Polyvagal Theory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Implications of Polyvagal Theory in the Classroom
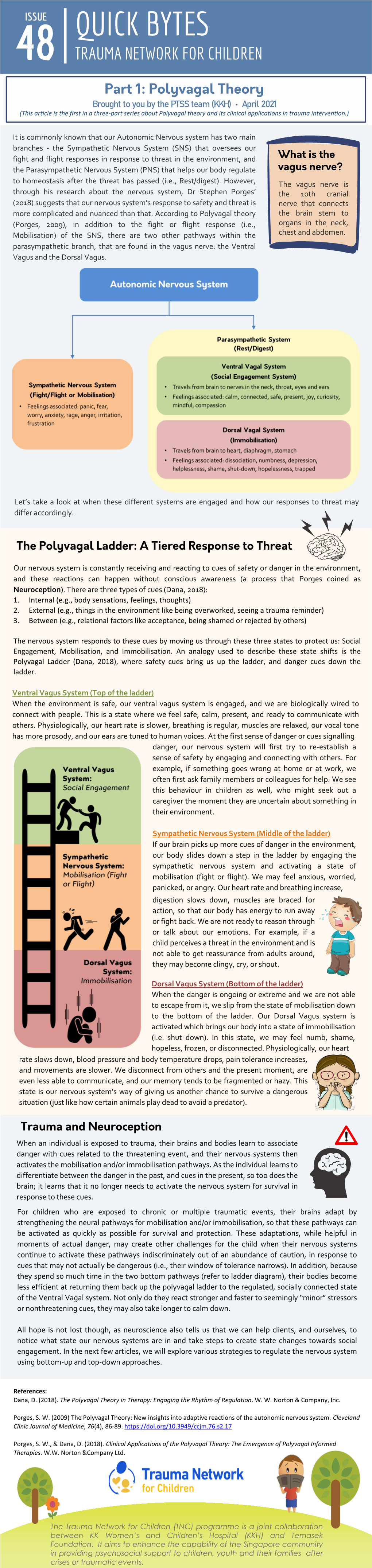
9/21/19 Social Connectedness as a Biological Imperative: Implications of Polyvagal Theory in the Classroom Stephen W. Porges, PhD Distinguished University Scientist, Kinsey Institute, Indiana University Professor Psychiatry, University of North Carolina Polyvagal Theory • A brain-body science of connection, trust, and safety • Leading to optimized mental and physical health and social behavior. • Can the principles of Polyvagal Theory be applied in the classroom? Copyright © 2019 Stephen W. Porges 1 9/21/19 Polyvagal Theory: Better Living Through Neurobiology • Helps identify environmental features that foster feelings of safety. • Explains how feeling safe “optimizes” behavior by turning off biobehavioral defenses, increasing spontaneous social behavior and opportunities to learn. • Explains the positive and negative feelings and behaviors of individuals while interacting (e.g., child and parent, partners, teacher and student, therapist and client). Copyright © 2019 Stephen W. Porges Better Education Through an Understanding of Neurobiology • How does neurobiology relate to education? – Improve learning – Optimize social behavior within the classroom • The traditional training does not prepare teachers for the problems they face in the classroom. – Teacher education focuses on learning and cognitive processes – The most relevant problems in the classroom are related to behavior and the underlying physiological state • How would educators embrace a classroom of students (independent of age) who were able to relate their behavioral state? 2 9/21/19 Visualize a Polyvagal-Informed Classroom • Are the prevalent models of education appropriate? – Education is steeped behavioral learning theory (S-R models). – Polyvagal Theory individualizes and dynamically expands the model from S-R to S-O-R. Where the ‘O’ is the physiological state of the student. -

Polyvagal Theory: Introduction for Somatic Psychotherapy Vincentia Schroeter
Polyvagal Theory: Introduction for Somatic Psychotherapy Vincentia Schroeter I. ABSTRACT This paper introduces polyvagal theory (1995) as defined by its originator, Stephen Porges, for the benefit of somatic, body-oriented, clinical psychotherapists. While there has been a recent explosion of interest in integrating this psychophysiological theory within various fields, some of the references to and explanation of the material can be difficult to grasp. The goal of this paper is to provide a clear explication of this theory. The main tenets of polyvagal theory will be presented including neuroception, the old and new view of the autonomic nervous system (ANS), normal and stress functions of the ANS, and trauma and attachment from a polyvagal point of view. Case material will illustrate somatic relational techniques from through an ANS lens. The use of anatomical portals to contact or promote shifts will be provided. KEYWORDS: polyvagal, neuroception, autonomic nervous system, sympathetic, social engagement system, vagal brake, portals. II. INTRODUCTION Interest in polyvagal theory has been spreading as it lends a valuable new view of human behavior from a neurological point of view. Within psychology, polyvagal theory has broad clinical applications and has influenced the understanding and treatment of many issues including trauma, personality disorders, and childhood challenges, such as autism. While many psychotherapists are integrating Polyvagal Theory into their clinical understanding and practice (including articles in this journal: see Heinrich-Clauer (2016), Shahri (2014, 2017), Clauer (2016), also Clauer workshop, IIBA conference (2011), the theoretical information can appear complex, particularly due to the dense writing of the book introducing polyvagal theory by it’s originator, Stephen Porges. -

The Polyvagal Theory: Phylogenetic Substrates of a Social Nervous System
International Journal of Psychophysiology 42Ž 2001. 123᎐146 The polyvagal theory: phylogenetic substrates of a social nervous system Stephen W. Porges Department of Psychiatry, Uni¨ersity of Illinois at Chicago, 1601 W. Taylor Street, Chicago, IL 60612-7327, USA Received 16 October 2000; received in revised form 15 January 2001; accepted 22 January 2001 Abstract The evolution of the autonomic nervous system provides an organizing principle to interpret the adaptive significance of physiological responses in promoting social behavior. According to the polyvagal theory, the well-documented phylogenetic shift in neural regulation of the autonomic nervous system passes through three global stages, each with an associated behavioral strategy. The first stage is characterized by a primitive unmyelinated visceral vagus that fosters digestion and responds to threat by depressing metabolic activity. Behaviorally, the first stage is associated with immobilization behaviors. The second stage is characterized by the sympathetic nervous system that is capable of increasing metabolic output and inhibiting the visceral vagus to foster mobilization behaviors necessary for ‘fight or flight’. The third stage, unique to mammals, is characterized by a myelinated vagus that can rapidly regulate cardiac output to foster engagement and disengagement with the environment. The mammalian vagus is neuroanatomically linked to the cranial nerves that regulate social engagement via facial expression and vocalization. As the autonomic nervous system changed through the process of evolution, so did the interplay between the autonomic nervous system and the other physiological systems that respond to stress, including the cortex, the hypothalamic᎐pituitary᎐adrenal axis, the neuropeptides of oxytocin and vasopressin, and the immune system. -

Polyvagal Theory, the Triune Autonomic Nervous System, And
Polyvagal Theory, the Triune Autonomic operational. Therefore structures evolved to secure dependent Nervous System, and Therapeutic Applications care for this extended time. Certain emotional affects, specifically the love feelings of mother/baby, are this survival By John Chitty, RPP, RCST mechanism. The “Social Nervous System” exists as a controller www.energyschool.com, email [email protected] over the sympathetic to enable moderation of more crude The “Polyvagal Theory” is a new understanding of the “fight/flight” responses to accommodate this dependency. autonomic nervous system (ANS), arising from the research The anatomy of the Social Nervous System consists of and writings of Stephen Porges, PhD. It uses solid scientific tools that bond a newborn to the mother. These include voice, method to significantly change the previous commonly- hearing, visual contact and facial expression, which are each accepted view of the ANS, with huge implications for trauma capable of triggering neurotransmitters inducing pleasurable therapies. sensations in the caregiver. These are “hard-wired,” The ANS is the neuro-endocrine-immune structure that precognitive functions that exist in newborns and have a enables survival. Traditionally it has been described as having compelling power to engender emotional bonding and two branches, parasympathetic (rest/rebuild) and sympathetic biochemical events which we interpret as love, thereby (fight/flight). Parasympathetic takes care of essential securing protective care during the vulnerable period. Healthy background operations such as heart/lungs and digestion, babies exhibit these instantly at delivery. They experience while sympathetic provides stress-response and procreation unsuccessful deployment of these strategies (i.e., betrayal by or strategies and functions. -

Love: an Emergent Property of the Mammalian Autonomic Nervous System
Psychoneuroendocrinology, Vol. 23, No. 8, pp. 837–861, 1998 © 1998 Elsevier Science Ltd. All rights reserved Printed in Great Britain 0306-4530/98 $ - see front matter PII: S0306-4530(98)00057-2 LOVE: AN EMERGENT PROPERTY OF THE MAMMALIAN AUTONOMIC NERVOUS SYSTEM Stephen W. Porges Institute for Child Study, University of Maryland, College Park, MD 20742-1131, USA SUMMARY The evolution of the autonomic nervous system provides an organizing principle to interpret the adaptive significance of mammalian affective processes including courting, sexual arousal, copula- tion, and the establishment of enduring social bonds. According to the Polyvagal Theory (Porges, 1995, 1996, 1997), the well-documented phylogenetic shift in the neural regulation of the autonomic nervous system passes through three stages, each with an associated behavioral strategy. The first stage is characterized by a primitive unmyelinated visceral vagus that fosters digestion and responds to threat by depressing metabolic activity. Behaviorally, the first stage is associated with immobiliza- tion behaviors. The second stage is characterized by the sympathetic nervous system that is capable of increasing metabolic output and inhibiting the visceral vagus to foster mobilization behaviors necessary for ‘fight or flight’. The third stage, unique to mammals, is characterized by a myelinated vagus that can rapidly regulate cardiac output to foster engagement and disengagement with the environment. The mammalian vagus is neuroanatomically linked to the cranial nerves that regulate social engagement via facial expression and vocalization. The Polyvagal Theory provides neurobio- logical explanations for two dimensions of intimacy: courting and the establishment of enduring pair-bonds. Courting is dependent upon the social engagement strategies associated with the mammalian vagus. -
Polyvagal Theory and How It Relates to Social Cues by Jodi Clarke, MA, LPC/MHSP Medically Reviewed by Steven Gans, MD Updated on August 05, 2019
Polyvagal Theory and How It Relates to Social Cues By Jodi Clarke, MA, LPC/MHSP Medically reviewed by Steven Gans, MD Updated on August 05, 2019 Have you ever been in a situation where you feel uncertain or in danger but not really sure why? You may look around and see that no one else seems to be bothered, but something still feels off to you? You may not realize it, but you are walking around in the world each day reading thousands of social cues in your environment. In our interacting with others, we pick up facial expressions, tones of voice, bodily movement, and more. We are constantly busy observing and interacting with the world and others as part of the human experience. As we have these interactions with others, our sense of self is being shaped. We learn about ourselves and about others, who we can trust, and who feels dangerous to us. Our bodies are processing this type of information constantly through these interactions with the world. The Body's Surveillance System Our nervous system is a complex structure that gathers information from all over our body and coordinates activity. There are two main parts of the nervous system: the central nervous system and the peripheral nervous system. Central Nervous System The central nervous system consists of two structures: Brain. This is the structure composed of billions of interconnected neurons or nerve cells contained in the skull and functions as the coordinating center for almost all of our body's functions. It is the seat of our intellect. -

PORGES and the POLYVAGAL THEORY Reflections on Clinical
A7 Autogenic Dynamics: Physiological, Psychological, and Research Matters PORGES AND THE POLYVAGAL THEORY Reflections on clinical and therapeutic significance This polyvagal theory deals with complexities of the Autonomic Nervous System that are not yet fully understood – and are in the process of being further researched. This paper gives a brief (and therefore simplified) introduction to some of the main concepts. The next webpage – A8 (“The Polyvagal Theory and a more sympathetic awareness of the ANS”) gives a further perspective . Contents page 1. Preamble 1 2. Perception and neuroception from the perspective of the Polyvagal theory 2 Co-option of un-myelinated vagus for other immobilisation activities not 3 associated with fear or threat: 3. The Polyvagal System 3 • Figure 1: Four overlapping systems embraced by the Polyvagal Theory 4 4. The central trio of the polyvagal theory – 5 Engagement, Mobilisation, and Immobilisation. 5. Affect, the Social Engagement System, and caring 6 6. Interactive play ( PLAY ) and Social Engagement 7 • Figure 2: Schematic and highly simplified bio-dance of neuro-circuits 8 involved in harmonious play 7. Summary 9 • 10 Including Figure 3: The Polyvagal Theory, Bodily States and Five Domains of Behaviour Appendix l 11 Some further aspects of the neuro-anatomy and physiology of the polyvagal theory including • 12 Figures 4 – 7 Appendix ll 13 Reflections on asthma in terms of the Vagal Competition Hypothesis 13 • 13-14 Including Figures 8 – 9B References and sources 15 Linked themes in this Autogenic Dynamics section 16 1. Preamble The polyvagal theory links the evolution of the neural regulation of the heart to affective experience, emotional expression, facial gestures, vocal communication, and social behaviour that is responsive to the behaviour of others. -

Ventral Vagus Healing & Craniosacral Therapy
Ventral Vagus Healing & Craniosacral Therapy 11/8/2018 Our Autonomic Nervous System (ANS), is the conductor of the inner orchestra in our body, responsible for the control of our bodily functions not consciously directed, such as breathing, the heartbeat, blood pressure, sweating and digestive processes. The ANS is always humming at a certain beat and how well it operates, determines our physical, mental and emotional health. In previous blogs I have written about the ANS. Our ANS was previously seen as having only 2 divisions: the Sympathetic Nervous System (SNS), fight or flight and the Parasympathetic Nervous System (PNS), relax and digest. Stephen Porges, Polyvagal Theory describes a new model of our nervous system. He describes how we respond to threats in 3 different biologically pre-programmed hierarchical ways. In this new model the PNS is divided into 2 branches, each with their own unique pathways and neural influences. Here, the PNS is divided into the Ventral Vagus Nerve (VNN) branch (also known as our Social Engagement System) and the Dorsal Vagus Nerve branch (DVN) which is characterised by immobilisation, freeze, shut down and withdrawal. This new model has great implications for the advancement of our health and well-being both practically and in therapy as each of these states, comes with their own set of physiological and emotional states, well- being and behaviours. (see also previous blog: Depression, Anxiety and Vagus Nerve). In this blog we will delve into the VVN, our Social Engagement System, the implications on our health and well-being and how craniosacral therapy can successfully help. -

Polyvagal Theory Informed Dance/Movement Therapy
Lesley University DigitalCommons@Lesley Graduate School of Arts and Social Sciences Expressive Therapies Capstone Theses (GSASS) Spring 5-16-2020 Rhythm and Safety of Social Engagement: Polyvagal Theory Informed Dance/Movement Therapy Suzanne Weare Lesley University, [email protected] Follow this and additional works at: https://digitalcommons.lesley.edu/expressive_theses Part of the Alternative and Complementary Medicine Commons, Cognition and Perception Commons, Counseling Psychology Commons, Dance Movement Therapy Commons, and the Other Mental and Social Health Commons Recommended Citation Weare, Suzanne, "Rhythm and Safety of Social Engagement: Polyvagal Theory Informed Dance/Movement Therapy" (2020). Expressive Therapies Capstone Theses. 347. https://digitalcommons.lesley.edu/expressive_theses/347 This Thesis is brought to you for free and open access by the Graduate School of Arts and Social Sciences (GSASS) at DigitalCommons@Lesley. It has been accepted for inclusion in Expressive Therapies Capstone Theses by an authorized administrator of DigitalCommons@Lesley. For more information, please contact [email protected], [email protected]. Running head: RHYTM AND SAFETY 1 Rhythm and Safety of Social Engagement: Polyvagal Theory Informed Dance/Movement Therapy Suzanne Weare Lesley University May 5, 2020 Suzanne Weare Dance/Movement Therapy Sarah Hamil, Ph.D., LCSW, RPT-S, ATR-BC RHYTM AND SAFETY 2 Abstract The polyvagal theory has exerted great influence on the field of clinical therapy since the 1990s by proposing an understanding -
The Polyvagal Theory's Use in Treating Trauma
The Polyvagal Theory for Treating Trauma A Teleseminar Session with Stephen W. Porges, PhD and Ruth Buczynski, PhD The National Institute for the Clinical Application nicabm of Behavioral Medicine www.nicabm.com The Polyvagal Theory for Treating Trauma 2 The Polyvagal Theory for Treating Trauma Contents What Practitioners Need to Know about Trauma and the Nervous System . 3 How the Polyvagal Theory Refines Our Understanding of Trauma . 5 Autonomic Nervous Systems . 8 Neuroception - Detection Without Awareness . 10 Triggering PTSD . 12 The Role of Social Engagement and Attachment . 13 What Do Autism and Trauma Have in Common? . 14 Treatment of Autism Disorders . 17 A Listening Project - Theory and Treatment . 21 A complete transcript of a Teleseminar Session featuring Stephen W. Porges, PhD and conducted by Dr. Ruth Buczynski, PhD of NICABM The National Institute for the Clinical Application of Behavioral Medicine www.nicabm.com The Polyvagal Theory for Treating Trauma 3 The Polyvagal Theory for Treating Trauma with Stephen W. Porges, PhD and Ruth Buczynski, PhD Dr. Buczynski: Hello everyone, I’d like to get started. Welcome back to this last teleseminar in our series on the treatment of trauma. I’m Dr. Ruth Buczynski a licensed psychologist in the state of Connecticut and the President of the National Institute for the Clinical Application of Behavioral Medicine. And I’m so glad that you’re joining us tonight for what will be a very, very exciting call. But before we begin, as has become our tradition at NICABM I’d like to share with you just some of the countries that were represented on last week’s call. -

Thank You the Polyvagal Theory Explains Everything!
3/10/2020 Creating Excellent Organizations through Brain and Body Science Patricia D. Wilcox, LCSW The Traumatic Stress Institute Klingberg Family Centers New Britain, Connecticut 2020 1 2 Thank you The concepts and therapy worksheets in this presentation have been learned from: Dana, Deb The Polyvagal Theory in Therapy: Engaging the Rhythm of Regulation (Norton Series on Interpersonal Neurobiology) W. W. Norton & Company; 1 edition (June, 2018) Which is based on the work of Steven Porgess More ideas and exercises available in the book. 3 The Polyvagal Theory Explains Everything! 1 3/10/2020 4 Explains everything? Describes our physical system of managing danger and intimacy The science of safety—the science of feeling safe enough to fall in love with life and take the risks of living. 5 What Is the Polyvagal Theory? POLY – many Creator Steven Porgess VAGAL – refers to the vagus nerve The Polyvagal Theory describes the multiple branches of the body’s vagus nerve and their role in maintaining our ability to stay safe and to thrive. 6 Key principles: • Not voluntary or conscious • No separation between our physical selves and our psychological selves • Applies equally to our clients and our selves 2 3/10/2020 7 The human paths to intimacy and safety The physical system that connects brain and body Three levels of reaction to Neuroception 8 Wait- what is neuroception? The way our autonomic nervous system scans for cues of safety, danger, and life-threat without involving the thinking parts of our brain. 9 Concept of Neuroception NEURO - -

A Neural Explanation of Fetal Heart Rate Patterns: a Test of the Polyvagal
DEV (WILEJ) LEFT INTERACTIVE Shawn F. Reed University of Maryland College Park, MD 20742 A Neural Explanation of Fetal Gonen Ohel Rahav David Heart Rate Patterns: A Test of Poriya Hospital Tiberias, Israel the Polyvagal Theory Stephen W. Porges University of Maryland College Park, MD 20742 Received 11 March 1998; accepted 5 February 1999 ABSTRACT: The current study applies a neurophysiological model based on the Polyvagal Theory (Porges, 1995) to interpret fetal heart rate patterns. Beat-to-beat heart rate data from 7 fetuses monitored during the ®rst and second stages of labor were analyzed. Transitory heart rate accelerations and reduced beat-to-beat variability reliably preceded heart rate decelera- tions. The data are interpreted within the context of the Polyvagal Theory, which provides a plausible explanation of the neurophysiological mechanisms that mediate fetal heart rate de- celerations. Speci®cally, it is proposed that both the transitory heart rate accelerations and the depression of the respiratory rhythm in the beat-to-beat heart rate pattern re¯ect a withdrawal of the vagal tone determined by myelinated vagal pathways originating in the nucleus ambig- uus. Functionally, withdrawal of vagal tone originating in the nucleus ambiguus results in the cardiac pacemaker becoming vulnerable to sympathetic in¯uences and to the more-primitive unmyelinated vagal pathways originating in the dorsal motor nucleus of the vagus, which may contribute to clinically relevant bradycardia. ᭧ 1999 John Wiley & Sons, Inc. Dev Psychobiol 35: 108±118, 1999 Keywords: electronic fetal heart rate monitoring; heart rate variability; respiratory sinus ar- rhythmia; vagus Based upon clinical observations and limited experi- mechanisms mediating the speci®c features of the mental manipulations, speci®c features of the fetal heart rate patterns used in the clinical assessment of heart rate pattern have been accepted by the clinical the fetus.