Integrating Peripheral Biomarker Analyses From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Moderna Appoints Oncology Leader Dr. Stephen Kelsey As President of Onkaido
Moderna Appoints Oncology Leader Dr. Stephen Kelsey as President of Onkaido Former Genentech executive to lead Moderna’s first venture company, focused exclusively in novel biology for oncology drug development CAMBRIDGE, Mass., July 1, 2014— Moderna Therapeutics, the pioneer in developing messenger RNA (mRNA) TherapeuticsTM, a revolutionary treatment modality to enable the in vivo production of therapeutic proteins, announced today that Stephen Kelsey, M.D., will become president of Onkaido Therapeutics, Moderna’s oncology drug development company, effective July 21. Launched in January of this year, Onkaido is Moderna’s first venture company, focused exclusively on developing and commercializing mRNA-based oncology treatments. “As we continue to grow Moderna and perfect our mRNA Therapeutics platform, we are also focused on building a transformational oncology company that will benefit patients and society. This requires hiring the best oncology talent to lead Onkaido,” said Stéphane Bancel, president and founding chief executive officer, Moderna. “Steve brings a wealth of experience in oncology drug development to his new role. His knowledge and leadership, combined with the team of Onkaido scientists and Moderna’s innovative mRNA technology, will help speed a new class of cancer drugs to patients around the world.” Dr. Kelsey has extensive pharmaceutical industry experience in oncology. After 16 years as an academic clinician, he started his industry career at Sugen, and later was vice president of hematology/oncology at Genentech. While at Genentech, Dr. Kelsey played a significant role in the development of key products Perjeta®, Kadcyla® and Erivedge®, as well as other molecules in the company’s oncology portfolio. He left Genentech in 2009 to run Geron’s oncology division, where he served for four years as executive vice president, research and development, and chief medical officer helping to develop therapeutics and vaccines to fight cancer. -

Print Layout 1
TECHNICAL PROGRAM Monday, March 19 5:00 – 8:00 pm Welcome Reception Tuesday, March 20 8:00 – 10:00 Session 1: Setting the Conference Context and Drivers Chair: Geoff Slaff (Amgen) Roger Perlmutter (Amgen) Conquering the Innovation Deficit in Drug Discovery Helen Winkle (CDER, FDA) Regulatory Modernization 10:00 – 10:30 Break Vendor and poster review 10:30 – 12:30 Session 2: Rapid Cell Line Development and Improved Expression System Development Chairs: Timothy Charlebois (Wyeth) and John Joly (Genentech) Amy Shen (Genentech) Stable Antibody Production Cell-Line Development with an Improved Selection Process and Accelerated Timeline Mark Leonard (Wyeth) High-Performing Cell-Line Development within a Rapid and Integrated Platform Process Control Pranhitha Reddy (Amgen) Applying Quality-by-Design to Cell Line Development Lin Zhang (Pfizer) Development of a Fully-Integrated Automated System for High-Throughput Screening and Selection of Single Cells Expressing Monoclonal Antibodies 12:30 – 2:00 Lunch Vendor and poster review 2:00 – 4:30 Session 3: High-Throughput Bulk Process Development Chairs: Brian Kelley (Wyeth) and Jorg Thommes (Biogen Idec) Colette Ranucci (Merck) Development of a Multi-Well Plate System for High-Throughput Process Development Min Zhang (SAFC Biosciences) CHO Media Library – an Efficient Platform for Rapid Development and Optimization of Cell Culture Media Supporting High Production of Pharmaceutical Proteins in Chinese Hamster Ovary Cells Nigel Titchener-Hooker The Use of Ultra-Scale-Down Approaches to Enable Rapid Investigation -

Genentech Tocilizumab Letter of Authority June 24 2021
June 24, 2021 Hoffmann-La Roche, Ltd. C/O Genentech, Inc. Attention: Dhushy Thambipillai Regulatory Project Management 1 DNA Way, Bldg 45-1 South San Francisco, CA 94080 RE: Emergency Use Authorization 099 Dear Ms. Thambipillai: This letter is in response to Genentech, Inc.’s (Genentech) request that the Food and Drug Administration (FDA) issue an Emergency Use Authorization (EUA) for the emergency use of Actemra1 (tocilizumab) for the treatment of coronavirus disease 2019 (COVID-19) in certain hospitalized patients, as described in the Scope of Authorization (Section II) of this letter, pursuant to Section 564 of the Federal Food, Drug, and Cosmetic Act (the Act) (21 U.S.C. §360bbb-3). On February 4, 2020, pursuant to Section 564(b)(1)(C) of the Act, the Secretary of the Department of Health and Human Services (HHS) determined that there is a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad, and that involves the virus that causes coronavirus disease 2019 (COVID-19).2 On the basis of such determination, the Secretary of HHS on March 27, 2020, declared that circumstances exist justifying the authorization of emergency use of drugs and biological products during the COVID-19 pandemic, pursuant to Section 564 of the Act (21 3 U.S.C. 360bbb-3), subject to terms of any authorization issued under that section. Actemra is a recombinant humanized monoclonal antibody that selectively binds to both soluble and membrane-bound human IL-6 receptors (sIL-6R and mIL-6R) and subsequently inhibits IL- 6-mediated signaling through these receptors. -

Companies in Attendance
COMPANIES IN ATTENDANCE Abbott Diabetes Care Archbow Consulting LLC Business One Technologies Abbott Laboratories ARKRAY USA BusinessOneTech AbbVie Armory Hill Advocates, LLC CastiaRX ACADIA Artia Solutions Catalyst Acaria Health Asembia Celgene Accredo Assertio Therapeutics Celltrion Acer Therapeutics AssistRx Center for Creative Leadership Acorda Therapeutics Astellas Pharma US Inc. Cigna Actelion AstraZeneca Cigna Specialty Pharmacy AdhereTech Athenex Oncology Circassia Advantage Point Solutions Avanir Coeus Consulting Group Aerie Pharmaceuticals Avella Coherus Biosciences AGIOS AveXis Collaborative Associates LLC Aimmune Theraputics Bank of America Collegium Akcea Therapeutics Bausch Health Corsica Life Sciences Akebia Therapeutics Bayer U.S. CoverMyMeds Alder BioPharmaceuticals Becton Dickinson Creehan & Company, Inc., an Inovalon Company Alexion Biofrontera CSL Behring Alkermes Biogen Curant Health Allergan Biohaven CVS Health Almirall BioMarin D2 Consulting Alnylam BioMatrix Specialty Pharmacy Daiichi Sankyo Amarin BioPlus Specialty Pharmacy DBV Technologies Amber Pharmacy Bioventus Deloitte Consulting LLP AmerisourceBergen Blue Cross Blue Shield Association Dendreon Amgen Blue Fin Group Dermira Amicus Therapeutics bluebird bio Dexcom Amneal Boehringer Ingelheim Diplomat Pharmacy Anthem Boston Biomedical Dova Applied Policy Bowler and Company Decision Resources Group Aquestive Therapeutics Braeburn Eisai Arbor Pharmaceuticals Bristol-Myers Squibb 1 electroCore Indivior Merz Pharmaceuticals EMD Serono Inside Rx Milliman Encore Dermatology, -

News Release
NEWS RELEASE Media: Nikki Levy (650) 225-1729 Investor: Susan Morris (650) 225-6523 Biogen Idec Contacts: Media: Amy Brockelman (617) 914-6524 Investor: Eric Hoffman (617) 679-2812 GENENTECH AND BIOGEN IDEC ANNOUNCE POSITIVE RESULTS FROM A PHASE II TRIAL OF RITUXAN IN RELAPSING-REMITTING MULTIPLE SCLEROSIS SOUTH SAN FRANCISCO, Calif. and CAMBRIDGE, Mass. – August 28, 2006 – Genentech, Inc. (NYSE: DNA) and Biogen Idec, Inc. (Nasdaq: BIIB) announced today that a Phase II study of Rituxan® (Rituximab) for relapsing-remitting multiple sclerosis (RRMS) met its primary endpoint. The study of 104 patients showed a statistically significant reduction in the total number of gadolinium enhancing T1 lesions observed on serial MRI scans of the brain at weeks 12, 16, 20 and 24 in the Rituxan-treated group compared to placebo. Genentech and Biogen Idec will continue to analyze the study results and will submit the data for presentation at an upcoming medical meeting. “These initial results exceeded our expectations,” said Hal Barron, M.D., Genentech senior vice president, development and chief medical officer. “Showing a significant benefit at 24 weeks in this small Phase II trial supports our hypothesis that selective B-cell targeted therapy may play an important role in the treatment of MS.” - more - - 2 - “Biogen Idec is committed to offering multiple options for people living with MS, a devastating disease. We are very encouraged by these data and look forward to learning more about the potential of Rituxan as a therapy to treat MS,” said Alfred Sandrock, M.D., Ph.D., senior vice president, neurology research and development, Biogen Idec. -

The Path Less Costly
COMMENtaRY CASE STUDY The path less costly Brady Huggett When faced with a competitive threat, two companies took diametrically opposite approaches. Both were ultimately successful, but Genzyme’s decision proved to be the cleaner and cheaper option. s the world’s leader in developing enzyme-replacement drugs, and Novartis of Basel. Houston-based Tanox was founded in 1986 to AGenzyme has always understood the importance of first to market. In focus on anti-IgE antibodies and by 1989 was looking for a clinical 1991, the company obtained approval for Ceredase (alglucerase injection), development partner; it sent samples of its candidate to both Genentech an enzyme replacement therapy for lysosomal storage disease (LSD) type and Ciba Geigy (the company that would later become Novartis). 1 Gaucher. Three years later, its second-generation product, Cerezyme Genentech passed. Ciba Geigy, however, began working with Tanox (imiglucerase for injection), was also cleared for commercialization. The on anti-IgE antibodies for allergic diseases. lack of treatments for lysosomal storage diseases and effective patient out- Yet Genentech clearly had interest in the area, because it began its own reach and marketing meant that Genzyme could command soaring prices anti-IgE program a few years later—a move that prompted a misappro- for its orphan treatments. In 2000, the two drugs alone provided 66% of priation suit from Tanox. The companies fought in court for three years Genzyme’s entire product revenue. before Genentech, Tanox and Novartis reached a settlement and entered At this time, Novazyme Pharmaceuticals was a young company devel- a cross-licensing agreement for anti-IgE antibodies. -

Oral Presentation Disclosures
Oral Presentation Disclosures Adler, Lenard – Alcobra Pharma, APSARD/Pond Foundation, Major League Baseball, Major League Baseball Players Association, National Football League, New York University School of Medicine, Novartis Bioventures, Shire Pharmaceuticals, Sunovion, SUNY Upstate, Theravance, US Department of Veterans Affairs Cooperative Studies Program Anton, Raymond – Abbvie, Alkermes, Eli Lilly, Ethypharm, Lundbeck, Pfizer, Sunpharma Baker, Ross – Otsuka Pharmaceutical Development & Commercialization, Inc. Baldwin, David – Lundbeck Beaver, Jessica – Targacept, Inc. Bencherif, Merouane – Targacept, Inc. Bertolino, Alessandro – F. Hoffmann-La Roche, Ltd. Bradshaw, Mark – Euthymics Bioscience, Neurovance, Inc. Burdick, Katherine – Dainippon Sumitomo Pharma Bymaster, Frank – Euthymics Bioscience, Neurovance, Inc. Calabrese, Joseph – Sunovion, Teva (Cephalon) Cantillon, Marc – Forest, Kyowa, Lilly, Merck, Pfizer, Reviva Caroff, Stanley – Sunovion Chen, Yinzhong – Takeda Development Center Americas, Inc. Chengappa, Roy – Pfizer, Inc. Childress, Ann – Abbott Laboratories, Bristol Myer Squibb, GlaxoSmithKline, Ironshore, Janssen (Ortho-McNeil), Johnson & Johnson PRD, Lilly, Neos Therapeutics, Neurovance Inc., NextWave, Novartis, Noven, Otsuka, Pfizer, Rhodes, Sepracor, Shionogi, Shire, Somerset, Sunovion, Theravance Christine, Mazzucco – Janssen Cohen, Lee – Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb, Cephalon, Inc., GlaxoSmithKline, National Institute of Mental Health, National Institute on Aging, Noven Pharmaceuticals, Ortho-McNeil -

Genentech 2002 Annual Report the Acceleration of Scientific Knowledge Over Time Has Been Profound— and It Is Ceaseless
What we don’t yet know could change everything. Genentech 2002 Annual Report The acceleration of scientific knowledge over time has been profound— and it is ceaseless. Today, the span of time between great discoveries in medicine gets smaller and smaller due in part to the relatively new field of biotechnology. And the number of breakthroughs and new approaches to disease continues to grow. At Genentech, we believe we have only just begun to scratch the surface of biotechnology’s potential. Without a doubt, future discoveries will dramatically change our understanding of serious illnesses and potential treatments. Even more importantly, science is likely to create dramatic change at a more personal level— increasing the length and quality of life for our loved ones and ourselves. What if one day everyone could survive cancer? Cancer is the second leading cause of death in the United States behind heart disease, with over 1.2 million new cases diagnosed per year. Some predict it will become number one in the next 10 years. Curing cancer is our ultimate goal, but if we are able to keep cancer in check, extend patients’ lives and improve their quality of life, that will be a major victory over the disease. Genentech developed the first two therapeutic antibodies for cancer in the United States, Rituxan® (Rituximab), which was co-developed with IDEC Pharmaceuticals, and Herceptin® (Trastuzumab) — both of which attack malignant cells without causing extensive damage to healthy tissues. Rituxan and Herceptin are different from chemotherapy in that, although they are serious medicines, they tend to have relatively few side effects and can sometimes be taken for prolonged periods to stave off the disease. -

2019 Annual Meeting Education Committee All Relationships Are Considered Compensated
2019 Annual Meeting Education Committee All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Patents, Royalties, Travel, Stock and Other Expert Name Employment Leadership Honoraria Consulting or Advisory Role Speakers' Bureau Research Funding Other Intellectual Accommodations, Other Ownership Interests Testimony Property Expenses Monica M. Abbvie (Inst), Agenus (Inst), Astellas Bertagnolli Pharma (Inst), AstraZeneca (Inst), Baxalta (Inst), Bayer Health (Inst), Breast Cancer Research Foundation (Inst), Bristol- Myers Squibb (Inst), Celgene (Inst), Complion (Inst), Eisai (Inst), Exelixis (Inst), Genentech (Inst), GHI Pharma (Inst), Gilead Sciences (Inst), GlaxoSmithKline (Inst), Incyte (Inst), Janssen (Inst), Jazz Pharmaceuticals (Inst), Leidos (Inst), Lexicon (Inst), Lilly (Inst), Matrex (Inst), Mayo Clinic (Inst), Merck (Inst), MGH (Inst), Millenium Pharamceuticals (Inst), Novartis (Inst), PCORI (Inst), Pfizer (Inst), Pharmacyclics (Inst), Robert Wood Johnson Foundation (Inst), Sagerock Advisors (Inst), Sanofi (Inst), Taiho Oncology (Inst), Takeda (Inst), Tesaro (Inst), Teva (Inst) Tatiana M. Prowell David R. Spigel AstraZeneca (Inst), Boehringer AstraZeneca (Inst), Boehringer Ingelheim (Inst), Bristol-Myers Ingelheim (Inst), Bristol-Myers Squibb Squibb (Inst), Celgene (Inst), (Inst), Celgene (Inst), Genentech/Roche Genentech/Roche (Inst), (Inst), Lilly (Inst), Merck (Inst), Novartis Novartis (Inst), Pfizer (Inst) (Inst), Pfizer (Inst), University -

Genentech Patient Foundation Patient Consent Form
PATIENT CONSENT FORM Genentech-Access.com Phone: (888) 941-3331 Fax: (833) 999-4363 6 a.m.–5 p.m. (PT) M-F M-US-00002802(v1.0) 01/20 Instructions for Patients By completing this form you can: Please follow these 3 steps to get started: Learn about your health insurance coverage and 1. Read “About Your Consent.” other options to get your Genentech medicine 2. Sign and date page 3. Please note you must sign the form to get support for your treatment. Enroll into optional disease-specific education, patient support services and communication 3. Send in your completed form using one of the options below. Genentech can start supporting you when page 3 of this form is submitted by you or your doctor's office in one of the following ways: OR OR Complete online at Take a photo and text it to Print, complete and fax it to Genentech-Access.com/PatientConsent (650) 877-1111 (833) 999-4363 A representative from Genentech Access Solutions or your doctor’s office will call you to tell you about your coverage, costs and support for your treatment. If you have any questions, talk to your health care provider or contact Genentech Access Solutions. Helpful Terminology Genentech: The maker of the medicine your doctor wants Education and patient support services: Optional programs to prescribe. Genentech is committed to helping patients offered by Genentech to help you start and stay on your get the medicine their doctor prescribed. medicine. Services may vary based on your medical condition Genentech Access Solutions: A team at Genentech that and could include co-pay assistance, clinical support, works with your doctor and health insurance plan to help marketing communication and general disease information. -

Biosimilars: 2019 a Year in Review
January 16, 2020 Webinar Series: Biosimilars Biosimilars: 2019 A Year in Review John Adkisson Tasha Francis Jenny Shmuel Principal Associate Principal Twin Cities Twin Cities Boston TODAY’S AGENDA • U.S. Market for Biosimilars • FDA Biosimilar Guidance • Biosimilar Legislation • Biosimilar Litigation • Antitrust Developments • Post Grant Activity • Looking Forward to 2020 fr.com | 2 FDA Approved 26 Biosimilars by End of 2019 Biosimilar Biologic Reference Product FDA Approval Date Biosimilar Code 1 Zarxio (Sandoz) Neupogen (Amgen) March 2015 Filgrastim-sndz 2 Inflectra (Pfizer/Celltrion) Remicade (J&J) April 2016 Infliximab-dyyb 3 Erelzi (Sandoz) Enbrel (Amgen) August 2016 Etanercept-szzs 4 Amjevita (Amgen) Humira (AbbVie) September 2016 Adalimumab-atto 5 Renflexis (Samsung Bioepis/Merck) Remicade (J&J) April 2017 Infliximab-abda 6 Cyltezo / BI-695501 (BI) Humira (AbbVie) August 2017 Adalimumab-adbm 7 Mvasi (Amgen) Avastin (Roche) September 2017 Bevacizumab-awwb 8 Ogivri (Mylan) Herceptin (Genentech/Roche) December 2017 Trastuzumab-dkst 9 Ixifi (Pfizer) Remicade (J&J) December 2017 Infliximab-qbtx 10 Retacrit (Pfizer/Hospira) Epogen/Procrit (Amgen/J&J) May 2018 Epoetin alfa-epbx 11 Fulphila (Mylan/Biocon) Neulasta (Amgen) June 2018 Pegfilgrastim-jmdb 12 Nivestym (Pfizer) Neupogen (Amgen) July 2018 Filgrastim-aafi 13 Hyrimoz (Sandoz) Humira (AbbVie) November 2018 Adalimumab-adaz 14 Udencya / CHS-1701 (Coherus) Neulasta (Amgen) November 2018 Pegfilgrastim-cbqv 15 Truxima (Celltrion/Teva) Rituxan (Roche/Genentech) November 2018 Rituximab-abbs -
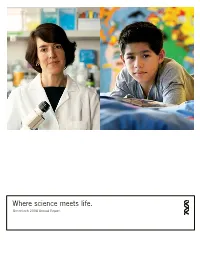
Where Science Meets Life. Genentech 2006 Annual Report
Where science meets life. Genentech 2006 Annual Report Header Genentech’s novel medicines are where cutting-edge science meets everyday life, where scientists working hard in labs intersect with individuals working hard to enjoy their lives while confronting serious and life-threatening illnesses. Our scientists and patients inspire each other and the rest of us at Genentech as we strive to develop therapies that dramati- cally improve the treatment options for people with critical medical conditions. On Cover: Ellen Filvaroff, Senior Scientist; Alex Alvarado, Nutropin AQ® Patient and Recipient of Free Medicine From the Genentech® Access to Care Foundation Our Mission Genentech’s mission is to be the leading biotechnology company, using human genetic information to discover, develop, manufacture and commercialize biotherapeutics that address significant unmet medical needs. The company is committed to high standards of integrity in contributing to the best interests of patients, the medical profession, our employees and our communities, and to seeking significant returns to our stockholders based on the continual pursuit of scientific and operational excellence. Letter to Stockholders Arthur D. Levinson, Ph.D. Chairman and Chief Executive Officer “We see tremendous advances in understanding the biological basis of many debilitating diseases, and we believe these advances play to Genentech’s greatest strengths as we try to translate the biology into new therapies.” Letter to Stockholders Dear Stockholders, I am happy to report that 2006 was another remarkable market for Genentech, the Lucentis launch was our most year for Genentech, with important developments across successful to date. Lucentis had U.S. sales of $380 million all areas of the business.