Autoimmune Diseases in Patients with Premature Ovarian Insufficiency—Our Current State of Knowledge
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Premature Ovarian Insufficiency
biomedicines Review Premature Ovarian Insufficiency: Procreative Management and Preventive Strategies Jennifer J. Chae-Kim 1 and Larisa Gavrilova-Jordan 2,* 1 Department of Obstetrics and Gynecology, East Carolina University, Greenville, NC 27834, USA; [email protected] 2 Department of Obstetrics and Gynecology, Augusta University, Augusta, GA 30912, USA * Correspondence: [email protected]; Tel.: +1-706-721-3832 Received: 30 November 2018; Accepted: 24 December 2018; Published: 28 December 2018 Abstract: Premature ovarian insufficiency (POI) is the loss of normal hormonal and reproductive function of ovaries in women before age 40 as the result of premature depletion of oocytes. The incidence of POI increases with age in reproductive-aged women, and it is highest in women by the age of 40 years. Reproductive function and the ability to have children is a defining factor in quality of life for many women. There are several methods of fertility preservation available to women with POI. Procreative management and preventive strategies for women with or at risk for POI are reviewed. Keywords: premature ovarian insufficiency; in vitro fertilization; donor oocyte; fertility preservation 1. Introduction Premature ovarian insufficiency (POI) is the loss of normal hormonal and reproductive function of ovaries in women before age 40 as the result of premature depletion of oocytes. POI is characterized by elevated gonadotrophin levels, hypoestrogenism, and amenorrhea, occurring years before the average age of menopause. Previously referred to as ovarian failure or early menopause, POI is now understood to be a condition that encompasses a range of impaired ovarian function, with clinical implications overlapping but not synonymous to that of physiologic menopause. -

Sex Hormones Related Ocular Dryness in Breast Cancer Women
Journal of Clinical Medicine Review Sex Hormones Related Ocular Dryness in Breast Cancer Women Antonella Grasso 1, Antonio Di Zazzo 2,* , Giuseppe Giannaccare 3 , Jaemyoung Sung 4 , Takenori Inomata 4 , Kendrick Co Shih 5 , Alessandra Micera 6, Daniele Gaudenzi 2, Sara Spelta 2 , Maria Angela Romeo 7, Paolo Orsaria 1, Marco Coassin 2 and Vittorio Altomare 1 1 Breast Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (A.G.); [email protected] (P.O.); [email protected] (V.A.) 2 Ophthalmology Operative Complex Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (D.G.); [email protected] (S.S.); [email protected] (M.C.) 3 Department of Ophthalmology, University Magna Graecia of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of Ophthalmology, School of Medicine, Juntendo University, 1130033 Tokyo, Japan; [email protected] (J.S.); [email protected] (T.I.) 5 Department of Ophthalmology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; [email protected] 6 Research and Development Laboratory for Biochemical, Molecular and Cellular Applications in Ophthalmological Sciences, IRCCS–Fondazione Bietti, 00198 Rome, Italy; [email protected] 7 School of Medicine, Humanitas University, 20089 Milan, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-06225418893; Fax: +39-9622541456 Abstract: Background: Dry eye syndrome (DES) is strictly connected to systemic and topical sex hor- mones. Breast cancer treatment, the subsequent hormonal therapy, the subsequent hyperandrogenism and the early sudden menopause, may be responsible for ocular surface system failure and its clinical Citation: Grasso, A.; Di Zazzo, A.; manifestation as dry eye disease. -

Androgen Excess in Breast Cancer Development: Implications for Prevention and Treatment
26 2 Endocrine-Related G Secreto et al. Androgen excess in breast 26:2 R81–R94 Cancer cancer development REVIEW Androgen excess in breast cancer development: implications for prevention and treatment Giorgio Secreto1, Alessandro Girombelli2 and Vittorio Krogh1 1Epidemiology and Prevention Unit, Fondazione IRCCS – Istituto Nazionale dei Tumori, Milano, Italy 2Anesthesia and Critical Care Medicine, ASST – Grande Ospedale Metropolitano Niguarda, Milano, Italy Correspondence should be addressed to G Secreto: [email protected] Abstract The aim of this review is to highlight the pivotal role of androgen excess in the Key Words development of breast cancer. Available evidence suggests that testosterone f breast cancer controls breast epithelial growth through a balanced interaction between its two f ER-positive active metabolites: cell proliferation is promoted by estradiol while it is inhibited by f ER-negative dihydrotestosterone. A chronic overproduction of testosterone (e.g. ovarian stromal f androgen/estrogen balance hyperplasia) results in an increased estrogen production and cell proliferation that f androgen excess are no longer counterbalanced by dihydrotestosterone. This shift in the androgen/ f testosterone estrogen balance partakes in the genesis of ER-positive tumors. The mammary gland f estradiol is a modified apocrine gland, a fact rarely considered in breast carcinogenesis. When f dihydrotestosterone stimulated by androgens, apocrine cells synthesize epidermal growth factor (EGF) that triggers the ErbB family receptors. These include the EGF receptor and the human epithelial growth factor 2, both well known for stimulating cellular proliferation. As a result, an excessive production of androgens is capable of directly stimulating growth in apocrine and apocrine-like tumors, a subset of ER-negative/AR-positive tumors. -
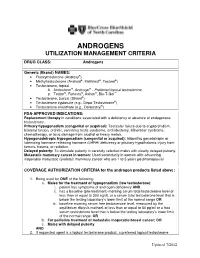
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

Serum Androgen Profiles in Women with Premature Ovarian Insufficiency: a Systematic Review and Meta-Analysis
Menopause: The Journal of The North American Menopause Society Vol. 26, No. 1, pp. 78-93 DOI: 10.1097/GME.0000000000001161 ß 2018 The Author(s). Published by Wolters Kluwer Health, Inc. on behalf of The North American Menopause Society. Serum androgen profiles in women with premature ovarian insufficiency: a systematic review and meta-analysis Midhun Soman, MS,1 Li-Cong Huang, MD,1 Wen-Hui Cai, MS,1 Jun-Bi Xu, MS,1 Jun-Yao Chen, MD,1 Ren-Ke He, MS,1 Heng-Chao Ruan, MS,1,2,3 Xiang-Rong Xu, MD,1,2,3 Zhi-Da Qian, MD,1,2,3,4 and Xiao-Ming Zhu, MD, PhD1,2,3 Abstract Objective: This meta-analysis aims to investigate serum androgen profiles (testosterone, dehydroepiandroster- one sulfate, androstenedione, and sex hormone-binding globulin) in women with premature ovarian failure and to establish if there is evidence of diminished androgen levels in these women. Methods: Various Internet sources of PubMed, Cochrane library, and Medline were searched systematically until February, 2018. Out of a pool of 2,461 studies, after applying the inclusion/exclusion criterion, 14, 8, 10, and 9 studies were chosen for testosterone, dehydroepiandrosterone sulfate, androstenedione, and sex hormone-binding globulin, respectively, for this meta-analysis. The effect measure was the standardized mean difference with 95% confidence interval (95% CI) in a random-effects model. Results: The testosterone concentrations in premature ovarian insufficiency were compared with fertile controls: stamdard mean difference (IV, random, 95% CI) À0.73 [À0.99, À0.46], P value < 0.05. The dehydroepiandrosterone sulfate concentrations in premature ovarian insufficiency compared to fertile controls: standard mean difference (IV, random, 95% CI) À0.65 [À0.92, À0.37], P value < 0.05. -

A Case of Malignant Insulinoma Responsive to Somatostatin Analogs
Caliri et al. BMC Endocrine Disorders (2018) 18:98 https://doi.org/10.1186/s12902-018-0325-4 CASE REPORT Open Access A case of malignant insulinoma responsive to somatostatin analogs treatment Mariasmeralda Caliri1†, Valentina Verdiani1†, Edoardo Mannucci2, Vittorio Briganti3, Luca Landoni4, Alessandro Esposito4, Giulia Burato5, Carlo Maria Rotella2, Massimo Mannelli1 and Alessandro Peri1* Abstract Background: Insulinoma is a rare tumour representing 1–2% of all pancreatic neoplasms and it is malignant in only 10% of cases. Locoregional invasion or metastases define malignancy, whereas the dimension (> 2 cm), CK19 status, the tumor staging and grading (Ki67 > 2%), and the age of onset (> 50 years) can be considered elements of suspect. Case presentation: We describe the case of a 68-year-old man presenting symptoms compatible with hypoglycemia. The symptoms regressed with food intake. These episodes initially occurred during physical activity, later also during fasting. The fasting test was performed and the laboratory results showed endogenous hyperinsulinemia compatible with insulinoma. The patient appeared responsive to somatostatin analogs and so he was treated with short acting octreotide, obtaining a good control of glycemia. Imaging investigations showed the presence of a lesion of the uncinate pancreatic process of about 4 cm with a high sst2 receptor density. The patient underwent exploratory laparotomy and duodenocephalopancreasectomy after one month. The definitive histological examination revealed an insulinoma (T3N1MO, AGCC VII G1) with a low replicative index (Ki67: 2%). Conclusions: This report describes a case of malignant insulinoma responsive to octreotide analogs administered pre- operatively in order to try to prevent hypoglycemia. The response to octreotide analogs is not predictable and should be initially assessed under strict clinical surveillance. -

Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’S Time to Sound the Alarm
Review Article Health promotion, disease prevention, and lifestyle pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health 2020 Jul 38(3): 323-337 https://doi.org/10.5534/wjmh.200012 Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’s Time to Sound the Alarm Abdulmaged M. Traish Department of Urology, Boston University School of Medicine, Boston, MA, USA 5α-dihydrotestosterone (5α-DHT) is the most potent natural androgen. 5α-DHT elicits a multitude of physiological actions, in a host of tissues, including prostate, seminal vesicles, hair follicles, skin, kidney, and lacrimal and meibomian glands. How- ever, the physiological role of 5α-DHT in human physiology, remains questionable and, at best, poorly appreciated. Recent emerging literature supports a role for 5α-DHT in the physiological function of liver, pancreatic β-cell function and survival, ocular function and prevention of dry eye disease and kidney physiological function. Thus, inhibition of 5α-reductases with finasteride or dutasteride to reduce 5α-DHT biosynthesis in the course of treatment of benign prostatic hyperplasia (BPH) or male pattern hair loss, known as androgenetic alopecia (AGA) my induces a novel form of tissue specific androgen deficien- cy and contributes to a host of pathophysiological conditions, that are yet to be fully recognized. Here, we advance the con- cept that blockade of 5α-reductases by finasteride or dutasteride in a mechanism-based, irreversible, inhabitation of 5α-DHT biosynthesis results in a novel state of androgen deficiency, independent of circulating testosterone levels. Finasteride and dutasteride are frequently prescribed for long-term treatment of lower urinary tract symptoms in men with BPH and in men with AGA. -

Menstrual Disorders Susan Hayden Gray, MD* Practice Gap 1
Article genital system disorders Menstrual Disorders Susan Hayden Gray, MD* Practice Gap 1. Dysmenorrhea, amenorrhea, and abnormal vaginal bleeding affect the majority of Author Disclosure adolescent females, impacting quality of life and school attendance. Patient-centered Dr Gray has disclosed adolescent care should include searching for, assessing, and managing menstrual concerns. no financial 2. Polycystic ovary syndrome (PCOS) is the most common endocrinopathy in young relationships relevant adult women, and pediatricians should recognize, monitor, educate, and manage their to this article. This patients who fit the medical profile for PCOS based on any/all of the three sets of commentary does diagnostic criteria. contain a discussion of an unapproved/ Objectives After reading this article, readers should be able to: investigative use of a commercial product/ 1. Define primary and secondary amenorrhea and list the differential diagnosis for each. device. 2. Recognize the importance of a sensitive urine pregnancy test early in the evaluation of menstrual disorders, regardless of stated sexual history. 3. Know that polycystic ovary syndrome is a common cause of secondary amenorrhea in adolescents and may present with oligomenorrhea or abnormal uterine bleeding. 4. Recognize that eating disordered behaviors are a common cause of secondary amenorrhea and irregular bleeding, and treatment of the eating disordered behavior is the best recommendation to ensure resumption of regular menses and long-term bone health. 5. Know the differential diagnosis of abnormal uterine bleeding and describe the preferred treatment, recognizing the central importance of iron replacement. 6. Understand the prevalence of primary dysmenorrhea and its role in causing recurrent school absence in young women, and describe its evaluation and management. -

Estrogen Deficiency During Menopause and Its Management: a Current Update V
Review Article Estrogen deficiency during menopause and its management: A current update V. T. Hemalatha1, A. Julius2, S. P. Kishore Kumar3, L. Vijayalakshmi4, Shankar Narayanan1 ABSTRACT Different phases of a woman’s life: Puberty, menses, pregnancy, and menopause have varied influence on her oral health. During the menopause, women go through biological and endocrine changes, particularly in their sex steroid hormone production, affecting their health. Sex hormones strongly influence body fat distribution and adipocyte differentiation. Estrogens and testosterone differentially affect adipocyte physiology, but the importance of estrogens in the development of metabolic diseases during menopause is disputed. Estrogens and estrogens receptor regulate various aspects of glucose and lipid metabolism. Disturbances of this metabolic signal lead to the development of metabolic syndrome and a higher cardiovascular risk in woman. The absence of estrogens is a clue factor in the onset of cardiovascular disease during the menopausal period, which is characterized by lipid profile variations and predominant abdominal fat accumulation. However, influence of the absence of these hormones and its relationship to higher obesity in women during menopause is not clear. This systematic review discusses of the role of estrogens and estrogen receptors in adipocyte differentiation and its various effects and brief discussion on its management. KEY WORDS: Estrogen hormone (estrogens/progestogens) replacement therapy, Menopause, Weight gain INTRODUCTION BODY CHANGES AT MENOPAUSE Menopause occurs when a woman stops ovulating and As we age, our muscles decrease in bulk and our her monthly period (menstruation) stops. metabolism slows down. These changes cancontribute to weight gain around the time of menopause. Other As women age, into their 40s and 50s, there is a tendency physical changes associated with menopause may to gain weight. -

AMENORRHOEA Amenorrhoea Is the Absence of Menses in a Woman of Reproductive Age
AMENORRHOEA Amenorrhoea is the absence of menses in a woman of reproductive age. It can be primary or secondary. Secondary amenorrhoea is absence of periods for at least 3 months if the patient has previously had regular periods, and 6 months if she has previously had oligomenorrhoea. In contrast, oligomenorrhoea describes infrequent periods, with bleeds less than every 6 weeks but at least one bleed in 6 months. Aetiology of amenorrhea in adolescents (from Golden and Carlson) Oestrogen- Oestrogen- Type deficient replete Hypothalamic Eating disorders Immaturity of the HPO axis Exercise-induced amenorrhea Medication-induced amenorrhea Chronic illness Stress-induced amenorrhea Kallmann syndrome Pituitary Hyperprolactinemia Prolactinoma Craniopharyngioma Isolated gonadotropin deficiency Thyroid Hypothyroidism Hyperthyroidism Adrenal Congenital adrenal hyperplasia Cushing syndrome Ovarian Polycystic ovary syndrome Gonadal dysgenesis (Turner syndrome) Premature ovarian failure Ovarian tumour Chemotherapy, irradiation Uterine Pregnancy Androgen insensitivity Uterine adhesions (Asherman syndrome) Mullerian agenesis Cervical agenesis Vaginal Imperforate hymen Transverse vaginal septum Vaginal agenesis The recommendations for those who should be evaluated have recently been changed to those shown below. (adapted from Diaz et al) Indications for evaluation of an adolescent with primary amenorrhea 1. An adolescent who has not had menarche by age 15-16 years 2. An adolescent who has not had menarche and more than three years have elapsed since thelarche 3. An adolescent who has not had a menarche by age 13-14 years and no secondary sexual development 4. An adolescent who has not had menarche by age 14 years and: (i) there is a suspicion of an eating disorder or excessive exercise, or (ii) there are signs of hirsutism, or (iii) there is suspicion of genital outflow obstruction Pregnancy must always be excluded. -

Type 1 Diabetes and Celiac Disease: Overview and Medical Nutrition Therapy
Nutrition FYI Type 1 Diabetes and Celiac Disease: Overview and Medical Nutrition Therapy Sarah Jane Schwarzenberg, MD, and Carol Brunzell, RD, CDE In patients with celiac disease (gluten- problems recognized only retrospec- glycemia, but only several months sensitive enteropathy, or GSE), inges- tively as resulting from celiac disease; after initiation. tion of the gliadin fraction of wheat it is common for “asymptomatic” It seems likely that a malabsorp- gluten and similar molecules (pro- patients to report improved health or tive disease could create opportunity lamins) from barley, rye, and possibly sense of well-being when following a for hypoglycemia in diabetes, partic- oats causes damage to the intestinal gluten-free diet. Up to one-third of ularly in patients under tight control. epithelium. The injury results from an patients may have unexplained failure Serological testing for GSE in abnormal T-cell response against to thrive, abdominal pain, or short patients with type 1 diabetes, with gliadin. Thus, GSE is a disease in stature.3,6 early diagnosis of GSE, may reduce which host susceptibility must be More controversial is the question this risk by allowing patients to be combined with a specific environmen- of whether GSE affects blood glucose diagnosed in a pre-symptomatic tal trigger to affect injury.1 control. A study by Acerini et al.7 in a state. It also seems prudent to closely Typically, patients with GSE have type 1 diabetic population found no monitor insulin needs and blood glu- chronic diarrhea and failure to thrive. difference between the celiac and non- cose control during the early phase of However, some patients present with celiac subpopulation in terms of instituting a gluten-free diet. -

The Role of Autoimmunity in Premature Ovarian Failure
Iran J Reprod Med Vol. 13. No. 8. pp: 461-472, August 2015 Review article The role of autoimmunity in premature ovarian failure Mahbod Ebrahimi M.D., Firouzeh Akbari Asbagh M.D. Department of Obstetrics and Abstract Gynecology, Moheb-e-Yas Women General Hospital, Faculty of Premature ovarian failure (POF) is a heterogeneous syndrome with several causative Medicine, Tehran University of factors. Autoimmune mechanisms are involved in pathogenesis of 4-30 % of POF Medical Sciences and Health cases. The present review focuses on the role of autoimmunity in the Services, Tehran, Iran. pathophysiology of POF. The evidences for an autoimmune etiology are: demonstration of ovarian autoantibodies, the presence of lymphocytic oophoritis, and association with other autoimmune disorders. Several ovarian antigenic targets have been identified in POF patients. The oocyte seems to be the most often targeted cell. Lymphocytic oophoritis is widely present in POF associated adrenal s disease is one of the most common autoimmune disordersۥinsufficiency. Addison associated with POF. Early detection of this potentially life threatening disease was recommended in several studies. The gold standard for detecting autoimmune POF is ovarian biopsy. This procedure is not recommended due to unknown clinical value, expense, and risks. Several immunoassays have been proposed as substitute diagnostic tools. Nevertheless, there is no clinically proven sensitive and specific serum test to confirm the diagnosis of autoimmune POF or to anticipate the patient’s chance of developing POF or Corresponding Author: Mahbod Ebrahimi,, Department of associated diseases. Obstetrics and Gynecology, Some authors suggested the possible effects of immuno-modulating therapy on the Moheb-e-Yas Women General resumption of ovarian function and fertility in a selected group of autoimmune POF Hospital, North Oustad Nejatollahi patients.