Colonoscopic Diagnosis of Rectal Perforation by Foreign Body
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

Rectal Foreign Body: a Primer for Emergency Physicians Bobby Desai
Desai International Journal of Emergency Medicine 2011, 4:73 http://www.intjem.com/content/4/1/73 CASEREPORT Open Access Visual diagnosis: Rectal foreign body: A primer for emergency physicians Bobby Desai Abstract We present a case that is occasionally seen within emergency departments, namely a rectal foreign body. After presentation of the case, a discussion concerning this entity is given, with practical information on necessity of an accurate and thorough history and removal of the object for clinicians. Case anoscope inserted. The object could not be visualized, A 39-year-old male presented to the Emergency Depart- and therefore no attempt was made to remove it. Gen- ment with vague complaints of abdominal pain and con- eral surgery was consulted to see the patient and stipation. He stated that the abdominal pain was dull decided to take him to the operating room for removal. and crampy in nature and generalized in distribution. The patient agreed to this. Furthermore, he stated that he had not had a bowel The object was noted to be the extension arm of a movement in 2 days, though he felt as if he had to have vacuum cleaner. It was removed according to notes with one. He denied constitutional complaints of fevers, some difficulty and the patient was admitted to the hos- chills, nausea, and vomiting, and denied urinary com- pital for observation and intravenous antibiotics. The plaints as well. patient was subsequently discharged 2 days later in The patient’s vital signs were: temperature 37.2°C, excellent condition. Upon social work discharge, he was pulse 87 beats per minute, respiratory rate of 20 per again asked how that apparatus managed to be placed minute, and blood pressure 130/84 mmHg. -

The American Society of Colon and Rectal Surgeons' Clinical Practice
CLINICAL PRACTICE GUIDELINES The American Society of Colon and Rectal Surgeons’ Clinical Practice Guideline for the Evaluation and Management of Constipation Ian M. Paquette, M.D. • Madhulika Varma, M.D. • Charles Ternent, M.D. Genevieve Melton-Meaux, M.D. • Janice F. Rafferty, M.D. • Daniel Feingold, M.D. Scott R. Steele, M.D. he American Society of Colon and Rectal Surgeons for functional constipation include at least 2 of the fol- is dedicated to assuring high-quality patient care lowing symptoms during ≥25% of defecations: straining, Tby advancing the science, prevention, and manage- lumpy or hard stools, sensation of incomplete evacuation, ment of disorders and diseases of the colon, rectum, and sensation of anorectal obstruction or blockage, relying on anus. The Clinical Practice Guidelines Committee is com- manual maneuvers to promote defecation, and having less posed of Society members who are chosen because they than 3 unassisted bowel movements per week.7,8 These cri- XXX have demonstrated expertise in the specialty of colon and teria include constipation related to the 3 common sub- rectal surgery. This committee was created to lead inter- types: colonic inertia or slow transit constipation, normal national efforts in defining quality care for conditions re- transit constipation, and pelvic floor or defecation dys- lated to the colon, rectum, and anus. This is accompanied function. However, in reality, many patients demonstrate by developing Clinical Practice Guidelines based on the symptoms attributable to more than 1 constipation sub- best available evidence. These guidelines are inclusive and type and to constipation-predominant IBS, as well. The not prescriptive. -

Small Bowel Obstruction After Laparoscopic Roux-En-Y Gastric Bypass Presenting As Acute Pancreatitis: a Case Report
Netherlands Journal of Critical Care Submitted January 2018; Accepted April 2018 CASE REPORT Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass presenting as acute pancreatitis: a case report N. Henning1, R.K. Linskens2, E.E.M. Schepers-van der Sterren3, B. Speelberg1 Department of 1Intensive Care, 2Gastroenterology and Hepatology, and 3Surgery, Sint Anna Hospital, Geldrop, the Netherlands. Correspondence N. Henning - [email protected] Keywords - Roux-en-Y, gastric bypass, pancreatitis, pancreatic enzymes, small bowel obstruction, biliopancreatic limb obstruction. Abstract Small bowel obstruction is a common and potentially life-threatening bowel obstruction within this complication after laparoscopic Roux-en-Y gastric bypass surgery. population, because misdiagnosis We describe a 30-year-old woman who previously underwent can have disastrous outcomes.[1,3-5,7] gastric bypass surgery. She was admitted to the emergency In this report we describe the department with epigastric pain and elevated serum lipase levels. difficulty of diagnosing small Conservative treatment was started for acute pancreatitis, but she bowel obstruction in post- showed rapid clinical deterioration due to uncontrollable pain and LRYGB patients and why frequent excessive vomiting. An abdominal computed tomography elevated pancreatic enzymes scan revealed small bowel obstruction and surgeons performed can indicate an obstruction in an exploratory laparotomy with adhesiolysis. Our patient quickly these patients. The purpose of improved after surgery and could be discharged home. This case this manuscript is to emphasise report emphasises that in post-bypass patients with elevated Figure 1. Roux-en-Y gastric bypass that in post-bypass patients with pancreatic enzymes, small bowel obstruction should be considered ©Ethicon, Inc. -

Perforation Due to a Rectal Foreign Body and Radiological Findings
Case Report Ann Colorectal Res 2021;9(1):44-46. Perforation Due to a Rectal Foreign Body and Radiological Findings Saim Turkoglu1, MD; Adem Yokuş2, MD; Fırat Aslan3, MD 1Van Traınıng and Research Hospıtal, Van, Turkey 2Department of Radiology, Medical Faculty, Yuzuncu Yıl University, Van, Turkey 3Department of General Surgery, Medical Faculty, Yuzuncu Yıl University, Van, Turkey *Corresponding authors: Received: 01-03-2021 Saim Turkoglu, Van Traınıng and Research Hospıtal, Van,Turkey Revised: 03-04-2021 Tel: +90 5356452865; Fax: +90 432 2150471 Accepted: 05-04-2021 Email: [email protected] Abstract Introduction: Rectal foreign bodies have been increasingly seen and cause urgent surgical complications. Diagnosis and treatment of these cases in emergency departments may be difficult. The effective use of radiological imaging techniques can accelerate and facilitate this process. Case Presentation: A 65-year-old male patient, who underwent computed tomography (CT) with the suspicion of a foreign body in the rectum, was admitted to the emergency outpatient clinic. The patient was a male with a psychiatric illness who later underwent emergency surgery. Since the patient had impaired consciousness during the examination, anamnesis could not be obtained, so the initial impression upon surgical consultation was perforation due to rectal tumoral thickening. In almost all cases, plain radiography is sufficient and can eliminate diagnostic difficulties. However, this is not possible for non-opaque objects. Therefore, the CT scan played an important role in the diagnosis of this patient. A 30 cm foreign body, identified as salami, was removed from the abdomen of the patient, who was later taken for emergency surgery. -

High Quality Fecal Occult Blood Testing (FOBT) for CRC Screening: Evidence and Recommendations
High Quality Fecal Occult Blood Testing (FOBT) for CRC Screening: Evidence and Recommendations Rationale for use of FOBT High sensitivity fecal occult blood testing (FOBT) is one of the colorectal cancer screening methods recommended in guidelines from the American Cancer Society, the US Preventive Services Taskforce, and every other major medical organization. In spite of this widespread endorsement, primary care clinicians often express conviction that colonoscopy is the “gold standard” test for colorectal cancer screening and that the use of FOBT represents sub-standard care. These beliefs persist in spite of well-documented shortcomings of endoscopy (missed adenomas and cancers, higher complication rates and higher one-time costs than other screening methodologies), and the fact that access to endoscopy is limited or non- existent for a significant proportion of the U.S. population. Many clinicians are also unaware that randomized controlled trials of FOBT screening have demonstrated decreases in colorectal cancer incidence and mortality, and modeling studies suggest that the years of life saved through a high quality FOBT screening program are essentially the same as with a high quality colonoscopy based screening programs. Recent advances in stool blood screening include the emergence of new tests and improved understanding of the impact of quality factors on testing outcomes. This document provides state-of-the-science information about high quality stool testing. Types of Fecal Occult Blood Tests Two main types of FOBT are available – guaiac and immunochemical. Both types of FOBT have been shown to have reasonably high detection rates for colon and rectal cancers; adenoma detection rates are appreciably lower. -

ICD~10~PCS Complete Code Set Procedural Coding System Sample
ICD~10~PCS Complete Code Set Procedural Coding System Sample Table.of.Contents Preface....................................................................................00 Mouth and Throat ............................................................................. 00 Introducton...........................................................................00 Gastrointestinal System .................................................................. 00 Hepatobiliary System and Pancreas ........................................... 00 What is ICD-10-PCS? ........................................................................ 00 Endocrine System ............................................................................. 00 ICD-10-PCS Code Structure ........................................................... 00 Skin and Breast .................................................................................. 00 ICD-10-PCS Design ........................................................................... 00 Subcutaneous Tissue and Fascia ................................................. 00 ICD-10-PCS Additional Characteristics ...................................... 00 Muscles ................................................................................................. 00 ICD-10-PCS Applications ................................................................ 00 Tendons ................................................................................................ 00 Understandng.Root.Operatons..........................................00 -
Exploratory Laparotomy.Docx
EXPLORATORY LAPAROTOMY CONSENT FORM Your physician has determined that you may have a disease or abnormality inside your abdomen which may be life threatening, preventing pregnancy or causing medical problems if not treated. An exploratory laparotomy is an operation in which the doctor makes a surgical “cut” in the belly. Sometimes this operation is done to make sure that no disease or abnormality exists. If the physician finds that a disease is found or if the physician doesn’t feel that corrective surgery should be done immediately, then he will close up the surgical cut. If major corrective surgery is done the risk will be greater than if no corrective surgery is done. It is possible that you will be worse after the operation. Your physician can make no guarantee as to the result that might be obtained from this operation. Complications from exploratory surgery of the abdomen without any corrective surgery are infrequent, but they do occur. As with any surgical procedure, complications from bleeding and infection can occur. These complications can result in prolonged illness, the need for blood transfusions, poor healing wounds, scarring and the need for further operations. Other uncommon complications of this operation include: Damage to the intestines, blocked bowels, hernia or “rupture” developing at the site of the surgical cut, heart attacks or stroke, blood clots in the lungs and pneumonia. Some complications of exploratory surgery of the abdomen may require further surgery, some can cause permanent deformity and rarely, some can even be fatal. Furthermore, there may be alternative therapeutic or diagnostic methods available to you in addition to exploratory surgery. -

Surgical Management of Anorectal Foreign Bodies H Cinar, M Berkesoglu1, M Derebey2, E Karadeniz3, C Yildirim4, K Karabulut2, T Kesicioglu5, K Erzurumlu2
[Downloaded free from http://www.njcponline.com on Monday, June 11, 2018, IP: 102.251.47.77] Original Article Surgical Management of Anorectal Foreign Bodies H Cinar, M Berkesoglu1, M Derebey2, E Karadeniz3, C Yildirim4, K Karabulut2, T Kesicioglu5, K Erzurumlu2 Department of General Purpose: Anorectal foreign bodies (AFBs) inserted into anus constitute one of Surgery, Faculty of Medicine, the most important problems needing surgical emergency due to its complications. Ordu University, Ordu, 1Department of General We describe our experience in the diagnosis and treatment of AFBs retained Surgery, Mersin University, in the rectosigmoid colon. Materials and Methods: Between the years 2006 Abstract Mersin, 2Department of and 2015, a total of 11 patients diagnosed with AFBs were admitted to an General Surgery, Ondokuz emergency room and general surgery clinics. They were diagnosed and treated Mayıs University, Samsun, in four different hospitals in four different cities in Turkey. Information on the 3Department of General AFBs, clinical presentation, treatment strategies, and outcomes were documented. Surgery, Atatürk University, Erzurum, 4Department of We retrospectively reviewed the medical records of these unusual patients. General Surgery, Ordu Public Results: Eleven patients were involved in this study. All patients were male with Hospital, Ordu, 5Department their mean age was 49.81 (range, 23–71) years. The time of the presentation to of General Surgery, Faculty the removal of the foreign bodies ranged between 2 h and 96 h with a mean of of Medicine, Giresun 19.72 h. Ten patients inserted AFBs in the anus with the purpose of eroticism but University, Giresun, Turkey one patient’s reason to relieve constipation. -
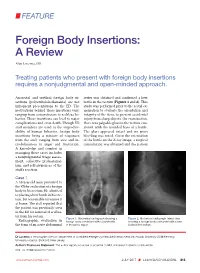
Foreign Body Insertions: a Review
FEATURE Foreign Body Insertions: A Review Alan Lucerna, DO Treating patients who present with foreign body insertions requires a nonjudgmental and open-minded approach. Anorectal and urethral foreign body in- series was obtained and confirmed a beer sertions (polyembolokoilamania) are not bottle in the rectum (Figures 1 and 2). This infrequent presentations to the ED. The study was performed prior to the rectal ex- motivations behind these insertions vary, amination to evaluate the orientation and ranging from autoeroticism to reckless be- integrity of the item, to prevent accidental havior. These insertions can lead to major injury from sharp objects. On examination, complications and even death. Though ED there was palpable glass in the rectum con- staff members are used to the unpredict- sistent with the rounded base of a bottle. ability of human behavior, foreign body The glass appeared intact and no gross insertions bring a mixture of responses bleeding was noted. Given the orientation from the staff, ranging from awe and in- of the bottle on the X-ray image, a surgical credulousness to anger and frustration. consultation was obtained and the patient A knowledge and comfort in managing these cases includes a nonjudgmental triage assess- ment, collective professional- ism, and self-awareness of the staff’s reaction. Case 1 A 58-year-old man presented to the ED for evaluation of a foreign body in his rectum. He admitted to placing a beer bottle in his rec- tum, but was unable to remove it at home. The staff reported that the patient was previously seen in the ED for removal of a vibra- tor from his rectum. -

Foreign Rectal Body – Systematic Review and Meta-Analysis
REVIEW 61 Foreign rectal body – Systematic review and meta-analysis M. Ploner1, A. Gardetto2, F. Ploner3, M. Scharl4, S. Shoap5, H. C. Bäcker5 (1) Department of Anesthesiology and Intensiver Care, Cantonal Spital Lucerne, Lucerne, Switzerland ; (2) Department of Plastic Surgery, Hospital Sterzing, Sterzing, South Tirol, Italy ; (3) Department of Anesthesiology and Emergency Medicine, Hospital Sterzing, South Tirol, Italy ; (4) Department of Gastroenterology and Hepatology, University Hospital Zurich, University of Zurich, Swetzerland ; (5) Department of Orthopaedic Surgery, Columbia University Medical Center, New York, USA. Abstract instrumentation (7). The most common complication is a rectal injury, which can result from a variety of agents and Background : Self-inserted foreign rectal bodies are an objects (8). Often, nonsurgical removal of foreign bodies infrequent occurrence, however they present a serious dilemma to the surgeon, due to the variety of objects, and the difficulty of has been described to be successful – in 11% to 65% – extraction. The purpose of this study is to give a comprehensive (9), however, in many situations, a surgical treatment review of the literature regarding the epidemiology, diagnostic may be essential. There have been a variety of algorithms tools and therapeutic approaches of foreign rectal body insertion. Methods : A comprehensive systematic literature review on introduced for the management of extraction, however, Pubmed/ Medline and Google for ‘foreign bodies’ was performed because of the diversity of foreign bodies, improvisation, on January 14th 2018. A meta-analysis was carried out to evaluate as well creativity of the treating emergency physician the epidemiology, diagnostics and therapeutic techniques. 1,551 abstracts were identified, of which 54 articles were included. -

Abdominal Exploratory and Closure
Abdominal exploratory and closure 10.1 Diagnostic procedures 10.1.1 Paracentesis 10.1.1.1 Paracentesis technique 10.1.2 Enterocentesis 10.1.2.1 Enterocentesis technique 10.2 Opening of the abdominal cavity 10.2.1 Introduction 10.2.2 Position of the animal 10.2.3 Location of incision 10.2.4 Type of incision 10.2.4.1 Through-and-through incision 10.2.4.2 Complete grid Incision 10.2.4.3 Partial grid incision 10.2.5 Laparotomy in the bovine 10.2.5.1 Indications 10.2.5.2 Through-and-through incision 10.2.5.3 Partial grid incision 10.2.5.4 Complete grid incision 10.2.6 Laparotomy in small ruminants Chapter 10 10.2.7 Laparotomy in the horse 10.2.7.1 Indications 10.2.7.2 The median coeliotomy 10.2.7.3 The paramedian laparotomy 10.2.8 Coeliotomy in the dog and the cat 10.2.8.1 Indications 10.2.8.2 The median coeliotomy 10.2.8.3 The flank or paracostal incision 10.3 Minimally invasive techniques 10.4 Abdominal procedures 10.4.1 The rumen (bovine, small ruminants) 10.4.1.1 Introduction 10.4.1.2 Rumenotomy 10.4.2 The abomasum (bovine) 10.4.3 The stomach (horse, dog and cat) 10.4.3.1 Introduction 10.4.3.2 Gastrotomy in the dog and the cat 10.4.4 The small- and large intestines 10.4.4.1 Introduction 10.4.4.1.1 Simple mechanical ileus 10.4.4.1.2 Strangulating ileus 10.4.4.1.3 Paralytic ileus 10.4.4.2 Diagnostics 10.4.4.3 Therapy 10.4.4.3.1 Enterotomy 10.4.4.3.2 Enterectomy 10.4.5 The bladder 10.4.5.1 Introduction 10.4.5.2 Urolithiasis in bovine and equine 10.4.5.3 Cystotomy in the horse 10.4.5.3.1 Laparocystotomy 10.4.5.3.2 Pararectal cystotomy 10.4.5.4 Urolithiasis in the dog and the cat 10.4.5.5 Cystotomy in the dog and the cat 10.4.6 The uterus 10.4.6.1 Opening and closing of the uterus 10.4.6.2 Ovariectomy and ovariohysterectomy in dog and cat Chapter 10 176 Chapter 10 Abdominal exploratory and closure 10.1 Diagnostic procedures 10.1.1 Paracentesis paracentesis Paracentesis is the puncturing of the abdominal cavity.