Capsule 2018 April
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Specialty Hospital in Alwarpet, Chennai, Kauvery Hospital Marks Its Presence in This Bustling Capital of Tamil Nadu That Is Home to 4.5 Million People
The New Age Family Hospital With a gleaming new 200 bed multi- specialty hospital in Alwarpet, Chennai, Kauvery hospital marks its presence in this bustling capital of Tamil Nadu that is home to 4.5 million people. In keeping with Kauvery's high standards, our hospital in Chennai boasts world- class facilities, top-of-the-line infrastructure, the best doctors in Chennai and highly trained medical staff who cater to all your needs with a smile. Kauvery Hospital, Chennai is an imposing building spanning seven floors located right in the middle of the city just adjacent to Alwarpet Flyover. We're very easy to reach from all major locations in Chennai. Our team of experienced doctors, specialists and medical staff are highly capable of dealing with every kind of medical situation, emergency and healthcare requirement. Our staffs are well trained to manage a wide range of complex medical and surgical issues. Our expertise in medical care is complemented by our modern state-of-the-art intensive care units. We are also proud to have one of the best critical care teams in India with 24x7 access to specialists and all related support services. Our Vision Statement To establish ourselves as the new age family hospital group, with a strong culture of personalized patient care, and a reputation of having established centers of excellence across all medical specialties and allied health services and be regarded as the most valued service provider in the region with national acclaim. Our Mission Statement To dedicate ourselves to unleash our fullest potential towards providing exemplary healthcare services, education & development and make a qualitative difference in people's lives by enriching their quality of life. -

RANKING SURVEY 2021 Against This Back Drop, Many Options Have Come up for Patients
*BTB140414/ /06/K/1*/06/Y/1*/06/M/1*/06/C/1* SURVEY An Optimal Media Solutions Initiative, A division of Times Internet Limited, circulated with The Times of India, Chennai Friday, 5 March, 2021 An Advertorial, Health Promotional Feature ALL INDIA CRITICAL CARE HOSPITAL Indian healthcare industry has witnessed tremendous growth in the last decade or so. find it difficult to decide which hospital to choose for which ailment. It is in this Indian doctors have always been valued. However in the recent past, many world class context, OMS, a division of Times Group, took the initiative to start a system of hospitals were set up by many top corporates with best infrastructure to offer world ranking top hospitals in India in various specialities and thereby help people class medical care in India. This has given major boost to medical tourism as many make informed choices. The rankings also serve as great motivation for various people from other countries found that they could get top class health care in India. brands to further enhance their facilities and care, which leads to even better RANKING SURVEY 2021 Against this back drop, many options have come up for patients. However, they healthcare services in India. ONCOLOGY NATIONAL MULTI SPECIALITY RANKING CARDIO SCIENCES NATIONAL MULTI SPECIALITY RANKING OBGYN NATIONAL MULTI SPECIALITY RANKING PAEDIATRICS NATIONAL MULTI SPECIALITY RANKING Rank Name Rank Name Rank Name Rank Name 1 Apollo Hospitals, Greams Lane, Chennai 1 Medanta the Medicity, Sector 38, Gurugram 1 Apollo Hospitals, Greams -

CHENNAI PPN LIST of HOSPITALS PIN S No HOSPITAL NAME Address CITY STATE CODE 1 Abhijay Hospital (P) Ltd
CHENNAI PPN LIST OF HOSPITALS PIN S No HOSPITAL NAME Address CITY STATE CODE 1 Abhijay Hospital (P) Ltd. NO.22/2,E.S.I HOSPITAL ROAD,PERAVALLUR Chennai Tamilnadu 600011 2 Aditya Hospital NO.7,BARNBAY ROAD,KILPAUK Chennai Tamilnadu 600010 3 Amma Hospital # 1,SOWRASTRA NAGAR7TH STREET Chennai Tamilnadu 600094 4 Ammayi Eye Hospital NEW # 80 7TH AVENUE, ASHOK NAGAR Chennai Tamilnadu 600083 5 Anand Hospital #201, KAMARAJ SALAI,,MANALI MANALI Chennai Tamilnadu 600068 6 Apollo Hospital ( T.H.Road-Chennai) #645,T.H.ROAD,TONDIARPET Chennai Tamilnadu 600081 7 Appasamy Medicare Centre Pvt Ltd 23-25 FRIENDS AVENUE ARUMBAKKAM,ARUMBAKKAM Chennai Tamilnadu 600106 8 Athipathi Hospital And Research Center PLOT NO 1 100 FT RD TANNI NAGAR,VELACHARY Chennai Tamilnadu 600042 9 B M Hospitals 36 5TH MAIN ROAD THILLAI GANGA,NAGARCHEENAI Chennai Tamilnadu 600061 10 Billroth Hospital Limited #43, LAKSHMI TAKIS ROAD, SHENOY NAGAR Chennai Tamilnadu 600030 NO.28. CATHEDRAL GARDEN 11 Brs Hospital Pvt.Ltd Chennai Tamilnadu 600034 ROADCATHEDRAL,GARDENSROAD 12 Billroth Hospitals - Ra Puram #52, 2ND MAIN ROAD, RAJA ANNAMALAI PURAM Chennai Tamilnadu 600028 15 DR RADHAKRISHNAN SALAI MYLAPORE NEXT,TO CITY 13 C.S.I. Kalyani General Hospital Chennai Tamilnadu 600004 CENTRE 14 Christudas Orthopaedic Speciality Hospital #9.DURAISWAMY NGR. I.A.F. ROAD Chennai Tamilnadu 600059 #327MUTHURANGAM 15 Deepam Hospital ROADTAMBARAM(WEST),KANCHIPURAM WEST Chennai Tamilnadu 600045 TAMBARAM 16 Chennai Meenakshi Multispeciality Hospital Ltd. # 148,LUZ CHURCH ROAD,MALAPORE Chennai Tamilnadu 600004 Hariharan Diabetes And Heartcare Hospitals Pvt 17 24826 29TH STREET NANGANALLUR,NANGANALLUR Chennai Tamilnadu 600061 Ltd 18 Dr Agarwal'S Eye Hospital Ltd No.222,TTK Road, Alwarpet Chennai Tamilnadu 600086 19 Dr.Rabindrans Healthcare Centre (P)Ltd. -

Chennai PPN Network Hospital List Sr
Chennai PPN Network Hospital List Sr. Tel_are Hospital Name Location Address Pin_No Tel_No MobileNo City State E_Mail PPN City No. a_code 81-86 Annai Valasaravakk Tamil [email protected] 1 A N N Hospital Therasa Street 600087 044 24869300 9442360800 Chennai Chennai am Nadu om Indira Nagar # 172, SOLAIAPPAN STREET, NEAR drselvaraj@avhospital Tamil 2 A V Hospitals Parrys MAHARANI 600021 044 25955859 9444013879 Chennai s.com;kalaivani.vetrise Chennai Nadu THEATRE, [email protected] MANNADY [email protected] No. 395, T H Road, Tamil m;aakashsrk_dr@yah 3 Aakash Hospital Thiruvotriyur Near Thiruvottriyur 600019 044 25730099 9444382293 Chennai Chennai Nadu oo.co.in;aakashsrkdr Bus Terminus @gmail.com abhijay.claims@gmail. 22/2, E.S.I Hospital Abhijay Hospital (p) Tamil com; 4 Perambur Road, Perambur, 600011 044 49015050 9884368589 Chennai Chennai Ltd Nadu cashless@abhijayhosp Peravallur itals.com adityahospital@gmail. 7, Barnaby Road, Tamil com; 5 Aditya Hospital Kilpauk 600010 044 26411447 9840727909 Chennai Chennai Kilpauk, Chennai Nadu insurance@adityahos pital.co.in insurance@agadaheal thcare.net;karthikaran No 8, Dr Nair Road, i.p@agadahealthcare. Agada Healt Care Tamil 6 T Nagar Behind Vani Mahal, 600017 044 28152604 9087718512 Chennai net;prabhub@agadah Chennai Pvt Ltd Nadu T Nagar ealthcare.net; operations@agadahea lthcare.net 1,Sowrastra Nungambakk Tamil sureshdrsuresh@yaho 7 Amma Hospital Nagar,7th 600094 044 24840441 9840048896 Chennai Chennai am Nadu o.co.in; Street,Choolaimedu new no 80 ,7 th ammayieyehospital@y Ammayi Eye Tamil -
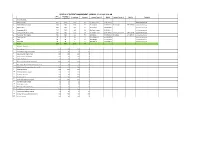
Status of Patient Management Chennai
STATUS OF PATIENT MANAGEMENT CHENNAI - 13.05.2021 8.00 AM Bed Covid bed Occupancy Vacancy Contact Person 1 Mobile Contact Person 2 Mobile Remarks Capacity availability I Covid Hospitals 1 MMC RGGGH 1618 1618 1527 91 Dr.Sudharshini 9791736334 O2 bed vacancy -0 2 Stanley Medical College 1400 1400 1348 52 Dr. Aravind 9840242328 Dr.Ramesh 9841736989 O2 bed vacancy -4 3 Kilpauk MCH 550 550 536 14 Dr. Geetha 9940087404 O2 bed vacancy -0 4 Omandurar MCH 727 727 695 32 Dr Pravin Kumar 8903306131 O2 bed vacancy -0 5 Govt Covid Hospital, Guindy 550 550 536 14 Dr. Mohankumar 9841744766 Dr Narayanaswami 9841170145 O2 bed vacancy -0 6 Tambaram TB Hospital 500 500 422 78 Dr Rathika 8939729493 Dr Sridhar 9444007311 O2 bed vacancy -0 7 Tambaram GH 45 45 42 3 Dr.C.Palanivel, 9444135154 O2 bed vacancy -3 8 KGH 50 50 36 14 Dr Karthiga 9444366296 O2 bed vacancy -4 9 KGH OMC 50 50 44 6 Dr.Kalpana 9345102848 O2 bed vacancy -0 Total 5490 5490 5186 304 B.Private Hospitals 1 Aakash Hospital 120 120 120 0 2 ACS Medical College And Hospital 100 100 63 37 3 Apollo Hospital, Greams Road 205 205 205 0 4 Apollo Hospitals, Vanagaram 123 123 123 0 5 Appasamy Hospital 87 87 87 0 6 Bhaarath medical college and hospital 160 160 160 0 7 Bharathiraja Hospital & Research Centre Pvt Ltd 93 93 93 0 8 Billroth Hospitals Shenoy Nagar, Chennai TN. 185 185 185 0 9 Chettinad Hospital 525 525 525 0 10 CSI Kalyani General Hospital 110 110 110 0 11 Dr. -
![Dr. Suresh Mickymaray, M.Sc., Ph.D., [Microbiology] and Diploma in Medical Laboratory Technology (DMLT)](https://docslib.b-cdn.net/cover/1119/dr-suresh-mickymaray-m-sc-ph-d-microbiology-and-diploma-in-medical-laboratory-technology-dmlt-1051119.webp)
Dr. Suresh Mickymaray, M.Sc., Ph.D., [Microbiology] and Diploma in Medical Laboratory Technology (DMLT)
CV Dr. Suresh Mickymaray, M.Sc., Ph.D., [Microbiology] and Diploma in Medical Laboratory Technology (DMLT) Assistant Professor Department of Biology College of Science –Zulfi Kingdom of Saudi Arabia HP: 0595592263 Email: [email protected] Residence address in India No: 11, 1st Street, Sri Rajaganapathy Nagar, JK Nagar, Khajamalai Post, Trichy: 620023 Dr. Suresh Mickymaray - CV 16.11.2016 Dr. Suresh Mickymaray Assistant Professor Department of Biology Central Bioscience Research Laboratories College of Science Majmaah University- Zulfi Kingdom of Saudi Arabia CURRICULUM ABSTRACT: OVER 22 years of active involvement in Diagnostic Microbiology fields inclusive of Research, Teaching, Clinical Diagnostic Microbiology, Molecular biology, Project guidance’s for Masters, M.Phil., and Ph.D’s. Day to-day Lab management and administration, Hospital infection control, CME organization and External quality control programs etc. CARRIER POSITIONS : AUGUST 2014 TO ASSISTANT PROFESSOR DEPARTMENT OF BIOLOGY FORMERLY IN MEDICAL LABORATORIES PRESENT MEMBER-RESEARCH: CENTRAL BIOSCIENCE RESEARCH LABORATORIES (CBRL) COLLEGE OF SCIENCE MAJMAAH UNIVERSITY AL-ZULFI – KINGDOM OF SAUDI ARABIA DEPT. OF MICROBIOLOGY & MOLECULAR BIOLOGY HEAD- MICROBIOLOGY & DOCTORS’DIAGNOSTIC CENTER -TRICHY (A UNIT OF MOLECULAR BIOLOGY MULTISPECIALITY LAB SERVICES) (STATE GOVT 2012 TO AUGUST APPROVED CENTRE FOR H1N1 TESTS ) 2014 ASSISTANT PROFESSOR DOCTORS’ INSTITUTE OF LABORATORY SCIENCE (Affiliated to Tamilnadu Dr. MGR Medical University – Chennai) OCTOBER,2010 ASSISTANT -

List of Tie-Up Hospitals for Super Specialty Treatment
LIST OF TIE-UP HOSPITALS FOR SUPER SPECIALTY TREATMENT 05.11.2020 S.No Name of the Address District Numbe Departments Period of MOA Contact email ID Hospital/Investigation centre r of Number 1 Kauvery Hospital 9/50, Trichy Main Salem 100Beds Cardiology, Cardiothoracic 04.03.2020 03.03.2021 0427- corporatebilling.salem@kauver Road, Surgery, Nephrology, Urology, 2677777,9344 yhospital.com Seelanaickenpatty, Dialysis, Medical 503284,98408 Salem - 636 201 Gastroenterology, Surgical 17716 Gastroenterology, Medical Oncology, Surgical Oncology, Plastic Surgery, Neurology and Nuerosurgery 2 Universal Cancer hospital limited 370, Nadu Street, Jari Salem 55 Medical Oncology, Surgical 10.01.2020 09.01.2021 0472- universalcancerhospital@gmail Kondalampatty, Oncology, Radiotheraphy, 2273477,2273 .com Kondalampatty Gastroenterology, Gastro 577, Roundtana, Salem - Intentinal Surgery, Neurology, 8608044773,9 636 010 Neuro surgery, Burns and 842188083 Plastic Surgery, Reconstructive Surgery, Imaging and Diagnostic facilities (SST only) 3 Vinayaka Mission Super NH-47, Sankari Main Salem 120 Urology, Neurosurgery, 28.02.2020 27.02.2021 0427-2200110, [email protected] Speciality Hospitals P Ltd Road, Veerapandi (PO) Neurology, Cardiology, 9362128563, Salem 636 308 Interventional Cardiology, 9500182225 Cardio Thoracic Surgery, Nephrology, Paediatrics Surgery, Surgical Gastroenterology, Interventional Radiology, Medical Oncology, Surgical Oncology, Vascular Surgery, Plastic/reconstructive Surgery, 4 Manipal Hospital Dalmia Board, Salem- Salem 140 CardiothoracicRenal -
Notice-And-Route-Map.Pdf
Annual Report 2015 - 2016 INDEX Page No. Notice to the Shareholders 001 Directors' Report 021 Independent Auditors' Report 039 Balance Sheet 047 Statement of Profit and Loss 048 Cash Flow Statement 049 Notes forming part of Financial Statements 051 Independent Auditors' Report on Consolidated Financial Statements 076 Balance Sheet 083 Statement of Profit and Loss 084 Cash Flow Statement 085 Notes forming part of Consolidated Financial Statements 087 Proxy Form 113 Attendance Slip 115 Annual Report 2015 - 2016 SRI KAVERY MEDICAL CARE (TRICHY) LIMITED Registered Office : No.1, K.C. Road Tennur, Trichy - 620 017 FROM MD ’S DESK Dear Share Owners It has been quite a while since I have connected with you all. In these few years, Kauvery has witnessed a qualitative & quantitative change for the better. We have evolved and fortified our base. We have consolidated our processes. We have made headway in our qualitative journey. With focused branding, we have indeed worked our way towards building the brand of Kauvery. Overall, it has been an optimistic and encouraging scenario. Centers of Excellence As part of our strategic planning process, we have created centers of excellence in core specialties across our units. The exclusive kidney care center at our parent unit at Tennur has evolved as a center of excellence in Urology & Nephrology. From dialysis to transplants it has emerged as one of the sought after treatment center for all kinds of kidney related disease The Brain & Spine center with an exclusive Neuro ICU, is a comprehensive center of excellence for all neurological disorders. The center is a pioneer in Trichy for GPS guided surgery, mechanical thrombectomy and interventional stroke management. -

Capsule Magazine July 2017
Medi Magazine kauvery A quarterly magazine from VOLUME - 21 | ISSUE - 03 | JULY 2017 - 21 | ISSUE 03 JULY VOLUME Anesthesia and A Rare Organism Challenges Causing Septic Arthritis of Hip Joint Awareness on Vocal Hygiene Diabetic Retinopathy -An Overview Stricture Urethra Inauguration of Chennai, Anna Nagar Branch Acute Myocardial Infarction in Infancy and Renal Update Childhood - A reality 2017 - CME Annual Day 2017 Papillary Carcinoma of Thyroid Pattimandram To download this magazine This magazine is free circulation for hospitals and doctors only, Not for sale. Design and logo of kauvery hospital are property of scan this QR Code Kauvery Hospital, To get this magazine copy mail us at: [email protected] with QR scanner APP If you want to know any other details contact us on Editorial Address in your smartphone KAUVERY CAPSULE | JANUARY 2017 CAPSULE MAGAZINE Capsule Magazine is published by Kauvery Hospital Copyright 2016 © Kauvery Hospital PATRONS Dr. S. Chandrakumar Dr. S. Manivannan ADVISORY BOARD Dr. D. Senguttuvan 00 Acute Myocardial Dr. Aravindan Selvaraj Dr. T. Senthil Kumar Infarction in Infancy & Childhood - A reality EDITOR Dr. S. Senthil Kumar Dr. Prashanth Sha, MBBS., MS., DNB., Consultant Cardiologist EDITORIAL TEAM Dr. Lakshmi Prashant, MBBS., MD(AIIMS)., Dr. S. Velmurugan Consultant Paediatrician Dr. S. Aravinda Kumar 01 Kauvery Hospital, Chennai From Dr. Iyyappan Ponnuswamy 00 the Editor’s Desk Acute Myocardial Infarction in Infancy & TECHNICAL TEAM Dr. S. Senthil Kumar, Ms., DNB., (Uro) Childhood - A reality Dr. Ve. Senthil Vel Murugan HOD & Senior consultant Urologist & Dr. A. Subramanian Andrologist Dr. Prashanth Sha, MBBS., MS., DNB., Transplant Surgeon Consultant Cardiologist Laparoscopic surgeon Dr. -

S.No. Name of Ethics Committee RC No
S.No. Name of Ethics Committee RC No. Address State All India Institute of Medical Sciences, Room No.102, 1st floor, OT Block, 1 Ethics Committee ECR/538/Inst/DL/2014/RR-17 Delhi Ansari Nagar, New Delhi-110029 Aster Aadhar Hospital, R.S. NO. 628, 'B' Ward, Near Shastri Nagar, KMT 2 Aster Aadhar Ethics Committee ECR/470/Inst/MH/2013/RR-16 Maharashtra Workshop, Kohlapur-416012 3 Visakha Institutional Review Board ECR/4/Indt/AP/2013/RR-16 A-11, Prince Villae Royal Appartment, Siripuram, Visakhapatnam- 530003 Andhra Pradesh SAUMYAA, C-321, Behind Ganesh Temple N-1, CIDCO, Aurangabad- 4 Aurangabad Ethics Committee ECR/122/Indt/MH/2013/RR-16 Maharashtra 431003 Ethics Committee of Diabetes Thyroid BCM Health Island, PU4, Scheme 54, Behind Prestige Management 5 ECR/409/Inst/MP/2013/RR-16 Madhya Pradesh Hormone Research Institute Institute, Near Bombay Hospital, Indore- 452010 Jehangir Clinical Development Centre Pvt. Ltd., Jehangir Hospital 6 Ethics Committee ECR/352/Inst/MH/2013/RR-19 Maharashtra Premises, 32 Sassoon Road, Pune- 411001 89, 3rd Cross, S V K Layout, Basaveshwar Nagar, Banagalore, Urban- 7 Lifeline Ethics Committee ECR/76/Indt/KA/2013/RR-16 Karnataka 560079 Instutional Ethics Committee-Clinical Indraprastha Apollo Hospitals, Sarita Vihar, Delhi- Mathura road, New 8 ECR/5/Inst/DL/2013/RR-16 Delhi Studies Delhi- 110076 H.No.- D/129, St. No.-13 Opp-Durga Mandir, Ashok Nagar, Shahdara- 9 Good Society for Ethical Research ECR/69/Indt/DL/2013/RR-19 Delhi 110093 Ethics Committee, S.P. Medical College & S.P Medical College & A.G Hospitals, HRMC Cardiovascular Sciences & 10 ECR/27/SP/Inst/RJ/2013/RR-16 Rajasthan A.G. -

Capsule Magazine Aprl 2017
Medi Magazine kauvery A quarterly magazine from VOLUME - 20 | ISSUE 02 APRIL 2017 VOLUME Anesthesia and A Rare Organism Challenges Causing Septic Arthritis of Hip Joint Awareness on Vocal Hygiene Diabetic Retinopathy -An Overview Stricture Urethra Inauguration of Chennai, Anna Nagar Branch Acute Myocardial Infarction in Infancy and Renal Update Childhood - A reality 2017 - CME Annual Day Papillary Carcinoma 2017 of Thyroid Pattimandram To download this magazine This magazine is free circulation for hospitals and doctors only, Not for sale. Design and logo of kauvery hospital are property of scan this QR Code Kauvery Hospital, To get this magazine copy mail us at: [email protected] with QR scanner APP If you want to know any other details contact us on Editorial Address in your smartphone KAUVERY CAPSULE | JANUARY 2017 CAPSULE MAGAZINE Capsule Magazine is published by Kauvery Hospital Copyright 2016 © Kauvery Hospital 01 From the Editor’s Desk PATRONS Dr. S. Chandrakumar Dr. S. Manivannan 02 Acute Myocardial ADVISORY BOARD Dr. D. Senguttuvan Infarction in Infancy & Dr. Aravindan Selvaraj Dr. S. Senthil Kumar, Ms., DNB., (Uro) Childhood - A reality Dr. T. Senthil Kumar HOD & Senior consultant Urologist & Andrologist Dr. Prashanth Sha, MBBS., MS., DNB., EDITOR Transplant Surgeon Consultant Cardiologist Dr. Lakshmi Prashant, MBBS., MD(AIIMS)., Dr. S. Senthil Kumar Laparoscopic surgeon Kauvery Kidney Centre, Tennur, Trichy Consultant Paediatrician Kauvery Hospital, Chennai EDITORIAL TEAM Dr. S. Velmurugan Dr. S. Aravinda Kumar Dr. Iyyappan Ponnuswamy TECHNICAL TEAM Dr. Ve. Senthil Vel Murugan Dr. A. Subramanian ADMIN TEAM Mr. S. Sathishkumar Mrs. JPJ. Bindhu CO-ORDINATORS 04 Mrs. G. Percy Anesthesia and Dr. -

Looking at Life Beyond Work Dream Bigger and Achieve Bigger
Looking At Life Beyond Work Dream Bigger And Achieve Bigger Dr.G.Balamurali MBBS, MRCS (Ed), MD (UK),FRCS (Surgical Neurology), Consultant Spine and Neurosurgeon, Chennai. A Neurosurgeon- A Dream And A Passion For A Lifetime Born to teachers, Dr.Balamurali was a highly motivated kid right from childhood days. He always aimed to become a doctor and strived for it. Being an all-rounder at Montfort School, Yercaud he studied hard and completed medicine with distinction. Later, two months after completing his internship from Kilpauk Medical College, on a cold winter night he landed in London with eyes full of dreams and hopes! He always carried a positive attitude and looked forward to a bright future. He didn’t think much about how, when and where he would achieve it. With high hopes, aspirations and dreams to be a surgeon, he worked hard, pushed himself out of his comfort zones and completed his training as a general surgeon from the Royal College of Surgeons Edinburgh. Soon, he completed his MRCS and began walking closer and closer towards his dreams. From Frustrations To Achievements To become a Neurosurgeon in the 90s was next to impossible for the minority race! But, that didn’t stop him from dreaming and working hard towards his goal. Still, the path ahead was not as smooth as he had expected. Having failed 8 interviews with a decent CV and many publications to his credit, he started getting frustrated that he was unable to achieve his dream- to be a Neurosurgeon! But that didn’t deter him.