Preventing Sports Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hockey Apparel Free Shipping
Hockey apparel free shipping Discounts average $11 off with a NHL Shop promo code or coupon. 34 NHL Shop coupons now on RetailMeNot. NHL Draft Hats Available 2, - Dec 31, Discounts average $10 off with a Gongshow Lifestyle Hockey Apparel promo code or coupon. 37 Gongshow Lifestyle Hockey Apparel coupons now on May 4, - Dec 31, No Sales Tax. Except CA. Free Same Day Shipping. On all orders over $ & before 4PM EST. Day Returns. Now easier than ever! Contact · Login. Discount Hockey carries the best selection of hockey equipment, ice skates, sticks, helmets, gloves, accessories, custom jerseys, goalie equipment, and more!Clearance · Skates · Sticks · Helmets. 50 best Gongshow Lifestyle Hockey Apparel coupons and promo codes. Save big on apparel and accessories. Today's top deal: $30 off. 8 verified NHL coupons and promo codes as of Oct Shop NHL Kid's Apparel The Hot Off The Ice sales section has discount merchandise of all types. Shop clearance hockey apparel & gear at DICK'S Sporting Goods today. Check out customer reviews and learn more about these great products. 29 Promo Codes for | Today's best offer is: Free Shipping on orders San Jose Sharks Western Conference Champions Fan Gear starting at $ women and kids. Get the latest NHL clothing and exclusive gear at hockey fan's favorite shop. Adidas Authentic NHL Jerseys; 9. NHL Coupons & Promos. Save up to 60% on select merchandise from ! Buy discounted shirts, hats, sweatshirts, and more apparel from the official store of the NHL. with coupon code ITP. coupons and deals also available for October Shop vintage NHL apparel with prices starting at $ NHL Shop Coupons, Promo Codes, and Discounts. -

CASE 11 Sports League Issues: the Relocation of the Los Angeles
CASE 11 Sports League Issues: The Relocation of the Los Angeles Rams to St. Louis (1998) Franklin M. Fisher, Christopher Maxwell, and Evan Sue Schouten INTRODUCTION Sports leagues raise unique antitrust issues. Although most leagues consist of a collection of separately owned teams, each team is dependent on the others. No team could play even a single game without the cooperation of another team, and the production of a season of sports games, culminating in a championship, requires the joint efforts of all of the teams in the league. As a result, the question arises whether such a league is a single entity or a group of cooperating competitors. Are the league’s rules pro-competitive, or do they constitute collusive restraint of trade? Such issues have often challenged the courts. Their resolution is made no easier by the fact that they often arise in a proceeding brought by one of a league’s member teams against the league or against the other members. In such cases, the plaintiff team often asserts that the league’s rules are an- ticompetitive restraints on the freedom of its members. Evidently, there are situations in which the interests of a league as a whole and those of one or more individual members fail to coincide. Nowhere has this phenomenon been more evident than in cases in- volving the relocation of team franchises. In the National Football League (NFL, or “the League”), the most famous cases are those stemming from Portions of this chapter were taken from Fisher et al. (2000). 277 THE ANTITRUST REVOLUTION the move of the Oakland Raiders to Los Angeles and then back again.1 Partly in response to the 1984 and 1986 cases, the NFL developed a process for making relocation decisions, a process that sometimes involves a relo- cation fee paid to the League. -

Development, Evolution, and Bargaining in the National Football League
DEVELOPMENT, EVOLUTION, AND BARGAINING IN THE NATIONAL FOOTBALL LEAGUE Thomas Sisco The National Football League [hereinafter: NFL] is the most popular professional sports organization in the United States, but even with the current popularity and status of the NFL, ratings and the public perception of the on-field product have been on steady decline.1 Many believe this is a byproduct of the NFL being the only one of the 4 major professional sports leagues in the country without a self-controlled system for player development. Major League Baseball [hereinafter: MLB] has a prominent and successful minor league baseball system, the National Hockey League has the American Hockey League and East Coast Hockey League, the National Basketball Association [hereinafter: NBA] has the 22 team development league widely known as “The D- League”, but the NFL relies on the National Collegiate Athletic Association [hereinafter: NCAA] to develop young players for a career in their league. The Canadian Football League and the Arena Football League are generally inadequate in developing players for the NFL as the rules of gameplay and the field dimensions differ from those of NFL football.2 NFL Europe, a developmental league founded by Paul Tagliabue, former NFL Commissioner, has seen minor success.3 NFL Europe, existing by various names during its lifespan, operated from 1991 until it was disbanded in 2007.4 During its existence, the NFL Europe served as a suitable incubator for a 1 Darren Rovell, NFL most popular for 30th year in row, ESPN (January 26, 2014), http://www.espn.com/nfl/story/_/id/10354114/harris-poll-nfl-most-popular-mlb-2nd, . -
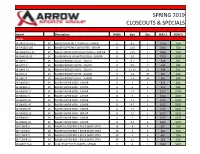
Spring 2019 Closeouts & Specials
SPRING 2019 CLOSEOUTS & SPECIALS Item # Description Width Size Qty WAS $ NOW $ SKATES SK-BAS170J-45EE SK BAUER SUPREME 170 SKATES - JUNIOR EE 4.5 1 $150 $50 SK-BA160S-105 SK BAUER SUPREME S160 SKATES - SENIOR D 10.5 2 $162 $50 SK-BAX600S-115 SK BAUER VAPOR X600 SKATES (2015) - SENIOR D 11.5 1 $242 $50 SK-BAN1NS-10 SK BAUER NEXUS 1N SKATES (2016) - SENIOR D 10 1 $720 $250 SK-BAPY-7 SK BAUER PRODIGY SKATE - YOUTH R 6-7 5 $48 $35 SK-BAPY-9 SK BAUER PRODIGY SKATE - YOUTH R 8-9 9 $48 $35 SK-BAPY-13 SK BAUER PRODIGY SKATE - YOUTH R 12-13 11 $48 $35 SK-BAPJ-2 SK BAUER PRODIGY SKATE - JUNIOR R 1-2 29 $60 $40 SK-BAPJ-4 SK BAUER PRODIGY SKATE - JUNIOR R 3-4 34 $60 $40 SK-BX400J-2 SK BAUER VAPOR X400 - JUNIOR R 2 2 $73 $49 SK-BX400J-4 SK BAUER VAPOR X400 - JUNIOR R 4 2 $73 $49 SK-BX600J-15 SK BAUER VAPOR X600 - JUNIOR D 1.5 1 $152 $105 SK-BX600J-3 SK BAUER VAPOR X600 - JUNIOR D 3 5 $152 $105 SK-BX600J-35 SK BAUER VAPOR X600 - JUNIOR D 3.5 2 $152 $105 SK-BX600J-45 SK BAUER VAPOR X600 - JUNIOR D 4.5 1 $152 $105 SK-BX600J-55 SK BAUER VAPOR X600 - JUNIOR D 5.5 2 $152 $105 SK-BX600S-12 SK BAUER VAPOR X600 - SENIOR D 12 1 $237 $150 SK-BX800J-2 SK BAUER VAPOR X800 - JUNIOR D 2 1 $265 $175 SK-BX800J-25 SK BAUER VAPOR X800 - JUNIOR D 2.5 3 $265 $175 SB-TLS4ER-4 SB BAUER LIGHTSPEED 4 EDGE SKATE STEEL JR 4 4 $62 $50 SB-TLS4ER-6 SB BAUER LIGHTSPEED 4 EDGE SKATE STEEL SR 6 6 $62 $50 SB-TLS4ER-7 SB BAUER LIGHTSPEED 4 EDGE SKATE STEEL SR 7 6 $62 $50 SB-TLS4ER-11 SB BAUER LIGHTSPEED 4 EDGE SKATE STEEL SR 11 6 $62 $50 SK-CMJFT1S-6 SK CCM JETSPEED FT1 SKATES - SENIOR -
Nfhs Rules Changes Affecting Risk (1982-2013)
NFHS RULES CHANGES AFFECTING RISK (1982-2013) Baseball 1982 Batting helmets meeting NOCSAE Standard to be required in 1985. Slippery tape on bat handles is illegal. 1983 Any player warming up a pitcher at any location shall wear a protective cup and a mask with a throat protector Casts, splints or braces must be padded and there shall be no exposed metal or any other hard material. Prosthesis that is not dangerous will be permitted. 1984 Any on-deck batter is required to wear a batting helmet. Protective devices attached to a batting helmet must be approved by the state association. Nontraditional playing equipment must be reviewed by the NFHS Baseball Rules Committee before it will be permitted. A player who maliciously runs into a fielder is to be ejected and shall also be called out. Metal cleats were prohibited. 1985 Devices or attachments that cause bat handles to become flush with the knob are illegal. Only bats may be used in loosening up. 1986 Exterior warning label is mandatory on batting helmets. Players in coaches’ boxes required to wear a head protector. Jewelry is prohibited. Medical-alert bracelets or medical-alert necklaces are legal if taped to the body. 1987 Bases with tapered edges are permitted. On-deck circles should be placed 37’ away from home plate if space permits. Otherwise, they should be placed a safe distance to the side and away from home plate. 1988 Bases designed to disengage their anchor systems for safety purposes are legal. 1989 Metal cleats are permitted. 1989 By state association adoption, a double first base is permitted. -

The NFL Salary Cap and Veteran Players' Salaries
Archives of Business Research – Vol.5, No.7 Publication Date: July. 25, 2017 DOI: 10.14738/abr.57.3436. McIntyre, K. H. (2017). The NFL Salary Cap and Veteran Players’ Salaries. Archives of Business Research, 5(7), 1-11. The NFL Salary Cap and Veteran Players’ Salaries K. H. McIntyre Department of Economics & Business Administration McDaniel College, Westminster, MD, USA ABSTRACT The salary structure and process of wage determination in the American National Football League (NFL) is perhaps unique among professional sports: contracts are not guaranteed, careers tend to be very short, and the league operates under a salary cap that limits teams’ payrolls. Thus, while a fairly well-defined set of performance metrics exists for most professional football players, the usual relationship between measured performance and compensation—i.e. higher productivity translates into higher pay - may be blurred, empirically observable, or even nonexistent. This paper investigates this issue using a four-year panel of veteran professional football players. Our analysis suggests that although performance plays a role in determining salaries in the NFL, experience, durability, and mobility are the most important factors veteran player compensation. Keywords: National Football League (NFL), professional athletics, wage determination, salary cap. INTRODUCTION Anyone who has ever listened to sports talk radio knows that the pay scale for professional athletes is one of the favorite topics of discussion among sports fans and members of the media, especially around draft days, free agency periods, and trade deadlines. This should not be surprising: the business of sports has never been bigger or more closely scrutinized, and athletics and sundry merchandising more aggressively marketed; professional athletes’ salaries are simply part of this trend. -
MLS As a Sports Product – the Prominence of the World's Game in the U.S
MLS as a Sports Product – the Prominence of the World’s Game in the U.S. Stephen A. Greyser Kenneth Cortsen Working Paper 21-111 MLS as a Sports Product – the Prominence of the World’s Game in the U.S. Stephen A. Greyser Harvard Business School Kenneth Cortsen University College of Northern Denmark (UCN) Working Paper 21-111 Copyright © 2021 by Stephen A. Greyser and Kenneth Cortsen. Working papers are in draft form. This working paper is distributed for purposes of comment and discussion only. It may not be reproduced without permission of the copyright holder. Copies of working papers are available from the author. Funding for this research was provided in part by Harvard Business School. MLS as a Sports Product – the Prominence of the World’s Game in the U.S. April 8, 2021 Abstract The purpose of this Working Paper is to analyze how soccer at the professional level in the U.S., with Major League Soccer as a focal point, has developed over the span of a quarter of a century. It is worthwhile to examine the growth of MLS from its first game in 1996 to where the league currently stands as a business as it moves past its 25th anniversary. The 1994 World Cup (held in the U.S.) and the subsequent implementation of MLS as a U.S. professional league exerted a major positive influence on soccer participation and fandom in the U.S. Consequently, more importance was placed on soccer in the country’s culture. The research reported here explores the league’s evolution and development through the cohesion existing between its sporting and business development, as well as its performance. -

Team Payroll Versus Performance in Professional Sports: Is Increased Spending Associated with Greater Success?
Team Payroll Versus Performance in Professional Sports: Is Increased Spending Associated with Greater Success? Grant Shorin Professor Peter S. Arcidiacono, Faculty Advisor Professor Kent P. Kimbrough, Seminar Advisor Duke University Durham, North Carolina 2017 Grant graduated with High Distinction in Economics and a minor in Statistical Science in May 2017. Following graduation, he will be working in San Francisco as an Analyst at Altman Vilandrie & Company, a strategy consulting group that focuses on the telecom, media, and technology sectors. He can be contacted at [email protected]. Acknowledgements I would like to thank my thesis advisor, Peter Arcidiacono, for his valuable guidance. I would also like to acknowledge my honors seminar instructor, Kent Kimbrough, for his continued support and feedback. Lastly, I would like to recognize my honors seminar classmates for their helpful comments throughout the year. 2 Abstract Professional sports are a billion-dollar industry, with player salaries accounting for the largest expenditure. Comparing results between the four major North American leagues (MLB, NBA, NHL, and NFL) and examining data from 1995 through 2015, this paper seeks to answer the following question: do teams that have higher payrolls achieve greater success, as measured by their regular season, postseason, and financial performance? Multiple data visualizations highlight unique relationships across the three dimensions and between each sport, while subsequent empirical analysis supports these findings. After standardizing payroll values and using a fixed effects model to control for team-specific factors, this paper finds that higher payroll spending is associated with an increase in regular season winning percentage in all sports (but is less meaningful in the NFL), a substantial rise in the likelihood of winning the championship in the NBA and NHL, and a lower operating income in all sports. -
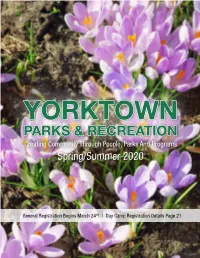
Parks & Recreation
YORKTOWN PARKS & RECREATION Creating Community Through People, Parks And Programs Spring/Summer 2020 General Registration Begins March 24th! | Day Camp Registration Details Page 21 TABLE OF CONTENTS Staff Lists/Contact Information .......................................1 Golf & Tennis .............................................................15-16 Yorktown Supervisor Letter .............................................1 Youth Sports & Specialty Camps .............................16-20 Registration/Refund & Important Information ............2 Day Camps .................................................................21-23 Special Events .....................................................................3 Aquatics Programs ..........................................................23 Town Parades .....................................................................3 Pool/Beach Information & Hours .................................24 Special Programs & Vacation Camps .............................4 Pool Pass Memberships ............................................24-25 Pre-School Programs - Youth Programs ....................4-6 Cooperating Agencies .....................................................26 Youth - Teen Programs ...............................................7-10 Program Registration Form ...........................................26 Adult Sports Information & Activities .....................9-13 Camper Registration & Medical Form ...................27-28 Senior Citizen Programs ..........................................13-15 -

The Impact of Designated Players in Major League Soccer
Superstar Salaries and Soccer Success: The Impact of Designated Players in Major League Soccer Dennis Coates Department of Economics University of Maryland, Baltimore County Bernd Frick Department of Management University of Paderborn Todd Jewell Department of Economics University of North Texas December 2012 Abstract This study estimates the relationship between production and salary structure in Major League Soccer (MLS), the highest level of professional soccer (association football) in North America. Soccer production, measured as league-points-per- game, is modeled as a function of a team’s total wage bill, the distribution of the team’s wage bill, and goals per game. Both the gini coefficient and the coefficient of variation are utilized to measure salary inequality. The results indicate that production in MLS is negatively responsive to increases in the salary inequality; this effect is consistently significant when using the coefficient of variation to measure dispersion. 1 I. Introduction Economic theory indicates that the distribution of salaries can affect the productivity of workers and firms. In the theory of tournaments, Lazear and Rosen (1981) discuss the possibility that greater salary inequality can lead to more worker effort and increased productivity. However, cohesion theory (Levine, 1991) implies firms may be able to increase the productivity of workers by equalizing salaries, since a more equal salary distribution will increase unity within the firm. The implication is that firms with more equal salary distributions will be more productive than similar firms with less equal salary structures. The present study attempts to shed light on the question of the connection between salary structure and productivity using professional sports data. -

COVID-19 RETURN to PLAY PROTOCOLS & GUIDELINES • We
COVID-19 RETURN TO PLAY PROTOCOLS & GUIDELINES We’re committed to providing the highest levels of safety for our community. To ensure player and staff safety, we have implemented mandatory 'Safe Return to Play Guidelines' for all Club Activities. In order to play with FCSSC and stay in good standing, the following guidelines MUST be followed. To ensure a successful season, please remember to practice safe physical distancing and a positive attitude! All players are required to read, understand, and adhere to the following: 1. Safe Return to Play Guidelines 2. COVID-19 League Changes 3. Self Screening Tool (done before each game). 4. Sport-Specific Rule Modifications outlined below PLUS, 5. Facility specific COVID-19 Protocols (you can find these protocols in the facility link in your schedule once live). TEAM HEALTH AMBASSADOR (THA) All teams must assign a Team Health Ambassador (THA) for the season. The THA must be a registered player and identified using the “THA” label in your online roster. THA Role: o Keep a record of attendance at each game. This record may be called upon for contact tracing. o Ensure individual wellness checks “COVID-19 Self Screening” are completed by each player prior to each game. o Ask players to leave the game if they arrive showing symptoms of cold or flu. o Ensure physical distancing measures are enforced by your team. Physical distancing of two meters is mandatory when players are arriving on-site, playing the sport, resting/sitting on the sidelines, and departing the game. o Sport-specific rules may adjust physical distancing measures taken on the playing surface. -
Ccm-Team-Catalog-2020
CCM HOCKEY 2020 TEAM PRODUCT GUIDE WEBSITE CCMHOCKEY.COM TO START YOUR B2B ONLINE SHOPPING, GO TO WWW.GO2CCMHOCKEY.COM AND CLICK ON “REQUEST LOGIN”. FIND US ON SOCIAL MEDIA WWW.FACEBOOK.COM/CCMHOCKEY @CCMHOCKEY CCMHOCKEY CCM_OFFICIAL HEAD OFFICE LOCATIONS NORTH CCM HOCKEY © 2019 SPORT MASKA INC. ALL RIGHTS RESERVED. CCM®, SUPERTACKS®, RIBCOR® AND THE CCM STYLIZED LOGO REGISTERED TRADEMARKS OF SPORT MASKA INC. AMERICA 3400, RAYMOND-LASNIER, MONTRÉAL, QUÉBEC H4R 3L3 NHL AND THE NHL SHIELD ARE REGISTERED TRADEMARKS OF THE NATIONAL HOCKEY LEAGUE. ALL NHL LOGOS AND MARKS AND TEAM LOGOS AND MARKS DEPICTED HEREIN ARE THE PROPERTY OF THE NHL AND THE RESPECTIVE TEAMS AND MAY NOT BE REPRODUCED WITHOUT THE PRIOR WRITTEN CONSENT OF NHL ENTERPRISES, L.P. © NHL CANADA 2019. ALL RIGHTS RESERVED. © PHOTOS: GETTY IMAGES. TEL.: (800) 636-5895 FAX: (800) 636-5751 † : THIS CATALOG MAY REFER TO THE FOLLOWING TRADEMARKS WHICH ARE OWNED BY THE COMPANIES WHOSE NAMES APPEAR AFTER THE TRADEMARK: AHL - - AMERICAN HOCKEY LEAGUE; CLARINO - - HURARAY CO. LTD.; CHL - - CANADIAN HOCKEY LEAGUE; LYCRA, SPANDEX AND SURLYN - - E.I. DUPONT DE NEMOURS AND COMPANY; ECHL - - ECHL EUROPE CCM HOCKEY AB INC.; PLAYDRY - - REEBOK INTERNATIONAL LTD; TACTEL - - INVISTA; VELCRO - - VELCRO INDUSTRIES B.V.; THINSULATE IS A TRADEMARK OF 3M, USED UNDER LICENSE IN GÅRDSVÄGEN 13 CANADA; D3O® - - DESIGN BLUE LTD.; JETSPEED - - TAYLORMADE GOLF COMPANY INC.; SIGMATEX - - SIGMATEX (UK) LIMITED; POLYGIENE - - POLYGIENE AB SE 16970 SOLNA WARNING : HOCKEY IS A DANGEROUS COLLISION SPORT. WE RECOMMEND THAT PROTECTIVE EQUIPMENT AND A CERTIFIED HELMET BE WORN AT ALL TIMES. SWEDEN TEL.: + 46 (0) 8 522 352 00 SPORT MASKA INC.