Zellweger Syndrome: an Older Child with Progressive Foot Deformity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
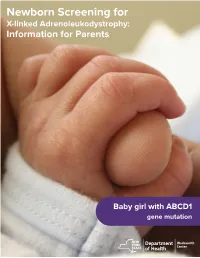
Newborn Screening for X-Linked Adrenoleukodystrophy: Information for Parents
Newborn Screening for X-linked Adrenoleukodystrophy: Information for Parents Baby girl with ABCD1 gene mutation What is newborn screening? the symptoms of ALD during childhood. Rarely, some women who are carriers of ALD develop mild symptoms as adults. It Newborn screening involves laboratory testing on a small is important for your family to meet with a genetic counselor sample of blood collected from newborns’ heels. Every state to talk about the genetics of ALD and implications for other has a newborn screening program to identify infants with rare family members. disorders, which would not usually be detected at birth. Early diagnosis and treatment of these disorders often prevents Why do only boys have ALD? serious complications. Only boys have ALD because it is caused by a mutation in What is adrenoleukodystrophy (ALD)? a gene (ABCD1) on the X chromosome, called “X-linked inheritance.” Males only have one X chromosome so they have ALD is one of over 40 disorders included in newborn screening one ABCD1 gene. Males with a nonfunctioning ABCD1 gene in New York State. It is a rare genetic disorder. People with have ALD. Females have 2 X chromosomes, so they have two ALD are unable to breakdown a component of food called ABCD1 genes. Females with one ABCD1 gene mutation will very long chain fatty acids (VLCFA). If VLCFA are not broken be carriers. When a mother is a carrier of ALD, each son has a down, they build up in the body and cause symptoms. 50% chance of inheriting the disorder and each daughter has a 50% chance of being a carrier. -

Peroxisome Biogenesis Disorders ⁎ Steven J
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1763 (2006) 1733–1748 www.elsevier.com/locate/bbamcr Review Peroxisome biogenesis disorders ⁎ Steven J. Steinberg a,b, , Gabriele Dodt c, Gerald V. Raymond a,b, Nancy E. Braverman d, Ann B. Moser a,b, Hugo W. Moser a,b a Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, MD, USA b Kennedy Krieger Institute, Baltimore, MD, USA c Interfakultäres Institut für Biochemie, Eberhard Karls Universität, Tübingen, Germany d Department of Pediatrics and Institute of Genetic Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, USA Received 25 May 2006; received in revised form 5 September 2006; accepted 6 September 2006 Available online 14 September 2006 Abstract Defects in PEX genes impair peroxisome assembly and multiple metabolic pathways confined to this organelle, thus providing the biochemical and molecular bases of the peroxisome biogenesis disorders (PBD). PBD are divided into two types—Zellweger syndrome spectrum (ZSS) and rhizomelic chondrodysplasia punctata (RCDP). Biochemical studies performed in blood and urine are used to screen for the PBD. DNA testing is possible for all of the disorders, but is more challenging for the ZSS since 12 PEX genes are known to be associated with this spectrum of PBD. In contrast, PBD-RCDP is associated with defects in the PEX7 gene alone. Studies of the cellular and molecular defects in PBD patients have contributed significantly to our understanding of the role of each PEX gene in peroxisome assembly. © 2006 Elsevier B.V. -
Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity
International Journal of Molecular Sciences Review Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity Yannick Das, Daniëlle Swinkels and Myriam Baes * Lab of Cell Metabolism, Department of Pharmaceutical and Pharmacological Sciences, KU Leuven, 3000 Leuven, Belgium; [email protected] (Y.D.); [email protected] (D.S.) * Correspondence: [email protected] Abstract: Peroxisomes are multifunctional organelles, well known for their role in cellular lipid homeostasis. Their importance is highlighted by the life-threatening diseases caused by peroxisomal dysfunction. Importantly, most patients suffering from peroxisomal biogenesis disorders, even those with a milder disease course, present with a number of ocular symptoms, including retinopathy. Patients with a selective defect in either peroxisomal α- or β-oxidation or ether lipid synthesis also suffer from vision problems. In this review, we thoroughly discuss the ophthalmological pathology in peroxisomal disorder patients and, where possible, the corresponding animal models, with a special emphasis on the retina. In addition, we attempt to link the observed retinal phenotype to the underlying biochemical alterations. It appears that the retinal pathology is highly variable and the lack of histopathological descriptions in patients hampers the translation of the findings in the mouse models. Furthermore, it becomes clear that there are still large gaps in the current knowledge on the contribution of the different metabolic disturbances to the retinopathy, but branched chain fatty acid accumulation and impaired retinal PUFA homeostasis are likely important factors. Citation: Das, Y.; Swinkels, D.; Baes, Keywords: peroxisome; Zellweger; metabolism; fatty acid; retina M. Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity. -

Functional Characterization of Novel Mutations in GNPAT and AGPS, Causing Rhizomelic Chondrodysplasia Punctata (RCDP) Types 2 and 3
RESEARCH ARTICLE OFFICIAL JOURNAL Functional Characterization of Novel Mutations in GNPAT and AGPS, Causing Rhizomelic Chondrodysplasia Punctata www.hgvs.org (RCDP) Types 2 and 3 Brandon Itzkovitz,1† Sarn Jiralerspong,1† Graeme Nimmo,1 Melissa Loscalzo,2 Dafne D. G. Horovitz,3 Ann Snowden,4 Ann Moser,4 Steve Steinberg,4,5 and Nancy Braverman1,6∗ 1Montreal Children’s Hospital Research Institute, Montreal, Quebec, Canada; 2Division of Genetics, Department of Pediatrics, University of South Florida, Tampa, Florida; 3Centro de Genetica Medica, Instituto Fernandes Figueira—FIOCRUZ, Rio de Janeiro, Brazil; 4Department of Neurogenetics, Kennedy Krieger Institute, Baltimore, Maryland; 5Department of Neurology, Johns Hopkins University, Baltimore, Maryland; 6Department of Human Genetics and Pediatrics, McGill University, Montreal, Quebec, Canada Communicated by Iain McIntosh Received 12 May 2011; accepted revised manuscript 13 September 2011. Published online 3 October 2011 in Wiley Online Library (www.wiley.com/humanmutation).DOI: 10.1002/humu.21623 Introduction ABSTRACT: Rhizomelic chondrodysplasia punctata Rhizomelic chondrodysplasia punctata (RCDP) is a rare disorder (RCDP) is a disorder of peroxisome metabolism result- of ether phospholipid, or plasmalogen, biosynthesis. Patients are ing from a deficiency of plasmalogens, a specialized class suspected clinically by proximal shortening of long bones or rhi- of membrane phospholipids. Classically, patients have a zomelia, bilateral congenital cataracts, dysmorphic facial features, skeletal dysplasia and profound mental retardation, al- and severe growth and developmental delays. Skeletal x-rays show though milder phenotypes are increasingly being iden- punctate epiphyseal calcifications, metaphyseal dysplasia, and ver- tified. It is commonly caused by defects in the peroxi- tebral coronal clefts. Various abnormalities on brain magnetic reso- some transporter, PEX7 (RCDP1), and less frequently nance imaging (MRI) were reported [Bams-Mengerink et al., 2006]. -

X Linked Adrenoleukodystrophy: Clinical Presentation, Diagnosis, and Therapy
4 Journal of Neurology, Neurosurgery, and Psychiatry 1997;63:4–14 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.63.1.4 on 1 July 1997. Downloaded from REVIEW X linked adrenoleukodystrophy: clinical presentation, diagnosis, and therapy Björn M van Geel, Johanna Assies, RonaldJAWanders, Peter G Barth Abstract that has its onset in adulthood, was first X linked adrenoleukodystrophy (X-ALD) reported in 1976.4 Now, at least six diVerent is an inherited disorder of peroxisomal phenotypes are recognised.5 Not only men are metabolism, biochemically characterised aVected: in the early 1980s it was shown that by accumulation of saturated very long female carriers are at risk for developing chain fatty acids. Accumulation of these neurological deficits as well.6 fatty acids is associated with cerebral In 1976 the accumulation of saturated very demyelination, peripheral nerve abnor- long chain fatty acids (VLCFAs) in brain lipids malities, and adrenocortical and testicu- and adrenal cortex of patients with X-ALD was lar insuYciency. The lowest estimated reported.78 In 1980 raised concentrations of birth incidence is one per 100 000. At least VLCFAs were shown in cultured skin 9 10 six phenotypes can be distinguished, of fibroblasts and in 1981 in plasma, thus Department of which the two most frequent are child- providing a reliable biochemical diagnostic Neurology, Academic hood cerebral ALD and adrenomyelo- test. In 1984 a defect in peroxisomal metabo- Medical Center, 11 neuropathy. The X-ALD gene has been lism was suggested, and shortly thereafter the University of defective enzyme activity in peroxisomal Amsterdam, PO Box identified, but thus far no relation between â-oxidation of VLCFAs was discovered.12 13 In 22700, 1100 DE genotype and phenotype has been found. -

Amplification of Glyceronephosphate O-Acyltransferase and Recruitment of USP30 Stabilize DRP1 to Promote Hepatocarcinogenesis
Author Manuscript Published OnlineFirst on August 24, 2018; DOI: 10.1158/0008-5472.CAN-18-0340 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Amplification of glyceronephosphate O-acyltransferase and recruitment of USP30 stabilize DRP1 to promote hepatocarcinogenesis Li Gu #, 1, 2, Yahui Zhu #, 1, 2, Xi Lin 1, 2, Yajun Li 1, 2, Kasa Cui 1, 2, Edward V. Prochownik 3, Youjun Li 1, 2,* 1 Hubei Key Laboratory of Cell Homeostasis, College of Life Sciences, Wuhan University, Wuhan 430072, China 2 Medical Research Institute, School of Medicine, Wuhan University, Wuhan 430071, China 3Division of Hematology/Oncology, Children's Hospital of Pittsburgh of UPMC, The Department of Microbiology and Molecular Genetics and The Hillman Cancer Center of UPMC The University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania 15224, USA #These authors contributed equally. Running title: GNPAT and USP30-mediated DRP1 stabilization in HCC. *Correspondence to: Youjun Li, Hubei Key Laboratory of Cell Homeostasis, College of Life Sciences, Wuhan University, Wuhan 430072, China; Medical Research Institute, School of Medicine, Wuhan University, Wuhan 430071, China. Tel.: (86-27) 6875-2050; Fax: (86-27) 6875-2560; E-mail: [email protected] Conflict of interest: The authors declare no conflicts of interest. Downloaded from cancerres.aacrjournals.org on September 25, 2021. © 2018 American Association for Cancer Research. Author Manuscript Published OnlineFirst on August 24, 2018; DOI: 10.1158/0008-5472.CAN-18-0340 -

Inherited Peroxisomal Disorders Involving the Nervous System
Arch Dis Child: first published as 10.1136/adc.63.7.767 on 1 July 1988. Downloaded from Archives of Disease in Childhood, i988, 63, 767-770 Annotations Inherited peroxisomal disorders involving the nervous system For genetic reasons peroxisomes may be absent or defective. Because of the great importance of the lack one or more of their enzymes. The result may peroxisomal enzymes involved in the I oxidation of be subtle and long delayed, but is often catastrophic VLCFA and the use of measurements of VLCFA in and immediately recognisable as a serious disorder diagnosis, this group is itself subdivided. Group 3A at birth. The trouble for the clinician is that it is includes those conditions in which VLCFA oxidation often not possible to make a diagnosis unless the is impaired and thus VLCFA accumulates, and right tests are thought of: these tests are not part of group 3B those in which the single enzyme defect is routine 'metabolic screens.' It is first necessary to of another sort. frame the question 'could this be a peroxisomopathy?' The object of this annotation is to help with when GENERALISED PEROXISOMAL DISORDERS (GROUP 1) and how to answer this question. The now classical example is the cerebro-hepato- renal syndrome of Zellweger. l 2The typical neonate Peroxisomes is more dysmorphic than a baby with Down's syndrome with high forehead and huge fontanelle Peroxisomes are subcellular organelles with a single with metopic extension. Inactivity is even greater membrane which occur in every cell apart from the than in the Prader-Willi syndrome and hypotonia mature erythrocyte. -

Pseudo Infantile Refsum's Disease: Catalase- Deficient Peroxisomal Particles with Partial Deficiency of Plasmalogen Synthesis and Oxidation of Fatty Acids
003 I-3998/93/3403-0270$03.00/0 PEDIATRIC RESEARCH Vol. 34. No. 3. 1993 Copyright 8 1993 International Pediatric Research Foundation. Inc I'ritrrid in U S :I. Pseudo Infantile Refsum's Disease: Catalase- Deficient Peroxisomal Particles with Partial Deficiency of Plasmalogen Synthesis and Oxidation of Fatty Acids P. AUBOURG, K. KREMSER, M. 0. ROLAND. F. ROCCHICCIOLI. AND I. SlNGH ABSTRACT. Zellweger syndrome, neonatal adrenoleuko- RCDP, rhizomelic chondrodysplasia punctata dystrophy, and infantile Refsum's disease are genetic dis- IRD, infantile Refsum's disease orders characterized by the virtual absence of catalase- positive perosisomes and a general impairment of perosi- somal functions. Recent studies in these three disorders have provided morphologic evidence of perosisomal Peroxisomes are subcellular organelles that participate in the "ghosts" of density 1.10 g/cd that contain membrane @-oxidation of long-chain fatty acids and VLCFA (1-3), the proteins but lack a majority of the matrix enzyme activities. synthesis of plasmalogens (4), the oxidation of L-pipecolic acid We report here the biochemical studies in a female infant (5, 6). and bile acid synthesis (7). In addition, peroxisomes with clinical features of infantile Refsum's disease whose contain catalase that degrades the Hz02 produced by various liver and fibroblasts contained cytosolic catalase but no oxidases (8). Peroxisomes, like mitochondria. arise by growth catalase-positive peroxisomes. Oxidation of phytanic and and division of preexisting peroxisomes (9). All peroxisomal pipecolic acids was severely impaired, whereas osidation proteins studied so far are synthesized on free polyribosomes, of very-long-chain fatty acids and dihydrosyacetone phos- then translocated into preexisting peroxisomes. -

Acetate Supplementation Reduces Disease Progression, Alters Cns
University of North Dakota UND Scholarly Commons Theses and Dissertations Theses, Dissertations, and Senior Projects January 2017 Acetate Supplementation Reduces Disease Progression, Alters Cns And Myelin Lipid Content, And Influences Cns And Myelin Protein Content In Mice Subjected To Experimental Autoimmune Encephalomyelitis Amber C. Chevalier Follow this and additional works at: https://commons.und.edu/theses Recommended Citation Chevalier, Amber C., "Acetate Supplementation Reduces Disease Progression, Alters Cns And Myelin Lipid Content, And Influences Cns And Myelin Protein Content In Mice Subjected To Experimental Autoimmune Encephalomyelitis" (2017). Theses and Dissertations. 2186. https://commons.und.edu/theses/2186 This Dissertation is brought to you for free and open access by the Theses, Dissertations, and Senior Projects at UND Scholarly Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. ACETATE SUPPLEMENTATION REDUCES DISEASE PROGRESSION, ALTERS CNS AND MYELIN LIPID CONTENT, AND INFLUENCES CNS AND MYELIN PROTEIN CONTENT IN MICE SUBJECTED TO EXPERIMENTAL AUTOIMMUNE ENCEPHALOMYELITIS By Amber Christine Chevalier Bachelor of Arts, Concordia College, 2012 Dissertation Submitted to the Graduate Faculty of the University of North Dakota In partial fulfillment of the requirements For the degree of Doctor of Philosophy Grand Forks, North Dakota December 2017 Copyright 2017 Amber Chevalier ii PERMISSION Title: Acetate Supplementation Reduces Disease Progression, Alters CNS and Myelin Lipid Content, and Influences CNS and Myelin Protein Content in Mice Subjected to Experimental Autoimmune Encephalomyelitis Department: Pharmacology, Physiology, and Therapeutics Degree: Doctor of Philosophy In presenting this dissertation in partial fulfillment of the requirements for a graduate degree from the University of North Dakota, I agree that the library of this University shall make it freely available for inspection. -

Biochimica Et Biophysica Acta 1822 (2012) 1326–1336
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Biochimica et Biophysica Acta 1822 (2012) 1326–1336 Contents lists available at SciVerse ScienceDirect Biochimica et Biophysica Acta journal homepage: www.elsevier.com/locate/bbadis Review Molecular basis of peroxisomal biogenesis disorders caused by defects in peroxisomal matrix protein import☆ Shirisha Nagotu 1, Vishal C. Kalel 1, Ralf Erdmann ⁎, Harald W. Platta ⁎ Abteilung für Systembiochemie, Medizinische Fakultät der Ruhr-Universität Bochum, D-44780 Bochum, Germany article info abstract Article history: Peroxisomal biogenesis disorders (PBDs) represent a spectrum of autosomal recessive metabolic disorders Received 19 December 2011 that are collectively characterized by abnormal peroxisome assembly and impaired peroxisomal function. Received in Revised form 26 March 2012 The importance of this ubiquitous organelle for human health is highlighted by the fact that PBDs are mul- Accepted 9 May 2012 tisystemic disorders that often cause death in early infancy. Peroxisomes contribute to central metabolic Available online 19 May 2012 pathways. Most enzymes in the peroxisomal matrix are linked to lipid metabolism and detoxification of reactive oxygen species. Proper assembly of peroxisomes and thus also import of their enzymes relies on Keywords: fi Peroxisome biogenesis disorders speci c peroxisomal biogenesis factors, so called peroxins with PEX being the gene acronym. To date, 13 Zellweger syndrome spectrum PEX genes are known to cause PBDs when mutated. Studies of the cellular and molecular defects in cells PEX derived from PBD patients have significantly contributed to the understanding of the functional role of the Peroxin corresponding peroxins in peroxisome assembly. -

Genetic Classification and Mutational Spectrum of More Than 600 Patients
Genetic classification and mutational spectrum of more than 600 patients with a Zellweger syndrome spectrum disorder Merel Sanne Ebberink, Petra Mooyer, Jeannette Gootjes, Janet Koster, Ronald J.A. Wanders, Hans Waterham To cite this version: Merel Sanne Ebberink, Petra Mooyer, Jeannette Gootjes, Janet Koster, Ronald J.A. Wanders, et al.. Genetic classification and mutational spectrum of more than 600 patients with a Zellweger syn- drome spectrum disorder. Human Mutation, Wiley, 2010, 32 (1), pp.59. 10.1002/humu.21388. hal-00599469 HAL Id: hal-00599469 https://hal.archives-ouvertes.fr/hal-00599469 Submitted on 10 Jun 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Human Mutation Genetic classification and mutational spectrum of more than 600 patients with a Zellweger syndrome spectrum disorder For Peer Review Journal: Human Mutation Manuscript ID: humu-2010-0170.R1 Wiley - Manuscript type: Research Article Date Submitted by the 30-Aug-2010 Author: Complete List of Authors: Ebberink, Merel; Academic Medical Centre, University of Amsterdam, Laboratoy -
06-0718 Index: Benefits
State of California—Health and Human Services Agency Department of Health Care Services JENNIFER KENT EDMUND G. BROWN JR. DIRECTOR GOVERNOR DATE: July 10, 2018 N.L.: 06-0718 Index: Benefits TO: COUNTY CALIFORNIA CHILDREN’S SERVICES (CCS) ADMINISTRATORS, MEDICAL DIRECTORS, AND MEDICAL CONSULTANTS, INTEGRATED SYSTEMS OF CARE DIVISION (ISCD) STAFF, CCS PROGRAM-APPROVED SPECIAL CARE CENTERS (SCC) SUBJECT: AUTHORIZATION OF DIAGNOSTIC AND TREATMENT SERVICE FOR INFANTS REFERRED BY THE CALIFORNIA NEWBORN SCREENING (NBS) PROGRAM FOR X-LINKED ADRENOLEUKODYSTROPHY (ALD) I. PURPOSE The purpose of this Numbered Letter is to establish CCS policy on the authorization of diagnostic and treatment services for X-linked ALD for individuals with a positive NBS test. II. BACKGROUND X-linked ALD is an inherited peroxisomal disorder in which accumulation of very long chain fatty acids (VCLFA) in the brain, spinal cord and adrenal glands leads to demyelination in the brain and spinal cord, and impaired adrenal corticoid function in the adrenal cortex. The condition results from the mutations of the ABCD1 gene on the X chromosome. The ABCD1 gene codes for the ALD protein, which facilitates transport of VLCFA into peroxisomes. Absence of the protein results in an inability to transport and degrade VLCFA. Over 1,000 mutations associated with ALD have been identified. The incidence is between 1 in 20,000 and 1 in 50,000 births. There are multiple presentations of ALD, including childhood cerebral ALD, adolescent cerebral ALD, ‘Addison’s disease only’ and adrenomyeloneuropathy (AMN). Childhood cerebral ALD most commonly presents in boys between the ages of four to eight years old, with intellectual or behavioral impairments.