Baseline Prevalence Survey of Schistosomiasis in Maguindanao
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ethnic and Religious Conflict in Southern Philippines: a Discourse on Self-Determination, Political Autonomy, and Conflict Resolution
Ethnic and Religious Conflict in Southern Philippines: A Discourse on Self-Determination, Political Autonomy, and Conflict Resolution Jamail A. Kamlian Professor of History at Mindanao State University- ILigan Institute of Technology (MSU-IIT), ILigan City, Philippines ABSTRACT Filipina kini menghadapi masalah serius terkait populasi mioniritas agama dan etnis. Bangsa Moro yang merupakan salah satu etnis minoritas telah lama berjuang untuk mendapatkan hak untuk self-determination. Perjuangan mereka dilancarkan dalam berbagai bentuk, mulai dari parlemen hingga perjuangan bersenjata dengan tuntutan otonomi politik atau negara Islam teroisah. Pemberontakan etnis ini telah mengakar dalam sejarah panjang penindasan sejak era kolonial. Jika pemberontakan yang kini masih berlangsung itu tidak segera teratasi, keamanan nasional Filipina dapat dipastikan terancam. Tulisan ini memaparkan latar belakang historis dan demografis gerakan pemisahan diri yang dilancarkan Bangsa Moro. Setelah memahami latar belakang konflik, mekanisme resolusi konflik lantas diajukan dalam tulisan ini. Kata-Kata Kunci: Bangsa Moro, latar belakang sejarah, ekonomi politik, resolusi konflik. The Philippines is now seriously confronted with problems related to their ethnic and religious minority populations. The Bangsamoro (Muslim Filipinos) people, one of these minority groups, have been struggling for their right to self-determination. Their struggle has taken several forms ranging from parliamentary to armed struggle with a major demand of a regional political autonomy or separate Islamic State. The Bangsamoro rebellion is a deep- rooted problem with strong historical underpinnings that can be traced as far back as the colonial era. It has persisted up to the present and may continue to persist as well as threaten the national security of the Republic of the Philippines unless appropriate solutions can be put in place and accepted by the various stakeholders of peace and development. -

Emindanao Library an Annotated Bibliography (Preliminary Edition)
eMindanao Library An Annotated Bibliography (Preliminary Edition) Published online by Center for Philippine Studies University of Hawai’i at Mānoa Honolulu, Hawaii July 25, 2014 TABLE OF CONTENTS Preface iii I. Articles/Books 1 II. Bibliographies 236 III. Videos/Images 240 IV. Websites 242 V. Others (Interviews/biographies/dictionaries) 248 PREFACE This project is part of eMindanao Library, an electronic, digitized collection of materials being established by the Center for Philippine Studies, University of Hawai’i at Mānoa. At present, this annotated bibliography is a work in progress envisioned to be published online in full, with its own internal search mechanism. The list is drawn from web-based resources, mostly articles and a few books that are available or published on the internet. Some of them are born-digital with no known analog equivalent. Later, the bibliography will include printed materials such as books and journal articles, and other textual materials, images and audio-visual items. eMindanao will play host as a depository of such materials in digital form in a dedicated website. Please note that some resources listed here may have links that are “broken” at the time users search for them online. They may have been discontinued for some reason, hence are not accessible any longer. Materials are broadly categorized into the following: Articles/Books Bibliographies Videos/Images Websites, and Others (Interviews/ Biographies/ Dictionaries) Updated: July 25, 2014 Notes: This annotated bibliography has been originally published at http://www.hawaii.edu/cps/emindanao.html, and re-posted at http://www.emindanao.com. All Rights Reserved. For comments and feedbacks, write to: Center for Philippine Studies University of Hawai’i at Mānoa 1890 East-West Road, Moore 416 Honolulu, Hawaii 96822 Email: [email protected] Phone: (808) 956-6086 Fax: (808) 956-2682 Suggested format for citation of this resource: Center for Philippine Studies, University of Hawai’i at Mānoa. -

4. Resources, Security and Livelihood
Violent Conflicts and Displacement in Central Mindanao 4. RESOURCES, SECURITY AND LIVELIHOOD This section examines households’ perceptions of their surrounding environment (e.g. security). It looks at their resources or capital (social, natural, economic) available to households, as well as how those resources were being used to shape livelihood strategies and livelihood outcomes such as food security. The results give insights into the complex interaction between, on the one hand, displacement and settlement options, and, on the other hand, access to basic needs, services and livelihood strategies. Services and Social Relations Access to Services Across the study strata, about one-third of the households ranked their access to services negatively, including access to education (22%), access to (35%) and quality of (32%) health care, and access to roads (37%). Respondents in Maguindanao ranked on average all services more negatively than any other strata. Disaggregated by settlement status, respondents who were displaced at the time of the survey were more likely to rank services negatively compared to others, with the exception of access to roads. Nearly the same percentage of households who were displaced at the time of survey and those returned home found the road to be bad of very bad (47% and 55%, respectively). Figure 11: Ranking of services (% bad - very bad) Two-thirds (67%) of the sampled households had children aged 6-12 years, and among them nearly all had children enrolled in primary school (97%). However, 36 percent of the households reported that their school-enrolled children missed school for at least a week within the 6 months prior to the survey. -

Chapter 3 Socio Economic Profile of the Study Area
CHAPTER 3 SOCIO ECONOMIC PROFILE OF THE STUDY AREA 3.1 SOCIAL CONDITIONS 3.1.1 Demographic Trend 1) Population Trends by Region Philippine population has been continuously increasing from 48.1million in 1980, 76.3 million in 2000 to 88.5million in 2007 with 2.15% of annual growth rate (2000-2007). Population of both Mindanao and ARMM also showed higher increases than national trend since 2000, from 18.1 in 2000 to 21.6 million in 2007 (AAGR: 2.52%), and 2.9 in 2000 to 4.1million in 2007 (AAGR: 5.27%), respectively. Population share of Mindanao to Philippines and of ARMM to Mindanao significantly increased from 23.8% to 24.4% and 15.9% to 24.4%, respectively. 100,000,000 90,000,000 Philippines Mindanao 80,000,000 ARMM 70,000,000 60,000,000 50,000,000 40,000,000 30,000,000 20,000,000 10,000,000 0 1980 1990 1995 2000 2007 Year Source: NSO, 2008 FIGURE 3.1.1-1 POPULATION TRENDS OF PHILIPPINES, MINDANAO AND ARMM Population trends of Mindanao by region are illustrated in Figure 3.1.1-2 and the growth in ARMM is significantly high in comparison with other regions since 1995, especially from 2000 to 2007. 3 - 1 4,500,000 IX 4,000,000 X XI 3,500,000 XII XIII ARMM 3,000,000 2,500,000 2,000,000 1,500,000 1,000,000 1980 1990 1995 2000 2007 year Source NSO, 2008 FIGURE 3.1.1-2 POPULATION TRENDS BY REGION IN MINDANAO As a result, the population composition within Mindanao indicates some different features from previous decade that ARMM occupies a certain amount of share (20%), almost same as Region XI in 2007. -

Autonomous Region in Muslim Mindanao
ISSN 0116-4007 Autonomous Region in Muslim Mindanao ISSN 0116-4007 Autonomous Region in Muslim Mindanao REPUBLIC OF THE PHILIPPINES PRESIDENT RODRIGO ROA DUTERTE REPUBLIC OF THE PHILIPPINES PHILIPPINE STATISTICS AUTHORITY LISA GRACE S. BERSALES, Ph.D. National Statistician and Civil Registrar General Copyright © 2012 by Philippine Statistics Authority (PSA) PSA CVEA Building East Avenue, Diliman Quezon City, Philippines FOREWORD Over the years, the Census of Agriculture and Fisheries (CAF) has been the major source of comprehensive information on agriculture and fishery sectors in the country. The collected census data provide statistical information which can assist decision making for all sectors of society such as governments, businesses, academics, researchers, students, community organizations and individuals. The 2012 CAF was undertaken by the then National Statistics Office (NSO) in accordance with Executive Order (EO) 121, designating the said office as the "major statistical agency responsible for generating general purpose statistics" and Commonwealth Act 591 which authorized the NSO, "to prepare for and undertake all censuses of population, agriculture, industry and commerce". Moreover, EO 352, otherwise known as the Designation of Statistical Activities that will Generate Critical Data for Decision-Making of the Government and the Private Sector, provided for the conduct of census of agriculture every 10 years. Recently, Republic Act (RA) 10625 (Reorganizing and Strengthening the Philippine Statistical System and for Other Purposes) Section 6 stipulates that one function of the Philippine Statistics Authority (PSA) is "to prepare and conduct periodic censuses on population, housing, agriculture, fisheries, business, industry and other sectors of the economy". The 2012 CAF was the sixth in a series of decennial agriculture censuses and the fifth in the decennial censuses of fisheries in the country. -

MAKING the LINK in the PHILIPPINES Population, Health, and the Environment
MAKING THE LINK IN THE PHILIPPINES Population, Health, and the Environment The interconnected problems related to population, are also disappearing as a result of the loss of the country’s health, and the environment are among the Philippines’ forests and the destruction of its coral reefs. Although greatest challenges in achieving national development gross national income per capita is higher than the aver- goals. Although the Philippines has abundant natural age in the region, around one-quarter of Philippine fami- resources, these resources are compromised by a number lies live below the poverty threshold, reflecting broad social of factors, including population pressures and poverty. The inequity and other social challenges. result: Public health, well-being and sustainable develop- This wallchart provides information and data on crit- ment are at risk. Cities are becoming more crowded and ical population, health, and environmental issues in the polluted, and the reliability of food and water supplies is Philippines. Examining these data, understanding their more uncertain than a generation ago. The productivity of interactions, and designing strategies that take into the country’s agricultural lands and fisheries is declining account these relationships can help to improve people’s as these areas become increasingly degraded and pushed lives while preserving the natural resource base that pro- beyond their production capacity. Plant and animal species vides for their livelihood and health. Population Reference Bureau 1875 Connecticut Ave., NW, Suite 520 Washington, DC 20009 USA Mangroves Help Sustain Human Vulnerability Coastal Communities to Natural Hazards Comprising more than 7,000 islands, the Philippines has an extensive coastline that is a is Increasing critical environmental and economic resource for the nation. -
Supporting People Affected by Conflict and Covid-19 Icrc Activities in the Philippines, January-July 2021
SUPPORTING PEOPLE AFFECTED BY CONFLICT AND COVID-19 ICRC ACTIVITIES IN THE PHILIPPINES, JANUARY-JULY 2021 The COVID-19 pandemic continued to pose major challenges to the its services and get feedback, illustrating its commitment to be Philippines. Despite the vaccination rollout, there were case surges accountable to affected people. due to new variant threats. The ICRC also resumed its operational visits in the Visayas, aimed To help overwhelmed health systems, the International at addressing the consequences of conflict on civilians in Samar Committee of the Red Cross (ICRC) ensured protective equipment and Negros islands. for health workers in COVID-19 referral hospitals in Mindanao, In the most congested detention facilities, efforts to enhance and in isolation centers for detainees. It also quickly assisted the detainees’ overall access to clean water, sanitation and Philippine Red Cross’ (PRC) COVID-19 response in support of healthcare—particularly for those with tuberculosis or were government efforts to address the surge. undernourished—were reinvigorated by support to and dialogue Meanwhile, armed conflicts displaced thousands of people in with detention authorities. Maguindanao, Caraga, Northern Mindanao and Zambasulta High-level and field operational dialogue with state forces (and regions; while many others still bear the long-term consequences some non-state armed groups) intensified through technical of the 2017 Marawi conflict. The ICRC, often in partnership with the working groups aimed at preventing or raising concerns regarding PRC, provided relief items and clean water for displaced families; potential international humanitarian law (IHL) violations. This and distributed cash grants and micro-economic initiatives to is alongside endeavors to promote better understanding and revive livelihoods. -

Income Classification Per DOF Order No. 23-08, Dated July 29, 2008 MUNICIPALITIES Classification NCR 1
Income Classification Per DOF Order No. 23-08, dated July 29, 2008 MUNICIPALITIES Classification NCR 1. Pateros 1st CAR ABRA 1 Baay-Licuan 5th 2 Bangued 1st 3 Boliney 5th 4 Bucay 5th 5 Bucloc 6th 6 Daguioman 5th 7 Danglas 5th 8 Dolores 5th 9 La Paz 5th 10 Lacub 5th 11 Lagangilang 5th 12 Lagayan 5th 13 Langiden 5th 14 Luba 5th 15 Malibcong 5th 16 Manabo 5th 17 Penarrubia 6th 18 Pidigan 5th 19 Pilar 5th 20 Sallapadan 5th 21 San Isidro 5th 22 San Juan 5th 23 San Quintin 5th 24 Tayum 5th 25 Tineg 2nd 26 Tubo 4th 27 Villaviciosa 5th APAYAO 1 Calanasan 1st 2 Conner 2nd 3 Flora 3rd 4 Kabugao 1st 5 Luna 2nd 6 Pudtol 4th 7 Sta. Marcela 4th BENGUET 1. Atok 4th 2. Bakun 3rd 3. Bokod 4th 4. Buguias 3rd 5. Itogon 1st 6. Kabayan 4th 7. Kapangan 4th 8. Kibungan 4th 9. La Trinidad 1st 10. Mankayan 1st 11. Sablan 5th 12. Tuba 1st blgf/ltod/updated 1 of 30 updated 4-27-16 Income Classification Per DOF Order No. 23-08, dated July 29, 2008 13. Tublay 5th IFUGAO 1 Aguinaldo 2nd 2 Alfonso Lista 3rd 3 Asipulo 5th 4 Banaue 4th 5 Hingyon 5th 6 Hungduan 4th 7 Kiangan 4th 8 Lagawe 4th 9 Lamut 4th 10 Mayoyao 4th 11 Tinoc 4th KALINGA 1. Balbalan 3rd 2. Lubuagan 4th 3. Pasil 5th 4. Pinukpuk 1st 5. Rizal 4th 6. Tanudan 4th 7. Tinglayan 4th MOUNTAIN PROVINCE 1. Barlig 5th 2. Bauko 4th 3. Besao 5th 4. -

Chapter 5 Existing Conditions of Flood and Disaster Management in Bangsamoro
Comprehensive capacity development project for the Bangsamoro Final Report Chapter 5. Existing Conditions of Flood and Disaster Management in Bangsamoro CHAPTER 5 EXISTING CONDITIONS OF FLOOD AND DISASTER MANAGEMENT IN BANGSAMORO 5.1 Floods and Other Disasters in Bangsamoro 5.1.1 Floods (1) Disaster reports of OCD-ARMM The Office of Civil Defense (OCD)-ARMM prepares disaster reports for every disaster event, and submits them to the OCD Central Office. However, historic statistic data have not been compiled yet as only in 2013 the report template was drafted by the OCD Central Office. OCD-ARMM started to prepare disaster reports of the main land provinces in 2014, following the draft template. Its satellite office in Zamboanga prepares disaster reports of the island provinces and submits them directly to the Central Office. Table 5.1 is a summary of the disaster reports for three flood events in 2014. Unfortunately, there is no disaster event record of the island provinces in the reports for the reason mentioned above. According to staff of OCD-ARMM, main disasters in the Region are flood and landslide, and the two mainland provinces, Maguindanao and Lanao Del Sur are more susceptible to disasters than the three island provinces, Sulu, Balisan and Tawi-Tawi. Table 5.1 Summary of Disaster Reports of OCD-ARMM for Three Flood Events Affected Damage to houses Agricultural Disaster Event Affected Municipalities Casualties Note people and infrastructures loss Mamasapano, Datu Salibo, Shariff Saydona1, Datu Piang1, Sultan sa State of Calamity was Flood in Barongis, Rajah Buayan1, Datu Abdulah PHP 43 million 32,001 declared for Maguindanao Sangki, Mother Kabuntalan, Northern 1 dead, 8,303 ha affected. -

Enduring Wars
CONFLICT ALERT 2020 Enduring Wars Peace is within our power About Conflict Alert Conflict Alert is a subnational conflict monitoring system that tracks the incidence, causes, and human costs of violent conflict in the Philippines. It aims to shape policymaking, development strategies, and peacebuilding approaches by providing relevant, robust, and reliable conflict data. Conflict Alert was developed and is run by the Philippines Programme of International Alert, an independent peacebuilding organization. www.conflictalert.info About International Alert International Alert helps find peaceful solutions to conflict. We are one of the world’s leading peacebuilding organizations with nearly 30 years of experience laying the foundations for peace. We work with local people around the world to help them build peace, and we advise governments, organizations, and companies on how to support peace. We focus on issues that influence peace, including governance, economics, gender relations, social development, climate change, and the role of business and international organizations in high-risk places. www.international-alert.org This project receives funding from The World Bank Group and the Department of Foreign Affairs and Trade of the Australian Government. The opinions expressed in this report are solely those of International Alert and do not necessarily reflect the opinions or policies of our donors. © International Alert 2020 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted -
NUTRIENT STATUS MAP : MAGNESIUM ( Key Corn Areas )
124°0' 124°20' 124°40' 125°0' Mamasapano Datu Unsay Shariff Saydona Mustapha Sultan sa Barongis LIGUASAN MARSH Shariff Aguak South Upi R E G I O N X I I Datu Hoffer Ampatuan Province of North Cotabato ARMM Ampatuan Gen S.K. Pendatun Province of Maguindanao Tulunan Lambayong ! Datu Abdullah Sangki Paglat Pandag ARMM Datu Paglas L i n a o B a y Province of Maguindanao Esperanza ! Buluan President Quirino ! Tacurong ^ Columbio ! R E G I O N X I Province of Davao del Sur 6°40' 6°40' Mangudadatu Isulan Lebak ! P LAKE BULUAN Lutayan ! Tantangan Kalamansig ! Bagumbayan ! Norala R E G I O N X I I Koronadal Province of South Cotabato R E P U B L I C O F T H E P H I L I P P I N E S Tampakan DEPARTMENT OF AGRICULTURE BUREAU OF SOILS AND Basiauang Bay WATER MANAGEMENT Sen. Ninoy Aquino ! Elliptical Road Cor. Visayas Ave., Diliman, Quezon City Sto. Niño NUTRIENT STATUS MAP : MAGNESIUM ( Key Corn Areas ) Banga PROVINCE OF SULTAN KUDARAT ° SCALE 1:110,000 0 2 4 6 8 10 Kilometers Projection : Transverse Mercator Datum : PRS 1992 Surallah DISCLAIMER : All political boundaries are not authoritative T u n a B a y Tupi LOCATION MAP 6°20' 6°20' LEGENDLEGEND 20°0' AREA Exchangeable Mg, Cotabato North Cotabato MAPPING UNIT DESCRIPTION City cmol/kg ha % 7°0' Maguindanao LUZON 15°0' Sufficient > 1.0 10,412 49.33 Davao del Sur R E G I O N X I I SULTAN KUDARAT B a s i a ua n g B a y South Cotabato Deficient 1.0 and below 10,696 50.67 10°0' Province of South Cotabato VISAYAS 6°0' T O T A L 21,108 100.00 Sarangani Lake Lahit Area estimated based on field survey, other information from DA-RFO's, MA's, NIA Service Area, NAMRIA Land Cover CELEBES SEA MINDANAO 5°0' (2010), and BSWM Land Use System Map 124°0' 125°0' 120°0' 125°0' Lake Sultan LAKE SEBU Lake Sebu T'boli Polomolok Palimbang ! CONVENTIONAL SIGNS MISCELLANEOUS INFORMATION ROADS BOUNDARY HYDROLOGY SOURCES OF INFORMATION : Topographic information taken from NAMRIA Topographic Map at a scale of 1:50,000. -

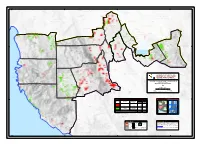
IOM Philippines - Response to Displacement Due to Conflict in Mindanao 12 March 2015 SITUATION REPORT # 5
IOM Philippines - Response to displacement due to conflict in Mindanao 12 March 2015 SITUATION REPORT # 5 Map of the latest displacement overview in Central Mindanao © IOM 2015 ARMED CONFLICT BETWEEN PHILIPPINE NATIONAL Municipality Affected POLICE SPECIAL ACTION FORCE AND ARMED Brgys Families Persons GROUPS ERUPTS IN MAMASAPANO Shariff Say- 6 1,864 9,320 dona BACKGROUND Mamasapano 15 2,637 13,185 Datu Unsay 4 175 875 Due to the continued tension between the Moro Islamic Liberation Front (MILF) and the Bangsamoro Islamic Freedom Fighters (BIFF), since 9 Feb- Shariff Aguak 6 1,373 6,865 ruary 2015, again a firefight has erupted between these groups at Datu Salibo 7 2,119 10,595 around 5:00 pm on Saturday, 13 February 2015 in the Barangays Buliok Datu Saudi 7 1,062 5,310 and Kalbugan, Pagalungan, Maguindanao Province. The conflict has Ampatuan affected thousands of civilians from the villages of Buliok, Kalbugan and Rajah Buay- No data 255 1,275 Bagoinged, Pagalungan, Maguindanao, where internally displaced per- an sons continue to flee their homes to avoid being caught in a cross fire. Talayan No data 1,195 5,975 Guindulungan No data 939 4,695 The table on the right side and the map above show the municipalities affected by the conflict and the number of families and individuals that Talitay No data 712 3,560 have been affected. According to ARMM HEART (7 March 2015) overall, Datu Anggal No data 589 2,945 12,920 families or 64,600 individuals have been affected in 11 municipal- Midtimbang ities, in Central Mindanao.