie Goessaert 09:20 09:40 Sleep and Nocturia – Central Mechanisms into Business? Karlien Dhondt 09:40 10:00 Bladder and Kidney – Making the Bladder Gladder or Lowering Philip Van Kerrebroeck the Water Levels? 10:00 10:20 Questionnaire on Nocturia – to TANGO or Not to TANGO? Wendy Bower 10:20 10:30 Questions All Speaker Powerpoint Slides Please note that where authorised by the speaker all PowerPoint slides presented at the workshop will be made available after the meeting via the ICS website www.ics.org/2017/programme Please do not film or photograph the slides during the workshop as this is distracting for the speakers. Aims of Workshop Nocturia is a highly prevalent condition affecting both men and women of all ages. It is no longer a problem merely attributed to overactive bladder or benign prostate hyperplasia. There can be an impairment in one or more factors of the triad brain-kidney- bladder but also other factors such as obesity, hypertension, peripheral edema, sleep disturbance, depression, medication, etc can play a role. The objective of this workshop is to provide an overview on causes and co-morbidities of nocturia and how to identify them. Learning Objectives This workshop should allow the attendant to know the answers to following questions: 1. What physical features can help you to identify possible causes or co-morbidities of nocturia? 2. -

A 27-Month-Old Boy with Polyuria and Polydipsia
UC Davis UC Davis Previously Published Works Title A 27-Month-Old Boy with Polyuria and Polydipsia. Permalink https://escholarship.org/uc/item/8x24x4p2 Authors Lee, Yvonne Winnicki, Erica Butani, Lavjay et al. Publication Date 2018 DOI 10.1155/2018/4281217 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Hindawi Case Reports in Pediatrics Volume 2018, Article ID 4281217, 4 pages https://doi.org/10.1155/2018/4281217 Case Report A 27-Month-Old Boy with Polyuria and Polydipsia Yvonne Lee,1 Erica Winnicki,2 Lavjay Butani ,3 and Stephanie Nguyen 3 1Department of Pediatrics, Section of Endocrinology, Kaiser Permanente Oakland Medical Center, Oakland, CA, USA 2Department of Pediatrics, Section of Nephrology, University of California, San Francisco, San Francisco, CA, USA 3Department of Pediatrics, Section of Nephrology, University of California, Davis, Sacramento, CA, USA Correspondence should be addressed to Stephanie Nguyen; [email protected] Received 16 May 2018; Accepted 1 August 2018; Published 23 August 2018 Academic Editor: Anselm Chi-wai Lee Copyright © 2018 Yvonne Lee et al. )is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Psychogenic polydipsia is a well-described phenomenon in those with a diagnosed psychiatric disorder such as schizophrenia and anxiety disorders. Primary polydipsia is differentiated from psychogenic polydipsia by the lack of a clear psychotic disturbance. We present a case of a 27-month-old boy who presented with polyuria and polydipsia. Laboratory studies, imaging, and an observed water deprivation test were consistent with primary polydipsia. -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -
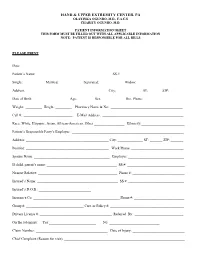
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________ -

Guidance on the Clinical Management of Acute and Chronic Harms of Club Drugs and Novel Psychoactive Substances NEPTUNE
Novel Psychoactive Treatment UK Network NEPTUNE Guidance on the Clinical Management of Acute and Chronic Harms of Club Drugs and Novel Psychoactive Substances NEPTUNE This publication of the Novel Psychoactive Treatment UK Network (NEPTUNE) is protected by copyright. The reproduction of NEPTUNE guidance is authorised, provided the source is acknowledged. © 2015 NEPTUNE (Novel Psychoactive Treatment UK Network) 2015 Club Drug Clinic/CAPS Central and North West London NHS Foundation Trust (CNWL) 69 Warwick Road Earls Court SW5 9HB http://www.Neptune-clinical-guidance.com http://www.Neptune-clinical-guidance.co.uk The guidance is based on a combination of literature review and expert clinical con sensus and is based on information available up to March 2015. We accept no responsi bility or liability for any consequences arising from the use of the information contained in this document. The recommended citation of this document is: Abdulrahim D & Bowden-Jones O, on behalf of the NEPTUNE Expert Group. Guidance on the Management of Acute and Chronic Harms of Club Drugs and Novel Psychoactive Substances. Novel Psychoactive Treatment UK Network (NEPTUNE). London, 2015. NEPTUNE is funded by the Health Foundation, an independent charity working to improve the quality of health care in the UK. Editorial production and page design by Ralph Footring Ltd, http://www.footring.co.uk NEPTUNE NEPTUNE (Novel Psychoactive Treatment UK Network): Expert Group members NEPTUNE Expert Group Dr Owen Bowden-Jones Neptune Chair Clinical and programme lead Consultant -

Unusual Case of Necrotizing Pneumonia Rajapriya Manickam*, Kabir Oladipo Olaniran and Raghu Loganathan
Manickam et al. Int J Respir Pulm Med 2015, 2:2 International Journal of ISSN: 2378-3516 Respiratory and Pulmonary Medicine Case Report : Open Access Unusual Case of Necrotizing Pneumonia Rajapriya Manickam*, Kabir Oladipo Olaniran and Raghu Loganathan Division of Pulmonary and Critical care Medicine, Lincoln Medical and Mental Health Center, USA *Corresponding author: Rajapriya Manickam, Division of Pulmonary and Critical care Medicine, Lincoln Medical and Mental Health Center, Bronx, New York, USA, Tel: 917-375-5626; E-mail: [email protected] Abstract Coccidioidomycosis is caused by inhalation of Coccidoides spores which is endemic in south western parts of USA and an uncommon cause of pneumonia in non-endemic areas. We report a young Hispanic man who lives in New York presenting with diabetic ketoacidosis and severe pulmonary Coccidioidomycosis. Through this case report and review we want to familiarize clinicians from non-endemic area to this unusual cause for necrotizing pneumonia, its association with diabetes mellitus, other risk factors for dissemination and the management strategy. Introduction Pulmonary Coccidioidomycosis is an uncommon cause of necrotizing pneumonia in non-endemic areas. We report a case of severe pulmonary Coccidioidomycosis in a young immigrant who lives in New York and discuss the association with diabetes mellitus. Hospital Course A young 32 year old Hispanic man presented with 4-weeks history of polyuria, polyphagia and weight loss and 2-weeks history Figure 1: Chest radiograph showing right upper lobe consolidation and of hemoptysis and shortness of breath. He denied fever, chills, night retraction of horizntal fissure. sweats, sick contacts, skin rash, glandular swelling or recent travel. -

Pheochromocytoma Presenting with Polydipsia And
OLGU SUNUMLARI (Case Reports) PHEOCHROMOCYTOMA PRESENTING WITH POLYDIPSIA AND POLYURIA IN A CHILD Poliüri ve polidipsi ile gelen feokromasitomalý çocuk: Olgu sunumu Ali Baykan1, Nazmi Narin1, Mustafa Kendirci1, Mustafa Akcakus1, Mustafa Küçükaydýn2, Tahir Patýroðlu3 Abstract : Pheochromocytomas are rare tumors in childhood Özet : Feokromositoma çocukluk çaðýnda nadir görülen and can mimic many unrelated diseases due to their various tümörlerdendir ve farklý semptomlarý ile birçok hastalýðý presenting symptoms. While hypertension is the most taklit edebilir. Hipertansiyon feokromositomada en sýk bulgu prevalent finding of pheochromocytomas, polyuria and olmasýna raðmen, poliüri-polidipsi nadir ve ilginç polydipsia are rare and interesting symptoms. In this study we presented a child with unilateral pheochromocytoma, semptomlardýr. Bu yazýda tek taraflý feokromositomalý, ilk whose first symptoms were polyuria-polydipsia, and semptomu poliüri-polidipsi olan ve fizik muayenede hypertension, which were important clues for hipertansiyon tespit edilen vaka takdim edilmiþtir. Klinik ve pheochromocytoma. With the help of clinical and laboratory laboratuar bulgularý ile taný konulan olguda cerrahi findings, patient was diagnosed as pheochromocytoma and rezeksiyon sonrasý bulgu ve belirtiler kayboldu. Multipl referred to surgery; with the removal of the tumor the symptoms disappeared. When the family members were endokrin neoplazi (MEN) açýsýndan aile bireyleri tarandý screened for multiple endocrine neoplasia (MEN) syndromes, ve kýz kardeþine de feokromositoma tanýsý konularak opere a bilateral pheochromocytoma was diagnosed in his sister edildi. Bu makale ile poliüri ve polidipsinin and she was also operated on immediately. In this article feokromositomanýn ilk semptomlarý olabileceðini, ilk we emphasized that polyuria-polydipsia may be the first muayenede tansiyon ölçülmesinin önemini ve symptoms of pheochromocytoma in children, the importance of blood pressure measurement in initial physical examination feokromositomanýn ailesel olabileceðini vurgulamak istedik. -

Pharmacovigilance - Post
PHARMACOVIGILANCE - POST MARKETING SURVEILLANCE NEWS Vol. 7 No. 3: Third Quarter Newsletter 2014 Editor’s Note I wish to thank all our numerous stakeholders who have been working tirelessly with the National Pharmacovigilance Centre (NPC) to ensure the safe use of medicines in Nigeria. The NPC is committed to sending quarterly newsletter to its stakeholders. The objectives of the Newsletter are to disseminate information on pharmacovigilance activities nationally and globally, to educate stakeholders on medicine safety issues, to promote rational use of drugs and to promote spontaneous reporting. This third quarter Newsletter focuses on Pharmacovigilance of Antidiabetic Drugs. We encourage all Health Care Professionals, Marketing Authorization Holders and other stakeholders to continue to report all adverse drug reactions. Your valued comments and acknowledgement of receipt of this issue through our email addresses ([email protected]; pharmacovigilance@nafdac,gov.ng ) would be most appreciated. Pharm. (Mrs.) Osakwe Director/NationalCoordinator, National Pharmacovigilance Centre (NPC) National Agency for Food and Drug Administration and Control (NAFDAC) Plot 2032 Olusegun Obasanjo Way Wuse Zone 7 Abuja PMB 5032 Wuse Abuja. Telephone 07098211221, 08086899571 E-mail: [email protected]; [email protected]; [email protected]; Website :www.nafdac.gov.ng Text any DRUG RELATED PROBLEM to SHORT CODE 20543 (for free on MTN, GLO and Etisalat) for action by the Pharmacovigilance Centre 1 PHARMACOVIGILANCE OF ANTIDIABETIC DRUGS Diabetes is one of the major causes of illnesses and deaths globally, and it affects many regardless of age or race. This disease can contribute to other health complications such as heart disease, kidney disease and blindness if not properly treated. -

The Basics of Pharmacology
THE BASICS OF PHARMACOLOGY Endocrine, Musculoskeletal, Genitourinary, Ear And Eye Systems Jassin M. Jouria, MD Dr. Jassin M. Jouria is a practicing Emergency Medicine physician, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serve as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e- module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. ABSTRACT The science of pharmacology and the responsibility relationship building with patients are important elements of a health professional’s clinical knowledge and skills to provide safe and appropriate pharmacotherapeutic regimens in everyday practice. Interdisciplinary members of the health team are required to continually interpret specific patient health data to implement and evaluate outcomes of medication treatment. All health clinicians are increasingly relying on practice guidelines and the applied specialized training of health team members when obtaining the patient health history to improve therapeutic medication regimens, avoid adverse effects, and to safely and effectively treat a disease state. -

Partial Target Organ Resistance to Thyroid Hormone
Partial Target Organ Resistance to Thyroid Hormone Hans Henning Bode, … , Farahe Maloof, John D. Crawford J Clin Invest. 1973;52(4):776-782. https://doi.org/10.1172/JCI107240. Research Article An 8-year old boy with a small goiter, normal basal metabolic rate (BMR), and elevated serum thyroid hormone levels (thyroxine [T4] 19.5 μg per 100 ml, free T4 4 ng per 100 ml, triiodothyronine [T3] 505 ng per 100 ml) was studied. He had measurable serum thyroid-stimulating hormone (TSH) levels (average 5.5 μU per ml), and the thyroxine-binding proteins, hearing, and epiphyseal structures were normal. There was no parental consanguinity nor were there thyroid abnormalities either in the parents or six siblings. Methimazole, 50 mg daily, depressed thyroxine synthesis (T4 10.5, free T4 2.5) and caused a rise in TSH to 11 μU per ml. After discontinuation of treatment, TSH declined to 4.2 μU per ml and chemical hyperthyroidism returned (T4 21.0 μg per 100 ml, free T4 4.2, and total T3 475 ng per 100 ml, radioactive iodine [RAI] uptake 68%), but studies of BMR and insensible water loss showed the patient to be clinically euthyroid. Thyrotropin-releasing hormone (TRH), 200 μg i.v., caused a brisk rise in TSH to 28 μU per ml, with T4 rising to 28 μg per 100 ml, free T4 to 5.6, and T3 to 730 ng per 100 ml, thus indicating that the pituitary-thyroid system was intact and that the patient's TSH was biologically active. The unusual sensitivity of the pituitary cells to TRH […] Find the latest version: https://jci.me/107240/pdf Partial Target Organ Resistance to Thyroid Hormone HANS HENNING BODE, MARco DANON, BRUCE D.