Managing Constipation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inflammatory Bowel Disease Irritable Bowel Syndrome
Inflammatory Bowel Disease and Irritable Bowel Syndrome Similarities and Differences 2 www.ccfa.org IBD Help Center: 888.MY.GUT.PAIN 888.694.8872 Important Differences Between IBD and IBS Many diseases and conditions can affect the gastrointestinal (GI) tract, which is part of the digestive system and includes the esophagus, stomach, small intestine and large intestine. These diseases and conditions include inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). IBD Help Center: 888.MY.GUT.PAIN 888.694.8872 www.ccfa.org 3 Inflammatory bowel diseases are a group of inflammatory conditions in which the body’s own immune system attacks parts of the digestive system. Inflammatory Bowel Disease Inflammatory bowel diseases are a group of inflamma- Causes tory conditions in which the body’s own immune system attacks parts of the digestive system. The two most com- The exact cause of IBD remains unknown. Researchers mon inflammatory bowel diseases are Crohn’s disease believe that a combination of four factors lead to IBD: a (CD) and ulcerative colitis (UC). IBD affects as many as 1.4 genetic component, an environmental trigger, an imbal- million Americans, most of whom are diagnosed before ance of intestinal bacteria and an inappropriate reaction age 35. There is no cure for IBD but there are treatments to from the immune system. Immune cells normally protect reduce and control the symptoms of the disease. the body from infection, but in people with IBD, the immune system mistakes harmless substances in the CD and UC cause chronic inflammation of the GI tract. CD intestine for foreign substances and launches an attack, can affect any part of the GI tract, but frequently affects the resulting in inflammation. -

Guideline for Dietary Fibre Intake
Guideline for dietary fibre intake Gezondheidsraad Health Council of the Netherlands To the Minister of Health, Welfare and Sport Subject : Presentation of advisory report Guideline for dietary fibre intake Your reference:- Our reference : U 383/CS/cn/754-C Enclosures : 1 Date : March 21, 2006 Dear Minister, I hereby present an advisory report concerning the Guideline for Dietary Fibre Intake, which has been prepared, at the request of my predecessor Professor JGAJ Hautvast, by the Health Council's Committee on Dietary Fibre and reviewed by the Standing Committee on Nutrition and the Standing Committee on Medicine. I have today also presented this report to the Minister of Agriculture, Nature and Food Quality. This is the fourth in a series of advisory reports designed to revise the Dutch dietary ref- erence intakes (Nederlandse Voedingsnormen), which were adopted in 1992 by the former Food and Nutrition Council (Voedingsraad). Dietary fibre received very little attention in that report, however. The advisory report Guidelines for a Healthy Diet (Richtlijnen Goede Voeding), which was published by the Food and Nutrition Council in 1986 and is currently being revised, also included a very brief passage about dietary fibre. The attached advisory report is therefore the first thorough evaluation of the physiological effects of dietary fibre to have been undertaken in the Netherlands. The Committee has chosen not to set a dietary reference intake for fibre, but instead to issue a guideline. This decision is motivated by the fact that dietary fibre is the collective term for a group of substances with very wide-ranging physiological effects. -

Dietary Supplementation with Inulin-Propionate Ester Or Inulin
Gut microbiota ORIGINAL ARTICLE Dietary supplementation with inulin-propionate ester Gut: first published as 10.1136/gutjnl-2019-318424 on 10 April 2019. Downloaded from or inulin improves insulin sensitivity in adults with overweight and obesity with distinct effects on the gut microbiota, plasma metabolome and systemic inflammatory responses: a randomised cross- over trial Edward S Chambers, 1 Claire S Byrne,1 Douglas J Morrison,2 Kevin G Murphy,3 Tom Preston,2 Catriona Tedford,4 Isabel Garcia-Perez,5 Sofia Fountana,5 Jose Ivan Serrano-Contreras,5 Elaine Holmes,5 Catherine J Reynolds,6 Jordie F Roberts,6 Rosemary J Boyton,6 Daniel M Altmann,6 Julie A K McDonald, 7 Julian R Marchesi,7,8 Arne N Akbar,9 Natalie E Riddell,10 Gareth A Wallis,11 Gary S Frost1 ► Additional material is ABSTRact published online only. To view Objective To investigate the underlying mechanisms Significance of this study please visit the journal online behind changes in glucose homeostasis with delivery (http:// dx. doi. org/ 10. 1136/ What is already known on this subject? gutjnl- 2019- 318424). of propionate to the human colon by comprehensive and coordinated analysis of gut bacterial composition, ► Short-chain fatty acids (SCFA), derived from For numbered affiliations see fermentation of dietary fibre by the gut end of article. plasma metabolome and immune responses. Design Twelve non-diabetic adults with overweight microbiota, have been shown to improve host insulin sensitivity. Correspondence to and obesity received 20 g/day of inulin-propionate Professor -

Constipation
Constipation Caris Diagnostics Health Improvement Series What is constipation? Constipation means that a person has three bowel movements or fewer in a week. The stool is hard and dry. Sometimes it is painful to pass. You may feel‘draggy’and full. Some people think they should have a bowel movement every day. That is not really true. There is no‘right’number of bowel movements. Each person's body finds its own normal number of bowel movements. It depends on the food you eat, how much you exercise, and other things. At one time or another, almost everyone gets constipated. In most cases, it lasts for a short time and is not serious. When you understand what causes constipation, you can take steps to prevent it. What can I do about constipation? Changing what you 4. Allow yourself enough time to have a bowel movement. eat and drink and how much you exercise will help re- Sometimes we feel so hurried that we don't pay atten- lieve and prevent constipation. Here are some steps you tion to our body's needs. Make sure you don't ignore the can take. urge to have a bowel movement. 1. Eat more fiber. Fiber helps form soft, bulky stool. It 5. Use laxatives only if a doctor says you should. is found in many vegetables, fruits, and grains. Be sure Laxatives are medicines that will make you pass a stool. to add fiber a little at a time, so your body gets used to Most people who are mildly constipated do not need it slowly. -

The Effect of Dietary Fibre on Gut Microbiota, Lipid Profile, And
nutrients Review The Effect of Dietary Fibre on Gut Microbiota, Lipid Profile, and Inflammatory Markers in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomised Controlled Trials Omorogieva Ojo 1,* , Osarhumwese Osaretin Ojo 2, Nazanin Zand 3 and Xiaohua Wang 4 1 School of Health Sciences, University of Greenwich, Avery Hill Campus, Avery Hill Road, London SE9 2UG, UK 2 South London and Maudsley NHS Foundation Trust, University Hospital, Lewisham High Street, London SE13 6LH, UK; [email protected] 3 School of Science, University of Greenwich, Medway Campus, Chatham ME4 4TB, UK; [email protected] 4 The School of Nursing, Soochow University, Suzhou 215006, China; [email protected] * Correspondence: [email protected]; Tel.: +44-20-8331-8626; Fax: +44-20-8331-8060 Abstract: Background: A disequilibrium of the gut microbial community has been closely associated with systemic inflammation and metabolic syndromes including type 2 diabetes. While low fibre and high fat diets may lead to dysbiosis of the gut microbiome as a result of the loss of useful microbes, it has been reported that a high fibre diet may prevent the fermentation of protein and may promote eubiosis of gut microbiota. Aim: This review aims to evaluate the effect of dietary fibre (DF) on gut microbiota, lipid profile, and inflammatory markers in patients with type 2 diabetes. Methods: The Citation: Ojo, O.; Ojo, O.O.; Zand, N.; Wang, X. The Effect of Dietary PRISMA framework was relied on to conduct this systematic review and meta-analysis. Searches were Fibre on Gut Microbiota, Lipid Profile, carried out using electronic databases and reference list of articles. -

Human Ration, As Part of a Dietary Program for Weight Loss
Enes BN, et al., J Food Sci Nutr 2020, 6: 076 DOI: 10.24966/FSN-1076/100076 HSOA Journal of Food Science and Nutrition Research Article an increase in haemoglobin concentration (P=0.0001) and did not Human Ration, as Part of a impair zinc absorption. Weight loss was not different between groups (P=0.924) but waist circumference decreased in HR treatment Dietary Program for Weight Loss, (P<0.01). No differences were observed in bone densitometry, biomarkers or blood pressure. A positive association was observed Improves Iron Status, Dietary for bone mineral density and body mass index (r=0.3956, P=0.0127) and a negative one between erythrocyte zinc and BMI (r=-0.5123; Fibre Intake and Does Not Impair P=0.0005). HR did not potentiate weight loss as part of a dietary energy restriction program, but ameliorated the diet quality and it was Zinc Metabolism and Bone effective in improving iron status, without impairing zinc metabolism. Keywords: Body composition; Bone health; Dietary fibre; Dietary Health in Overweight Women supplements; Mineral status; Whole grains Bárbara Nery Enes1, Natália Elizabeth Galdino Alves2, Neuza Introduction Maria Bronoro Costa3, Rita de Cássia Gonçalves Alfenas2, Sônia Machado Rocha Ribeiro2, Antônio Policarpo Souza Carneiro4 Overweigh has been considered a protective factor against bone and Hércia Stampini Duarte Martino2* loss, osteoporosis and fractures [1]. However, recent publications indicate that this relation is controversial, since the accumulation of 1 Health Center, Nutrition Faculty, Vale do Rio Doce University, Governador fat mass may have a negative on bone health [2]. The subclinical in- Valadares, Minas Gerais, Brazil flammation induced by obesity is followed by significant increases 2Nutrition and Health Department, Federal University of Viçosa, Viçosa, Minas in levels of proinflammatory cytokine and the inflammatory scenario Gerais, Brazil increases bone turnover and reabsorption markers [3]. -
Food and Ibd Condition Your Guide Introduction
CROHN’S & COLITIS UK SUPPORTING YOU TO MANAGE YOUR FOOD AND IBD CONDITION YOUR GUIDE INTRODUCTION ABOUT THIS BOOKLET If you have Ulcerative Colitis (UC) or Crohn’s Disease (the two main forms of Inflammatory Bowel Disease - IBD) you may wonder whether food or diet plays a role in causing your illness or treating your symptoms. This booklet looks at some of the most frequently asked questions about food and IBD, and provides background information on digestion and healthy eating for people with IBD. We hope you will find it helpful. All our publications are research based and produced in consultation with patients, medical advisers and other health or associated professionals. However, they are prepared as general information and are not intended to replace specific advice from your own doctor or any other professional. Crohn’s and Colitis UK does not endorse or recommend any products mentioned. If you would like more information about the sources of evidence on which this booklet is based, or details of any conflicts of interest, or if you have any feedback on our publications, please visit our website. About Crohn’s and Colitis UK We are a national charity established in 1979. Our aim is to improve life for anyone affected by Inflammatory Bowel Diseases. We have over 28,000 members and 50 local groups throughout the UK. Membership costs from £15 per year with concessionary rates for anyone experiencing financial hardship or on a low income. This publication is available free of charge, but we © Crohn’s and Colitis UK would not be able to do this without our supporters 2015 and 2016 and members. -

Therapeutic Enema for Intussusception
Therapeutic Enema for Intussusception Therapeutic enema is used to help identify and diagnose intussusception, a serious disorder in which one part of the intestine slides into another in a telescoping manner and causes inflammation and an obstruction. Intussusception often occurs at the junction of the small and large intestine and most commonly occurs in children three to 24 months of age. A therapeutic enema using air or a contrast material solution may be performed to create pressure within the intestine and "un-telescope" the intussusception while relieving the obstruction. This exam is usually performed on an emergency basis. Tell your doctor about your child's recent illnesses, medical conditions, medications and allergies, especially to barium or iodinated contrast materials. Your child may be asked to wear a gown and remove any objects that might interfere with the x-ray images. An ultrasound may be performed to help confirm the diagnosis. What is a Therapeutic Enema for Intussusception? What is intussusception? Intussusception is a serious disorder in which one part of the intestine slides into another part of the intestine, similar to a collapsing telescope. The intestine becomes inflamed and swollen and can cause an obstruction or blockage. Symptoms can include severe abdominal pain, fever, vomiting or abnormal stools. Intussusception may occur anywhere along the gastrointestinal tract; however, it often occurs at the junction of the small and large intestine. The condition most commonly occurs in children three months to 24 months of age. Intussusception is a medical/surgical emergency. If your child has some or all of the symptoms of intussusception, you should call your physician or an emergency medical professional immediately. -

Gastrointestinal Intraluminal Ph in Normal Subjects and Those with Colorectal Adenoma Or Carcinoma
Gut, 1990,31, 1355-1357 1355 Gastrointestinal intraluminal pH in normal subjects Gut: first published as 10.1136/gut.31.12.1355 on 1 December 1990. Downloaded from and those with colorectal adenoma or carcinoma G Pye, D F Evans, S Ledingham, J D Hardcastle Abstract colorectal cancer but only with total non-starch Recent evidence suggests that the production polysaccharide. 14 of colorectal carcinogens is facilitated when In a comprehensive review of recent hypo- the pH of the colonic contents is alkaline. It theses for the origin of colorectal cancer,'5 Bruce follows that the colonic intraluminal pH of was unable to support enthusiastically the patients with colorectal neoplasms should be evidence in favour ofa bacterial origin of colonic higher than in normal subjects. Gastro- carcinogens but did find evidence to support the intestinal pH has been measured in 30 patients role ofdietary fats and fibre as well as faecal pH. with colorectal cancer and 37 patients with benign colorectal adenomas (using a pH sensi- tive radiotelemetry capsule). These values SUBJECTS AND METHODS have been compared with those recorded in 66 A total of 133 pH studies were successfully normal subjects. No differences in gastro- performed. Sixty six normal volunteers com- intestinal pH were found and the results did pleted the study (47 men, median age 26 years, not support the hypothesis that colonic pH range 21-82 years). None of the volunteers had plays a role in the aetiology of colorectal any history ofcolorectal disease. neoplasia. Thirty seven patients with benign adenoma- tous polyps underwent pH studies (24 men, median age 66 years, range 49-80 years). -
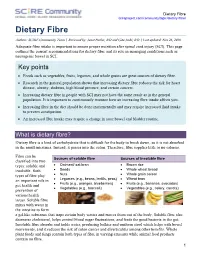
Dietary Fibre Scireproject.Com/Community/Topic/Dietary-Fibre
Dietary Fibre scireproject.com/community/topic/dietary-fibre/ Dietary Fibre Authors: SCIRE Community Team | Reviewed by: Janet Parker, RD and Gita Joshi, RD | Last updated: Nov 26, 2019 Adequate fibre intake is important to ensure proper nutrition after spinal cord injury (SCI). This page outlines the current recommendations for dietary fibre and its role in managing conditions such as neurogenic bowel in SCI. Key points • Foods such as vegetables, fruits, legumes, and whole grains are great sources of dietary fibre. • Research in the general population shows that increasing dietary fibre reduces the risk for heart disease, obesity, diabetes, high blood pressure, and certain cancers. • Increasing dietary fibre in people with SCI may not have the same result as in the general population. It is important to continuously monitor how an increasing fibre intake affects you. • Increasing fibre in the diet should be done incrementally and may require increased fluid intake to prevent constipation. • An increased fibre intake may require a change in your bowel and bladder routine. What is dietary fibre? Dietary fibre is a kind of carbohydrate that is difficult for the body to break down, so it is not absorbed in the small intestines. Instead, it passes into the colon. Therefore, fibre supplies little to no calories. Fibre can be Sources of soluble fibre Sources of insoluble fibre classified into two types: soluble and • Oatmeal/ oat bran • Brown rice insoluble. Both • Seeds • Whole wheat bread types of fibre play • Nuts • Whole grain cereal an important role in • Legumes (e.g., beans, lentils, peas) • Wheat bran • Fruits (e.g., oranges, blueberries) • Fruits (e.g., bananas, avocados) gut health and • Vegetables (e.g., broccoli) • Vegetables (e.g., celery, carrots) prevention of various health issues. -

Management of Gastrointestinal Disorders in Rett Syndrome
Management of gastrointestinal disorders in Rett syndrome Jenny Downs & Helen Leonard Telethon Kids Institute, Perth, Western Australia What is meant by gastrointestinal disorders? The three most common gastro-intestinal problems affecting girls and women with Rett syndrome are: constipation, Gastro-Oesophageal Reflux Disease or Gastro-Esophageal Reflux Disease (GORD/GERD or reflux) and abdominal bloating. Constipation occurs where stools are dry, hard and difficult to pass. Constipation can cause considerable discomfort and pain. Reflux occurs when the muscle at the lower end of the oesophagus does not close properly after food has passed through to the stomach. As a result, stomach contents can pass back up the oesophagus which can be painful, and in extreme cases, damage to the oesophagus lining. Acid may also flow back into the oesophagus when the stomach doesn’t empty properly. This is known as delayed gastric emptying. Abdominal bloating describes the swelling of the abdomen, accompanied by feelings of tightness, fullness, discomfort and pain. Why do gastrointestinal disorders occur in Rett syndrome? As the digestive system operates alongside other systems in the body (the nervous, circulatory, muscular -skeletal, respiratory and endocrine systems), disruptions to any of these systems can affect the healthy operation of the digestive system. • Reduced intestinal motility, physical activity and some side effects from various medications may cause individuals with Rett syndrome to suffer constipation. • Reflux is likely to occur in individuals with restricted mobility and/or scoliosis. • The tendency to hyperventilate, breath hold and swallow air can cause abdominal bloating. Pain, anxiety and excitement may exacerbate these issues and increase discomfort. -

When to Seek Medical Attention
When To Seek Medical Attention The Signs & Symptoms of Crohn’s Disease There is no doubt that inflammatory bowel disease (IBD) is a serious medical condition. During flare-ups and when the disease is active, symptoms can be troublesome, distressing, and downright embarrassing. Most people with IBD will need to take medications on an ongoing basis, even during periods of remission, to keep the inflammation in check and prevent flare-ups. There might be times where you will need to be in hospital—for example, if you become severely dehydrated or develop a complication. At some point you might also have to face the prospect of surgery, either to treat the disease itself or for complications associated with your condition. But the good news is that IBD is manageable: it will not necessarily take over your entire life, and the life expectancy of those with the disease is normal. With the current range of treatment options available, most people are able to lead full and productive lives, complete with family, career, leisure activities, and travel. However it is important to be aware of any change that may indicate a flare-up, a worsening of the condition, or that a new problem has developed so that prompt action can be taken. Typical signs & symptoms include: • frequent, watery diarrhoea • sense of urgency to have a bowel movement • crampy abdominal pain • a feeling of ‘blockage’ • fever during active stages of disease • rectal bleeding (if the colon is involved) • loss of appetite • tiredness and fatigue • weight loss. The signs and symptoms of Crohn’s disease can vary considerably among those who have the condition, depending on the location and severity of the inflammation within the GI tract.