Mental Health System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
North America Other Continents
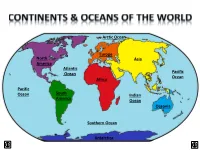
Arctic Ocean Europe North Asia America Atlantic Ocean Pacific Ocean Africa Pacific Ocean South Indian America Ocean Oceania Southern Ocean Antarctica LAND & WATER • The surface of the Earth is covered by approximately 71% water and 29% land. • It contains 7 continents and 5 oceans. Land Water EARTH’S HEMISPHERES • The planet Earth can be divided into four different sections or hemispheres. The Equator is an imaginary horizontal line (latitude) that divides the earth into the Northern and Southern hemispheres, while the Prime Meridian is the imaginary vertical line (longitude) that divides the earth into the Eastern and Western hemispheres. • North America, Earth’s 3rd largest continent, includes 23 countries. It contains Bermuda, Canada, Mexico, the United States of America, all Caribbean and Central America countries, as well as Greenland, which is the world’s largest island. North West East LOCATION South • The continent of North America is located in both the Northern and Western hemispheres. It is surrounded by the Arctic Ocean in the north, by the Atlantic Ocean in the east, and by the Pacific Ocean in the west. • It measures 24,256,000 sq. km and takes up a little more than 16% of the land on Earth. North America 16% Other Continents 84% • North America has an approximate population of almost 529 million people, which is about 8% of the World’s total population. 92% 8% North America Other Continents • The Atlantic Ocean is the second largest of Earth’s Oceans. It covers about 15% of the Earth’s total surface area and approximately 21% of its water surface area. -

Barbados and the Eastern Caribbean
Integrated Country Strategy Barbados and the Eastern Caribbean FOR PUBLIC RELEASE FOR PUBLIC RELEASE Table of Contents 1. Chief of Mission Priorities ................................................................................................................ 2 2. Mission Strategic Framework .......................................................................................................... 3 3. Mission Goals and Objectives .......................................................................................................... 5 4. Management Objectives ................................................................................................................ 11 FOR PUBLIC RELEASE Approved: August 15, 2018 1 FOR PUBLIC RELEASE 1. Chief of Mission Priorities Our Mission is accredited bilaterally to seven Eastern Caribbean (EC) island nations (Antigua and Barbuda; Barbados; Dominica; Grenada; St. Kitts and Nevis; St. Lucia; and St. Vincent and the Grenadines) and to the Organization of Eastern Caribbean States (OECS). All are English- speaking parliamentary democracies with stable political systems. All of the countries are also Small Island Developing States. The U.S. has close ties with these governments. They presently suffer from inherently weak economies, dependent on tourism, serious challenges from transnational crime, and a constant threat from natural disasters. For these reasons, our engagement focuses on these strategic challenges: Safety, Security, and Accountability for American Citizens and Interests Energy -

1 Executive Summary Mauritius Is an Upper Middle-Income Island Nation
Executive Summary Mauritius is an upper middle-income island nation of 1.2 million people and one of the most competitive, stable, and successful economies in Africa, with a Gross Domestic Product (GDP) of USD 11.9 billion and per capita GDP of over USD 9,000. Mauritius’ small land area of only 2,040 square kilometers understates its importance to the Indian Ocean region as it controls an Exclusive Economic Zone of more than 2 million square kilometers, one of the largest in the world. Emerging from the British colonial period in 1968 with a monoculture economy based on sugar production, Mauritius has since successfully diversified its economy into manufacturing and services, with a vibrant export sector focused on textiles, apparel, and jewelry as well as a growing, modern, and well-regulated offshore financial sector. Recently, the government of Mauritius has focused its attention on opportunities in three areas: serving as a platform for investment into Africa, moving the country towards renewable sources of energy, and developing economic activity related to the country’s vast oceanic resources. Mauritius actively seeks investment and seeks to service investment in the region, having signed more than forty Double Taxation Avoidance Agreements and maintaining a legal and regulatory framework that keeps Mauritius highly-ranked on “ease of doing business” and good governance indices. 1. Openness To, and Restrictions Upon, Foreign Investment Attitude Toward FDI Mauritius actively seeks and prides itself on being open to foreign investment. According to the World Bank report “Investing Across Borders,” Mauritius has one of the world’s most open economies to foreign ownership and is one of the highest recipients of FDI per capita. -
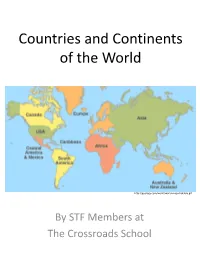
Countries and Continents of the World: a Visual Model
Countries and Continents of the World http://geology.com/world/world-map-clickable.gif By STF Members at The Crossroads School Africa Second largest continent on earth (30,065,000 Sq. Km) Most countries of any other continent Home to The Sahara, the largest desert in the world and The Nile, the longest river in the world The Sahara: covers 4,619,260 km2 The Nile: 6695 kilometers long There are over 1000 languages spoken in Africa http://www.ecdc-cari.org/countries/Africa_Map.gif North America Third largest continent on earth (24,256,000 Sq. Km) Composed of 23 countries Most North Americans speak French, Spanish, and English Only continent that has every kind of climate http://www.freeusandworldmaps.com/html/WorldRegions/WorldRegions.html Asia Largest continent in size and population (44,579,000 Sq. Km) Contains 47 countries Contains the world’s largest country, Russia, and the most populous country, China The Great Wall of China is the only man made structure that can be seen from space Home to Mt. Everest (on the border of Tibet and Nepal), the highest point on earth Mt. Everest is 29,028 ft. (8,848 m) tall http://craigwsmall.wordpress.com/2008/11/10/asia/ Europe Second smallest continent in the world (9,938,000 Sq. Km) Home to the smallest country (Vatican City State) There are no deserts in Europe Contains mineral resources: coal, petroleum, natural gas, copper, lead, and tin http://www.knowledgerush.com/wiki_image/b/bf/Europe-large.png Oceania/Australia Smallest continent on earth (7,687,000 Sq. -

Geography Notes.Pdf
THE GLOBE What is a globe? a small model of the Earth Parts of a globe: equator - the line on the globe halfway between the North Pole and the South Pole poles - the northern-most and southern-most points on the Earth 1. North Pole 2. South Pole hemispheres - half of the earth, divided by the equator (North & South) and the prime meridian (East and West) 1. Northern Hemisphere 2. Southern Hemisphere 3. Eastern Hemisphere 4. Western Hemisphere continents - the largest land areas on Earth 1. North America 2. South America 3. Europe 4. Asia 5. Africa 6. Australia 7. Antarctica oceans - the largest water areas on Earth 1. Atlantic Ocean 2. Pacific Ocean 3. Indian Ocean 4. Arctic Ocean 5. Antarctic Ocean WORLD MAP ** NOTE: Our textbooks call the “Southern Ocean” the “Antarctic Ocean” ** North America The three major countries of North America are: 1. Canada 2. United States 3. Mexico Where Do We Live? We live in the Western & Northern Hemispheres. We live on the continent of North America. The other 2 large countries on this continent are Canada and Mexico. The name of our country is the United States. There are 50 states in it, but when it first became a country, there were only 13 states. The name of our state is New York. Its capital city is Albany. GEOGRAPHY STUDY GUIDE You will need to know: VOCABULARY: equator globe hemisphere continent ocean compass WORLD MAP - be able to label 7 continents and 5 oceans 3 Large Countries of North America 1. United States 2. Canada 3. -

The History and Development of the Saint Lucia Civil Code N
Document generated on 10/01/2021 11:30 p.m. Revue générale de droit THE HISTORY AND DEVELOPMENT OF THE SAINT LUCIA CIVIL CODE N. J. O. Liverpool Volume 14, Number 2, 1983 Article abstract The Civil Code of St. Lucia was copied almost verbatim from the Québec Civil URI: https://id.erudit.org/iderudit/1059340ar Code and promulgated in the island in 1879, with minor influences from the DOI: https://doi.org/10.7202/1059340ar Civil Code of Louisiana. It has constantly marvelled both West Indians and visitors to the region alike, See table of contents that of all the former British Caribbean territories which were subjected to the vicissitudes of the armed struggles in the region between the Metropolitan powers resulting infrequent changes is sovereignty from one power to the Publisher(s) other, only St. Lucia, after seventy-six years of uninterrupted British rule since its last cession by the French, managed to introduce a Civil Code which in effect Éditions de l’Université d’Ottawa was in direct conflict in most respects with the laws obtaining in its parent country. ISSN This is an attempt to examine the forces which were constantly at work in 0035-3086 (print) order to achieve this end, and the resoluteness of their efforts. 2292-2512 (digital) Explore this journal Cite this article Liverpool, N. J. O. (1983). THE HISTORY AND DEVELOPMENT OF THE SAINT LUCIA CIVIL CODE. Revue générale de droit, 14(2), 373–407. https://doi.org/10.7202/1059340ar Droits d'auteur © Faculté de droit, Section de droit civil, Université d'Ottawa, This document is protected by copyright law. -

PWFI in the Caribbean
Cara_V.0.22_impresión.pdf 1 22/1/2020 15:44:35 Were you aware that... Every year, ten island states in the Caribbean generate more plastic debris than the weight of 20,000 space shuttles. These are Aruba, Antigua & Barbuda, Saint Kitts and Nevis, Guyana, Barbados, Saint Lucia, Bahamas, Grenada, Anguilla and Trinidad and Tobago. (Ewing-Chow,D. 2019) Plastic Waste-Free Islands © IUCN / Dave Elliot PWFI Caribbean countries of intervention Saving our oceans from plastic pollution Pillars of PWFI Knowledge IUCN works with countries to co-generate credible data and analysis to understand their current plastic leakage status, set targets, implement actions, and track progress towards targets over time. C M Y Capacity CM MY IUCN is facilitating collaboration amongst key public and private stakeholders to share best practices to CY enhance plastic waste management measures. CMY K Policy IUCN is supporting policy and legislative analysis For more information contact us at: and reform, to minimise plastic leakage. IUCN is working on identifying plastic leakage reduction IUCN, International Union for Conservation of Nature options and potential solutions through development Regional Office for Mexico, Central America and the Caribbean of scenario models. Tel: (506) 2283-8449 www.iucn.org/ormacc Email: [email protected] © IUCN / Derek Galon Sources: Boucher, J. and Friot D. (2017). Primary Microplastics in the Oceans: A Global INTERNATIONAL UNION FOR CONSERVATION OF NATURE Business Evaluation of Sources. Gland, Switzerland: IUCN. 43pp. Ewing-Chow,D. (2019). “Caribbean Islands Are The Biggest Plastic Polluters Per IUCN is working with the private sector, with a focus Capita In The World”. -

ICS South Africa
Integrated Country Strategy South Africa FOR PUBLIC RELEASE FOR PUBLIC RELEASE Table of Contents 1. Chief of Mission Priorities ................................................................................................................ 2 2. Mission Strategic Framework .......................................................................................................... 4 3. Mission Goals and Objectives .......................................................................................................... 6 4. Management Objectives ................................................................................................................ 12 FOR PUBLIC RELEASE Approved: August 22, 2018 1 FOR PUBLIC RELEASE 1. Chief of Mission Priorities There are tremendous opportunities to broaden U.S. engagement in South Africa which stand to benefit both countries. Over 600 U.S. companies already operate in South Africa, some for over 100 years; furthermore, many of them use South Africa as a platform for operations and a springboard for expansion into the rest of Africa. South Africa is therefore the single most critical market hub to a population expecting to double to two billion people in the next 30 years. While some resentment of the United States continues from the apartheid era, there is also recognition of American activism that helped end apartheid. In polls, the United States is seen very favorably by every day South Africans, who respond positively to American politics, culture, and goods. South Africa’s economy is the most -

Barbados' Debt Crisis: the Effects of Colonialism and Neoliberalism
University at Albany, State University of New York Scholars Archive Latin American, Caribbean, and U.S. Latino Latin American, Caribbean, and U.S. Latino Studies Honors Program Studies 2019 Barbados’ Debt Crisis: The Effects of Colonialism and Neoliberalism Noel Chase University at Albany, State University of New York, [email protected] Follow this and additional works at: https://scholarsarchive.library.albany.edu/lacs_honors Part of the Latin American Languages and Societies Commons Recommended Citation Chase, Noel, "Barbados’ Debt Crisis: The Effects of Colonialism and Neoliberalism" (2019). Latin American, Caribbean, and U.S. Latino Studies Honors Program. 4. https://scholarsarchive.library.albany.edu/lacs_honors/4 This Honors Thesis is brought to you for free and open access by the Latin American, Caribbean, and U.S. Latino Studies at Scholars Archive. It has been accepted for inclusion in Latin American, Caribbean, and U.S. Latino Studies Honors Program by an authorized administrator of Scholars Archive. For more information, please contact [email protected]. Barbados’ Debt Crisis: The Effects of Colonialism and Neoliberalism Faculty Sponsor Address: [email protected] | University at Albany Social Science 250 1400 Washington Avenue Albany, NY 12222 Undergraduate Author Address: [email protected] | 159 E 88th St Brooklyn, NY 11236 1 This research project explains the correlation between the tourism sector and Barbados’s cycle of debt. Barbados has continuously incurred debt, from international financing institutions such as the International Monetary Fund, since its independence from Great Britain in 1966. As of 2017, the estimated national debt of Barbados is $7.92 billion (USD).1 Sir Hillary Beckles, Michael Howard, and other economic experts and professors at the University of the West Indies, believe the country has gone into debt for a variety of different reasons. -

Republic of Seychelles
REPUBLIC OF SEYCHELLES MINAMATA INITIAL ASSESSMENT REPORT 2016 Document title Minamata Initial Assessment Report 2016 Document short title MIA Report Date 15th Mar 2017 Consultants AAI Enterprise Pty Ltd Lead Consultant, Mr Cliff Gonzalves, and Inventory Team, Ms Janet Dewea, Mrs Shirley Mondon and Ms Elaine Mondon First draft contributions from Mr Dinesh Aggarwal. Second draft contributions from Dr David Evers, Dr David Buck, and Ms Amy Sauer. Acknowledgements We would like to thank everyone who participated in the development of this document, including experts at the UNDP. Cover page photos by Mr. Cliff Gonzalves and the late Mr. Terrence Lafortune. Disclaimer This document does not necessarily represent the official views of the Government of Seychelles, the United Nations Development Programme, the Global Environment Facility, or the Secretariat of the Minamata Convention on Mercury. 2 Table of Contents ACRONYMS ............................................................................................................. 7 Foreword (draft) .................................................................................................... 9 Executive Summary ................................................................................................. 10 I. Results of the national mercury Inventory .............................................................................................. 10 II. Policy, regulatory and institutional assessment ................................................................................... -

Barbados High Commission
H.E. Mr. Guy Hewitt High Commissioner for Barbados to the United Kingdom of Great Britain and Northern Ireland Mr Tom Tugendhat, MP Chair Foreign Affairs Select Committee House of Commons London, SW1A 0AA 09 April 2018 Dear Chair, I write to request an opportunity for the victims, migration and human rights advocates, High Commissioners, and other concerned groups to have an interaction with members of the Foreign Affairs Select Committee on the situation facing some elderly Commonwealth-born residents in the UK. I write in part as a product of the Commonwealth as I was born in the UK to parents from India and Barbados. The situation is that these migrants from the Caribbean, and other Commonwealth countries, many of whom have been here since childhood, now, due to their irregular status, face the possibility of destitution, detention, and deportation. Based on information received from Migration Observatory at Oxford University we estimate there could be up to 50,000 Commonwealth-born persons in the UK who arrived before 1971 but do not have regularised status. The situation started with the call from Britain in the 1950s and 1960s to journey here to address labour shortages. Having left the Caribbean for the “Mother Country” as British Subjects, as the islands were still colonies, and having secured leave to remain and subsequently being educated, skilled, worked, taxed and levied in the UK, it never occurred to them that they were not legally British. The situation changed markedly in 2012, when the Home Office began systematic immigration checks. The real issue is that these long-term undocumented UK residents are not treated as anomalies to be regularised, but as “illegal immigrants” and barred from working and refused access to government services: the denial of NHS treatment, and loss of welfare benefits including housing benefits. -

ORGANISATION of EASTERN CARIBBEAN STATES Morne Fortuné, P.O
ORGANISATION OF EASTERN CARIBBEAN STATES Morne Fortuné, P.O. Box 179, Castries, St. Lucia. Telephone: (758) 452-2537 * Fax: (758) 453-1628 * E-mail: [email protected] COMMUNIQUE 42ND MEETING OF THE OECS AUTHORITY 6-8 November 2005 Malliouhana Hotel Meads Bay, Anguilla INTRODUCTION The 42nd Meeting of the Authority of the Organisation of Eastern Caribbean States (OECS) was held at the Malliouhana Resort, Anguilla, 6-8 November 2005. The Meeting was chaired by Prime Minister Dr. the Hon. Kenny Anthony of St. Lucia due to the unavoidable absence of the Chairman of the OECS Authority, Prime Minister Dr. Ralph Gonsalves of St. Vincent and the Grenadines. Heads of Government and Representatives of Heads of Government in attendance were: Hon. Baldwin Spencer, Prime Minister of Antigua and Barbuda. Hon John Osborne, Chief Minister of Montserrat. Hon. Dr. Denzil Douglas, Prime Minister of St. Kitts and Nevis. Dr. the Hon. Kenny Anthony, Prime Minister of St. Lucia. Hon. Osborne Fleming, Chief Minister of Anguilla. Hon. Gregory Bowen, Deputy Prime Minister and Minister of Agriculture, Lands, Fisheries and Energy Resources of Grenada. Hon. Charles Savarin, Minister of Foreign Affairs, Trade and the Civil Service of Dominica. Ms. Patricia Martin, Permanent Secretary, Ministry of Foreign Affairs, St. Vincent and the Grenadines Mr. Otto O’Neal, Director of Planning and Statistics, British Virgin Islands. Heads of delegations from regional institutions were: Sir Dwight Venner, Governor of the Eastern Caribbean Central Bank, ECCB. Mr. Alan Slusher, Director of Economics of the Caribbean Development Bank, CDB, and Mr. Rosemond James, Acting Director General of the Eastern Caribbean Civil Aviation Authority, ECCAA.