A Cross-Sectional Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S# BRANCH CODE BRANCH NAME CITY ADDRESS 1 24 Abbottabad
BRANCH S# BRANCH NAME CITY ADDRESS CODE 1 24 Abbottabad Abbottabad Mansera Road Abbottabad 2 312 Sarwar Mall Abbottabad Sarwar Mall, Mansehra Road Abbottabad 3 345 Jinnahabad Abbottabad PMA Link Road, Jinnahabad Abbottabad 4 131 Kamra Attock Cantonment Board Mini Plaza G. T. Road Kamra. 5 197 Attock City Branch Attock Ahmad Plaza Opposite Railway Park Pleader Lane Attock City 6 25 Bahawalpur Bahawalpur 1 - Noor Mahal Road Bahawalpur 7 261 Bahawalpur Cantt Bahawalpur Al-Mohafiz Shopping Complex, Pelican Road, Opposite CMH, Bahawalpur Cantt 8 251 Bhakkar Bhakkar Al-Qaim Plaza, Chisti Chowk, Jhang Road, Bhakkar 9 161 D.G Khan Dera Ghazi Khan Jampur Road Dera Ghazi Khan 10 69 D.I.Khan Dera Ismail Khan Kaif Gulbahar Building A. Q. Khan. Chowk Circular Road D. I. Khan 11 9 Faisalabad Main Faisalabad Mezan Executive Tower 4 Liaqat Road Faisalabad 12 50 Peoples Colony Faisalabad Peoples Colony Faisalabad 13 142 Satyana Road Faisalabad 585-I Block B People's Colony #1 Satayana Road Faisalabad 14 244 Susan Road Faisalabad Plot # 291, East Susan Road, Faisalabad 15 241 Ghari Habibullah Ghari Habibullah Kashmir Road, Ghari Habibullah, Tehsil Balakot, District Mansehra 16 12 G.T. Road Gujranwala Opposite General Bus Stand G.T. Road Gujranwala 17 172 Gujranwala Cantt Gujranwala Kent Plaza Quide-e-Azam Avenue Gujranwala Cantt. 18 123 Kharian Gujrat Raza Building Main G.T. Road Kharian 19 125 Haripur Haripur G. T. Road Shahrah-e-Hazara Haripur 20 344 Hassan abdal Hassan Abdal Near Lari Adda, Hassanabdal, District Attock 21 216 Hattar Hattar -

Usg Humanitarian Assistance to Pakistan in Areas
USG HUMANITARIAN ASSISTANCE TO CONFLICT-AFFECTED POPULATIONS IN PAKISTAN IN FY 2009 AND TO DATE IN FY 2010 Faizabad KEY TAJIKISTAN USAID/OFDA USAID/Pakistan USDA USAID/FFP State/PRM DoD Amu darya AAgriculture and Food Security S Livelihood Recovery PAKISTAN Assistance to Conflict-Affected y Local Food Purchase Populations ELogistics Economic Recovery ChitralChitral Kunar Nutrition Cand Market Systems F Protection r Education G ve Gilgit V ri l Risk Reduction a r Emergency Relief Supplies it a h Shelter and Settlements C e Food For Progress I Title II Food Assistance Shunji gol DHealth Gilgit Humanitarian Coordination JWater, Sanitation, and Hygiene B and Information Management 12/04/09 Indus FAFA N A NWFPNWFP Chilas NWFP AND FATA SEE INSET UpperUpper DirDir SwatSwat U.N. Agencies, E KohistanKohistan Mahmud-e B y Da Raqi NGOs AGCJI F Asadabad Charikar WFP Saidu KUNARKUNAR LowerLower ShanglaShangla BatagramBatagram GoP, NGOs, BajaurBajaur AgencyAgency DirDir Mingora l y VIJaKunar tro Con ImplementingMehtarlam Partners of ne CS A MalakandMalakand PaPa Li Î! MohmandMohmand Kabul Daggar MansehraMansehra UNHCR, ICRC Jalalabad AgencyAgency BunerBuner Ghalanai MardanMardan INDIA GoP e Cha Muzaffarabad Tithwal rsa Mardan dd GoP a a PeshawarPeshawar SwabiSwabi AbbottabadAbbottabad y enc Peshawar Ag Jamrud NowsheraNowshera HaripurHaripur AJKAJK Parachinar ber Khy Attock Punch Sadda OrakzaiOrakzai TribalTribal AreaArea Î! Adj.Adj. PeshawarPeshawar KurrumKurrum AgencyAgency Islamabad Gardez TribalTribal AreaArea AgencyAgency Kohat Adj.Adj. KohatKohat Rawalpindi HanguHangu Kotli AFGHANISTAN KohatKohat ISLAMABADISLAMABAD Thal Mangla reservoir TribalTribal AreaArea AdjacentAdjacent KarakKarak FATAFATA BannuBannu us Bannu Ind " WFP Humanitarian Hub NorthNorth WWaziristanaziristan BannuBannu SOURCE: WFP, 11/30/09 Bhimbar AgencyAgency SwatSwat" TribalTribal AreaArea " Adj.Adj. -

Download FATA Colleges Choices Form
Pre Merit List Merit No. Declaration of Preferences PMC MDCAT Roll No. MBBS/BDS(FATA/MAD SEATS) for Agency/FR. Public Sector Medical Dental Colleges/Institutions Session 2020-21 VERY IMPORTANT: 1.Write your preferences in the order you would like to be considered for admission against the name of College/Institution. 2.Preference once given shall be final and cannot be changed subsequently. Think carefully before writing. 3.Cutting / erasing / over writing is not allowed. 4.The applicant shall never be considered for a college which he/she has not written down in this list of choices. The University shall not assign a college by itself if the alternate choices are not indicated. 5.Khyber Girls Medical College, Peshawar and Fatima Jinnah Medical College, Lahore are for female students only. Male students cannot opt for this college. 6.Candidate who do not submit choices by the deadline i.e. till 02:00 pm on 17/02/2021, the placement committee shall consider his/her choices recorded previously on the already submitted online application form. Name of the Institution/College Choice No. (In Figure and Words) Signatures of the Applicant ADS=Ayub Dental Section, Abbotabad AMC=Ayub Medical College, Abbotabad BKMC=Bacha Khan Medical College, Mardan BKDS=Bacha Khan Dental Secion, Mardan. BMC=Bannu Medical College, Bannu. GKMC = Gajju Khan Medical College Swabi KGMC = Khyber Girls Medical College (For Girls only) GMC = Gomal Medical College KCD = Khyber College of Dentistry KIMS = KMU Institute of Medical Sciences, Kohat KIDS = KMU Institute of Dental Sciences, Kohat KMC = Khyber Medical College Peshawar 1 of 2 Pre Merit List Merit No. -

Recurrent Episcleritis in Children-Less Than 5 Years
J Ayub Med Coll Abbottabad 2006; 18(4) CASE REPORT RECURRENT EPISCLERITIS IN CHILDREN-LESS THAN 5 YEARS OF AGE Syed Ashfaq Ali Shah, Hassan Sajid Kazmi, Abdul Aziz Awan, Jaffar Khan Department of Ophthalmology, Ayub Medical College and teaching Hospital, Abbottabad. Background: Episcleritis , though common in adults, is a rare disease in children. Episcleritis is associated with systemic diseases in a third of cases in adults. Here we describe systemic diseases associated with recurrent episcleritis in children less than five years of age. Method: This Retrospective Observational case series study was conducted at the Department of Ophthalmology of Ayub Teaching Hospital, Abbottabad, from March 1995 till February, 2006. Six children diagnosed clinically with recurrent episcleritis were included in this study. Complete ophthalmologic as well as systemic evaluation was done in each case. Results: This study was conducted on 6 children with a diagnosis of recurrent episcleritis. There were four boys and two girls, with an age range of 35-52 months. Right eye was involved in three cases, left eye in two cases while one case had a bilateral disease. Recurrence occurred in the same eye in all cases, with one bilateral involvement. Four children (66%) had a history of upper respiratory tract infection in the recent past. No other systemic abnormality was detected in any case. Two cases had a history of contact with a pet animal. Conclusion: Recurrent episcleritis in young children is a benign condition. Upper respiratory tract infection is the most common systemic association. Pet animals may be a contributory factor. Keywords: Recurrent Episcleritis, Children, Age, Systemic Disease. -

Health Bulletin July.Pdf
July, 2014 - Volume: 2, Issue: 7 IN THIS BULLETIN HIGHLIGHTS: Polio spread feared over mass displacement 02 English News 2-7 Dengue: Mosquito larva still exists in Pindi 02 Lack of coordination hampering vaccination of NWA children 02 Polio Cases Recorded 8 Delayed security nods affect polio drives in city 02 Combating dengue: Fumigation carried out in rural areas 03 Health Profile: 9-11 U.A.E. polio campaign vaccinates 2.5 million children in 21 areas in Pakistan 03 District Multan Children suffer as Pakistan battles measles epidemic 03 Health dept starts registering IDPs to halt polio spread 04 CDA readies for dengue fever season 05 Maps 12,14,16 Ulema declare polio immunization Islamic 05 Polio virus detected in Quetta linked to Sukkur 05 Articles 13,15 Deaths from vaccine: Health minister suspends 17 officials for negligence 05 Polio vaccinators return to Bara, Pakistan, after five years 06 Urdu News 17-21 Sewage samples polio positive 06 Six children die at a private hospital 06 06 Health Directory 22-35 Another health scare: Two children infected with Rubella virus in Jalozai Camp Norwegian funding for polio eradication increased 07 MULTAN HEALTH FACILITIES ADULT HEALTH AND CARE - PUNJAB MAPS PATIENTS TREATED IN MULTAN DIVISION MULTAN HEALTH FACILITIES 71°26'40"E 71°27'30"E 71°28'20"E 71°29'10"E 71°30'0"E 71°30'50"E BUZDAR CLINIC TAYYABA BISMILLAH JILANI Rd CLINIC AMNA FAMILY il BLOOD CLINIC HOSPITAL Ja d M BANK R FATEH MEDICAL MEDICAL NISHTER DENTAL Legend l D DENTAL & ORAL SURGEON a & DENTAL STORE MEDICAL COLLEGE A RABBANI n COMMUNITY AND HOSPITAL a CLINIC R HOSPITALT C HEALTH GULZAR HOSPITAL u "' Basic Health Unit d g CENTER NAFEES MEDICARE AL MINHAJ FAMILY MULTAN BURN UNIT PSYCHIATRIC h UL QURAN la MATERNITY HOME CLINIC ZAFAR q op Blood Bank N BLOOD BANK r ishta NIAZ CLINIC R i r a Rd X-RAY SIYAL CLINIC d d d SHAHAB k a Saddiqia n R LABORATORY FAROOQ k ÷Ó o Children Hospital d DECENT NISHTAR a . -

Complications of Cataract Surgery in Patients with Pseudoexfoliation
J Ayub Med Coll Abbottabad 2009;21(2) COMPLICATIONS OF CATARACT SURGERY IN PATIENTS WITH PSEUDOEXFOLIATION SYNDROME Mohammad Jawad, Aqil-ur-Rehman Nadeem, Aleem ul Haq Khan*, Mohammad Aftab Department of Ophthalmology, *Department of Biochemistry, Women Medical College, Abbottabad, Pakistan Background: The weak zonule’s predisposition to complications during conventional cataract surgery is one of the common risk factor for poor visual acuity after surgery. The present study was conducted to determine the frequency and types of complications during cataract surgery in patients with Pseudoexfoliation Syndrome. Methods: A cross sectional descriptive study based on non probability sampling of patients having pseudoexfoliation syndrome admitted for cataract surgery in tertiary care hospitals was carried out spread over 4 years. The data of all variables of interest were entered and analyzed through SPSS version 15.0. Results: A total of 200 eyes of 122 patients having Psuedoexfoliation were included in the study. Vitreal prolapse in 21 (10.5%) and posterior capsular rupture in 18 (9%) patients were the most common complications seen in Pseudoexfoliation. Damage to sphincter pupillae in 16 (8%), iridodialysis in 2 (1%), decentration of IOL in 8 (4%) and hyphaema in 2 (1%) patients was seen. Zonular dialysis in 8 (4%), retained lens matter in 12 (6%) and lens dislocation was seen in 6 (3%) patients. Conclusion: Patients with pseudoexfoliation are at increased risk for development of complications. Ophthalmologists should stress to increase awareness among general public for the proper diagnosis and convince patients for proper and regular follow up visits to the hospital. Keywords: Pseudoexfoliation, Cataract, Complications, Intraocular pressure INTRODUCTION Multiple factors contribute to the development of 1 pseudoexfoliation syndrome. -

Abbreviations and Acronyms
P ART III] THE GAZETTE OF PAKISTAN, EXTRA., FEBRUARY 12, 2019 259 ISLAMABAD, TUESDAY, FEBRUARY 12, 2019 PART III Other Notifications, Orders, etc. ELECTION COMMISSION OF PAKISTAN NOTIFICATIONS Islamabad, the 31st January, 2019 SUBJECT:— NOTIFICATION OF RETURNED CANDIDATES TO THE VACANT SEATS OF NAZIM / NAIB NAZIM IN VARIOUS LOCAL COUNCILS OF KP PROVINCE. No. F. 23(1)/2018-LGE-KPK(Vol-IV)(1).—WHEREAS, under Rule-70 (6) of the Khyber Pakhtunkhwa Local Councils (Conduct of Elections) Rules 2014, the Returning Officers, appointed for the conduct of Election to the seats of Nazim/ Naib Nazim of Local Councils concerned, have declared the names of the members commanding the confidence of the majority of members of the Local Council concerned. NOW THEREFORE, in exercise of powers conferred upon it under Article 140A (2) of the Constitution of the Islamic Republic of Pakistan, Section-86 of Khyber Pakhtunkhwa Local Government Act, 2013 and all other powers (259) Price: Rs. 10.00 [220(2019)/Ex.Gaz.] 260 THE GAZETTE OF PAKISTAN, EXTRA., FEBRUARY 12, 2019 [PART III enabling it in that behalf, the Election Commission of Pakistan hereby notifies hereunder, for information of public, the names of returned candidates against the seats of Nazim/ Naib Nazim of various Local Councils concerned elected during the Election held on 21st January, 2019:— Votes Name of Name of Category Obtained/ S.No. Returned Father Name Address Council of Seat Total candidate Votes DISTRICT PESHAWAR Muhammad Town Naib Urmar Bala, 1 Hazrat Gul 24/31 Zafar Council-IV Nazim Peshawar NC-280 Naib Achini Payan, 2 Islam Shah Rahim Shah 7/12 Achini Payan Nazim Peshawar VC 174, Suleman Khel, 3 Islam Khan Dawlat Khan Nazim 8/12 Suleman Khel Peshawar Kochian P.O. -

MBBS / BDS ADMISSIONS Government Medical Colleges of Azad Jammu & Kashmir (AJ&K) and Reserved Seats for AJ&K Nationals in Pakistan, Session 2019-2020
University of Health Sciences Lahore MBBS / BDS ADMISSIONS Government Medical Colleges of Azad Jammu & Kashmir (AJ&K) and Reserved Seats for AJ&K Nationals in Pakistan, Session 2019-2020 Online applications are invited from eligible (First Class State Subject) candidates for admissions in First Year MBBS and BDS against reserved seats for AJ&K Nationals, Refugees 1947and Refugees 1989 (conditions apply), in the following Public Sector Medical/Dental Colleges of Pakistan (Punjab, Khyber Pakhtunkhwa, Balochistan & Sindh) and Public Sector Medical Colleges of AJ&K. Admissions will be made strictly on merit basis as per PM&DC Admission Regulations and Admission Policy of AJ&K Government in vogue: Medical/Dental Institutions of Pakistan Punjab (MBBS) Khyber Pakhtunkhwa (MBBS) Allama Iqbal Medical University Lahore Ayub Medical College Abbottabad Fatima Jinnah Medical University Lahore Gomal Medical College D.I Khan King Edward Medical University Lahore Khyber Medical University Peshawar Nishtar Medical University Multan Saidu Sharif Medical College Swat Punjab Medical University Faisalabad Khyber Pakhtunkhwa (BDS) Quaid e Azam Medical College Bahawalpur Dental Unit Ayub Medical College Abbottabad Rawalpindi Medical University Rawalpindi Sindh (MBBS) Services Institute of Medical Sciences Lahore Chandka Medical College Larkana Sheikh Zayad Medical College Rahim Yar Khan Balochistan (MBBS) Punjab (BDS) Bolan Medical College Quetta de’Montmorency College of Dentistry Lahore Medical Institutions of AJ&K Azad Jammu Kashmir Medical College Muzaffarabad Mohtarma Be’Nazir Bhutto Shaheed Medical College Mirpur Poonch Medical College Rawalakot 1. ELIGIBILITY CRITERIA i) Qualifications: In accordance with “MBBS and BDS (Admissions, House Job and Internship) Regulations, 2018, as amended on 30th May, 2019” of Pakistan Medical and Dental Council, the required qualifications for admissions are as follows: The applicant has passed, obtaining minimum Seventy percent (770/1100) marks, in Higher Secondary School Certificate (HSSC) or F.Sc. -

Role of Chest Imaging in Diagnosis and Management of COVID-19
DISCOVERIES REPORTS 2021, 4: e20 10.15190/drep.2021.5 Chest Imaging and COVID-19 DOI: REVIEW Article Role of Chest Imaging in Diagnosis and Management of COVID-19 Madeeha Subhan Waleed1,*, Kinal Paresh Bhatt2, Farwah N. Fatima3, Anoopa Mathew4, Paz Ines M. Domingo5, Mehrie H. Patel6, Bishnu M. Singh7 1Ayub Medical College, 22040, Abbottabad, Pakistan 2Larkin Health System, 33143, South Miami, FL, USA 3Lahore Medical and Dental College,53400, Lahore, Pakistan 4K.S. Hegde Medical Academy, 575018, Mangaluru, Karnataka, India 5University of the East Ramon Magsaysay Memorial Medical Center, 1113, Quezon City, Philippines 6Pramukhswami Medical College, 388325, Gujarat, India 7Hetauda City Hospital, 44107, Hetauda, Nepal * Corresponding authors: Madeeha Subhan Waleed MBBS, Ayub Medical College, 22040, Abbottabad, Pakistan; Email: [email protected]; Phone:00923335634888. Submitted: Mar. 31, 2021; Revised: May 08, 2021; Accepted: May 08, 2021; Published: June 30, 2021; Citation: Waleed MS, Bhatt KP, Fatima FN, Mathew A, Domingo PIM, Patel MH, Singh BM. Role of Chest Imaging in Diagnosis and Management of COVID-19. Discoveries Reports, 2021; 4: e20. DOI: 10.15190/drep.2021.5 ABSTRACT mounting prevalence of COVID-19 in the The COVID-19 pandemic is a serious global health community demands for an accurate and sensitive threat. The standard gold test for detecting COVID - test for COVID-19. This review article sheds light 19 is a real-time reverse transcription-polymerase on the limited role of different imaging modalities in chain reaction (RT-PCR) of viral nucleic acid. There diagnosing and managing COVID-19. are different specific and nonspecific diagnostic tests available for COVID-19. -

Reclaiming Prosperity in Khyber- Pakhtunkhwa
Working paper Reclaiming Prosperity in Khyber- Pakhtunkhwa A Medium Term Strategy for Inclusive Growth Full Report April 2015 When citing this paper, please use the title and the following reference number: F-37109-PAK-1 Reclaiming Prosperity in Khyber-Pakhtunkhwa A Medium Term Strategy for Inclusive Growth International Growth Centre, Pakistan Program The International Growth Centre (IGC) aims to promote sustainable growth in developing countries by providing demand-led policy advice informed by frontier research. Based at the London School of Economics and in partnership with Oxford University, the IGC is initiated and funded by DFID. The IGC has 15 country programs. This report has been prepared under the overall supervision of the management team of the IGC Pakistan program: Ijaz Nabi (Country Director), Naved Hamid (Resident Director) and Ali Cheema (Lead Academic). The coordinators for the report were Yasir Khan (IGC Country Economist) and Bilal Siddiqi (Stanford). Shaheen Malik estimated the provincial accounts, Sarah Khan (Columbia) edited the report and Khalid Ikram peer reviewed it. The authors include Anjum Nasim (IDEAS, Revenue Mobilization), Osama Siddique (LUMS, Rule of Law), Turab Hussain and Usman Khan (LUMS, Transport, Industry, Construction and Regional Trade), Sarah Saeed (PSDF, Skills Development), Munir Ahmed (Energy and Mining), Arif Nadeem (PAC, Agriculture and Livestock), Ahsan Rana (LUMS, Agriculture and Livestock), Yasir Khan and Hina Shaikh (IGC, Education and Health), Rashid Amjad (Lahore School of Economics, Remittances), GM Arif (PIDE, Remittances), Najm-ul-Sahr Ata-ullah and Ibrahim Murtaza (R. Ali Development Consultants, Urbanization). For further information please contact [email protected] , [email protected] , [email protected] . -

Outcome of Traumatic Brain Injury in Children by Using Rotterdam Score on Computed Tomography
eCommons@AKU Department of Paediatrics and Child Health Division of Woman and Child Health 1-2018 Outcome of traumatic brain injury in children by using rotterdam score on computed tomography Anwarul Haque Aga Khan University, [email protected] Zehra Dhanani Aga Khan University Amin Ali Aga Khan University, [email protected] Basit Salam Aga Khan University, [email protected] Qalab Abbas Aga Khan University, [email protected] See next page for additional authors Follow this and additional works at: https://ecommons.aku.edu/ pakistan_fhs_mc_women_childhealth_paediatr Part of the Neurology Commons, and the Pediatrics Commons Recommended Citation Haque, A., Dhanani, Z., Ali, A., Salam, B., Abbas, Q., Javed, G., Jurair, H. (2018). Outcome of traumatic brain injury in children by using rotterdam score on computed tomography. Journal of Ayub Medical College, Abbottabad:JAMC, 30(1), 140-142. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_women_childhealth_paediatr/308 Authors Anwarul Haque, Zehra Dhanani, Amin Ali, Basit Salam, Qalab Abbas, Gohar Javed, and Humaira Jurair This article is available at eCommons@AKU: https://ecommons.aku.edu/ pakistan_fhs_mc_women_childhealth_paediatr/308 J Ayub Med Coll Abbottabad 2018;30(1) SHORT COMMUNICATION OUTCOME OF TRAUMATIC BRAIN INJURY IN CHILDREN BY USING ROTTERDAM SCORE ON COMPUTED TOMOGRAPHY Anwarul Haque, Zehra Dhanani, Amin Ali, Basit Salam*, Qalab Abbas, Gohar Javed, Humaira Jurair Department of Paediatrics and Child Health, *Department of Radiology, Department of Neuro-Surgery Aga Khan University Hospital, Karachi-Pakistan Background: The Rotterdam Score (RS) on CT head is a new evolving clinical tool as a predictor of mortality in Traumatic Brain Injury (TBI). The objective of this study is to assess the outcome of children with TBI admitted in paediatric intensive care unit (PICU) of a tertiary-care, university hospital by using RS. -
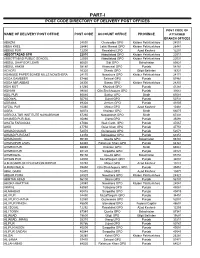
Part-I: Post Code Directory of Delivery Post Offices
PART-I POST CODE DIRECTORY OF DELIVERY POST OFFICES POST CODE OF NAME OF DELIVERY POST OFFICE POST CODE ACCOUNT OFFICE PROVINCE ATTACHED BRANCH OFFICES ABAZAI 24550 Charsadda GPO Khyber Pakhtunkhwa 24551 ABBA KHEL 28440 Lakki Marwat GPO Khyber Pakhtunkhwa 28441 ABBAS PUR 12200 Rawalakot GPO Azad Kashmir 12201 ABBOTTABAD GPO 22010 Abbottabad GPO Khyber Pakhtunkhwa 22011 ABBOTTABAD PUBLIC SCHOOL 22030 Abbottabad GPO Khyber Pakhtunkhwa 22031 ABDUL GHAFOOR LEHRI 80820 Sibi GPO Balochistan 80821 ABDUL HAKIM 58180 Khanewal GPO Punjab 58181 ACHORI 16320 Skardu GPO Gilgit Baltistan 16321 ADAMJEE PAPER BOARD MILLS NOWSHERA 24170 Nowshera GPO Khyber Pakhtunkhwa 24171 ADDA GAMBEER 57460 Sahiwal GPO Punjab 57461 ADDA MIR ABBAS 28300 Bannu GPO Khyber Pakhtunkhwa 28301 ADHI KOT 41260 Khushab GPO Punjab 41261 ADHIAN 39060 Qila Sheikhupura GPO Punjab 39061 ADIL PUR 65080 Sukkur GPO Sindh 65081 ADOWAL 50730 Gujrat GPO Punjab 50731 ADRANA 49304 Jhelum GPO Punjab 49305 AFZAL PUR 10360 Mirpur GPO Azad Kashmir 10361 AGRA 66074 Khairpur GPO Sindh 66075 AGRICULTUR INSTITUTE NAWABSHAH 67230 Nawabshah GPO Sindh 67231 AHAMED PUR SIAL 35090 Jhang GPO Punjab 35091 AHATA FAROOQIA 47066 Wah Cantt. GPO Punjab 47067 AHDI 47750 Gujar Khan GPO Punjab 47751 AHMAD NAGAR 52070 Gujranwala GPO Punjab 52071 AHMAD PUR EAST 63350 Bahawalpur GPO Punjab 63351 AHMADOON 96100 Quetta GPO Balochistan 96101 AHMADPUR LAMA 64380 Rahimyar Khan GPO Punjab 64381 AHMED PUR 66040 Khairpur GPO Sindh 66041 AHMED PUR 40120 Sargodha GPO Punjab 40121 AHMEDWAL 95150 Quetta GPO Balochistan 95151