A Large UK Case Series of Retinal Injuries in Children Secondary to Hand-Held Lasers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Advanced Optics with Laser Pointer and Metersticks Roman Ya
Advanced Optics with Laser Pointer and Metersticks Roman Ya. Kezerashvili New York City College of Technology, The City University of New York 300 Jay Street, Brooklyn NY, 11201 Email: [email protected] Abstract We are using a laser pointer as a light source, and metersticks as an optical branch and the screen for wave optics experiments. It is shown the setup for measurements of wavelength of laser light and rating radial spacing of the CD, diffraction on a wire and a slit, observation of a polarization of light and observation of a hologram. 1. Introduction Laser pointers also know as laser penlights, have become very affordable recently due to new developments in laser technology. They are widely available at electronic stores, novelty shops, through mail order catalogs and by numerous other sources. They are in the price range from $1 to $30 as other electronic toys and are being treated as such by many parents and children. Pointers are used for other purposes such as the aligning of other lasers, laying pipes in construction, and as aiming devices for firearms. Laser pointer can be use to observe the interference, diffraction and polarization of light in college physics laboratory. Laser pointers can be used to produce holograms[1-2]. It been opinions it couldn't be done because of the short coherence of the beam and that laser pointer’s beam was not polarized. But it was practically proved that a laser pointer could be used not only to observe a hologram but to produce a high quality transmission and reflection display hologram[1-3]. -

Laser Pointer Safety About Laser Pointers Laser Pointers Are Completely Safe When Properly Used As a Visual Or Instructional Aid
Harvard University Radiation Safety Services Laser Pointer Safety About Laser Pointers Laser pointers are completely safe when properly used as a visual or instructional aid. However, they can cause serious eye damage when used improperly. There have been enough documented injuries from laser pointers to trigger a warning from the Food and Drug Administration (Alerts and Safety Notifications). Before deciding to use a laser pointer, presenters are reminded to consider alternate methods of calling attention to specific items. Most presentation software packages offer screen pointer options with the same features, but without the laser hazard. Selecting a Safe Laser Pointer 1) Choose low power lasers (Class 2) Whenever possible, select a Class 2 laser pointer because of the lower risk of eye damage. 2) Choose red-orange lasers (633 to 650 nm wavelength, choose closer to 635 nm) The National Institute of Standards and Technology (NIST) researchers found that some green laser pointers can emit harmful levels of infrared radiation. The green laser pointers create green light beam in a three step process. A standard laser diode first generates near infrared light with a wavelength of 808nm, and pumps it into a ND:YVO4 crystal that converts the 808 nm light into infrared with a wavelength of 1064 nm. The 1064 nm light passes into a frequency doubling crystal that emits green light at a wavelength of 532nm finally. In most units, a combination of coatings and filters keeps all the infrared energy confined. But the researchers found that really inexpensive green lasers can lack an infrared filter altogether. One tested unit was so flawed that it released nine times more infrared energy than green light. -
Modeling Light Interactions with Matter (Liquid Solutions)
Modeling Light Interactions with Matter (liquid solutions) Author(s): David Deutsch Date Created: July 31, 2015 (Revised June 22, 2017) Subject: Physics Grade Level: High School Standards: Next Generation Science Standards (www.nextgenscience.org) HS-PS4-5 Communicate technical information about how some technological devices use the principles of wave behavior and wave interactions with matter to transmit and capture information and energy Schedule: Two 45 minute periods CCMR Lending Library Connected Activities: Diffraction DNA and the Diffraction of Light (CIPT) The Phantastic Photon and LEDs (CIPT) Text is available under the Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0) license. - 1 – Objectives: Vocabulary: Laser pointers of several frequencies, · transmission index cards, and a small transparent · scattering container of extra virgin olive oil can be · absorption used to investigate the interaction of · fluorescence light with particles in solution. One can describe the observed phenomena · Stokes Shift operationally in terms of brightness, color, and direction or from a photon – particle perspective. Students Will: Materials: 1. Operationally define scattering, - Two plain white index cards transmission, absorption, and - One small, transparent container of fluorescence. extra virgin olive oil 2. Develop a photon/energy level - Laser pointers (green, red, blue/violet) model for absorption and fluorescence. 3. Interpret absorption and emission spectra and define the Stokes Shift The laser pointers used can damage Safety tissue, especially in the eye. Care must be taken to assure that laser light is aimed only at the targets intended in this activity Science Content for the Teacher: When light encounters matter (such as particles in a solution), there are several phenomena which may occur. -

Laser Pointer Safety
Laser Pointer Safety INTRODUCTION The use of laser diode pointers that operate in the visible radiation region (400 to 760 nanometers [nm]) is becoming widespread. These pointers are intended for use by educators while presenting talks in the classroom or at conventions and meetings. A high-tech alternative to the retractable, metal pointer, the laser pointer beam will produce a small dot of light on whatever object at which it is aimed. It can draw an audience¹s attention to a particular key point in a slide show. Laser pointers are not regulated at Oklahoma State University although the university has a Laser Safety Committee. Only Class IIIb and Class IV lasers are covered under OSU’s Laser Safety Program. The power emitted by these laser pointers ranges from 1 to 5 milliwatts (mW). Laser Pointers are similar to devices used for other purposes such as the aligning of other lasers, laying pipes in construction, and as aiming devices for firearms. They are widely available at electronic stores, novelty shops, through mail order catalogs and by numerous other sources. At $20 or even less, laser pointers are in the price range of other electronic toys and have been treated as such by many parents and children. Laser Pointers are not toys! Although most of these devices contain warning labels, as required by FDA regulations, many have been erroneously advertised as "safe". The potential for hazard with laser pointers is generally considered to be limited to the unprotected eyes of individuals who might be exposed by a direct beam (intrabeam viewing). -

High Performance Raman Spectroscopy with Simple Optical Components ͒ ͒ W
High performance Raman spectroscopy with simple optical components ͒ ͒ W. R. C. Somerville, E. C. Le Ru,a P. T. Northcote, and P. G. Etchegoinb The MacDiarmid Institute for Advanced Materials and Nanotechnology, School of Chemical and Physical Sciences, Victoria University of Wellington, P.O. Box 600, Wellington, New Zealand ͑Received 6 December 2009; accepted 19 April 2010͒ Several simple experimental setups for the observation of Raman scattering in liquids and gases are described. Typically these setups do not involve more than a small ͑portable͒ CCD-based spectrometer ͑without scanning͒, two lenses, and a portable laser. A few extensions include an inexpensive beam-splitter and a color filter. We avoid the use of notch filters in all of the setups. These systems represent some of the simplest but state-of-the-art Raman spectrometers for teaching/ demonstration purposes and produce high quality data in a variety of situations; some of them traditionally considered challenging ͑for example, the simultaneous detection of Stokes/anti-Stokes spectra or Raman scattering from gases͒. We show examples of data obtained with these setups and highlight their value for understanding Raman spectroscopy. We also provide an intuitive and nonmathematical introduction to Raman spectroscopy to motivate the experimental findings. © 2010 American Association of Physics Teachers. ͓DOI: 10.1119/1.3427413͔ I. INTRODUCTION and finish with a higher energy than the original one. This case corresponds to anti-Stokes Raman scattering. The Raman effect was discovered in 1928 by Raman1 and In reality, the photon is usually provided by a laser, which is now a major research tool with applications in physics, has a well defined frequency. -

CD, DVD, and Blu-Ray Disc Diffraction with a Laser Ray Box Alan J
CD, DVD, and Blu-Ray Disc Diffraction with a Laser Ray Box Alan J. DeWeerd, University of Redlands, Redlands, CA compact disc (CD) can be used as a diffraction grat- of the rays are blocked and the remaining ray is aimed at the ing, even though its track consists of a series of pits, point where the origin of the polar graph paper meets the CD. not a continuous groove. Previous authors described The paths of the incoming, reflected, and diffracted rays are Ahow to measure the track spacing on a CD using an incident visible, especially with the room lights slightly dimmed, so it is laser beam normal to the surface1 or one at an oblique angle.2 very easy to measure their directions. Note that the diffracted In both cases, the diffraction pattern was projected on a light on the paper will curve slightly as it gets further from the screen and distance measurements allowed the track spacing CD because it comes from higher up where the track becomes to be calculated. I propose an alternative method using a laser less vertical. Using the outer part of the CD where the track is ray box, which is also applied to a DVD and a Blu-ray disc. less curved reduces this effect. The upper portion of the CD Figure 1 shows the simple layout for the experiment. The could also be masked off to eliminate the problem. CD is taped to the edge of a table so that slightly more than In the simplest case, the incident ray is normal to the half of it sticks up over the edge, which means that the track surface of the CD, so the incident and reflected rays overlap. -

Blackbody Radiation and Optical Sources
01/03/2021 Blackbody Radiation and Optical Sources Optical Engineering Prof. Elias N. Glytsis School of Electrical & Computer Engineering National Technical University of Athens Prof. Elias N. Glytsis, School of ECE, NTUA 2 Wave-Particle Duality of Light De Broglie (1924): λ = h / p, h = 6.62607015 × 10-34 J sec, p = momentum (exact according to NIST 2018-2019) Φορτίο Ηλεκτρονίου: e = 1.602176634 × 10-19 Coulombs (exact according to NIST 2018-2019) Photons (zero rest mass) Particles (non-zero rest mass) https://physics.nist.gov/cgi-bin/cuu/Category?view=pdf&All+values.x=71&All+values.y=12 Prof. Elias N. Glytsis, School of ECE, NTUA 3 Light Sources Incoherent Light Sources Incandescent Sources Blackbody Radiators Discharge Lamps Line (Spectral) Sources) High-Intensity Sources Fluorescent Lamps Light Emitting Diodes (LED) Coherent Light Sources LASERS (Light Amplification via Stimulated Emission of Radiation) Prof. Elias N. Glytsis, School of ECE, NTUA 4 Blackbody Radiation https://chem.libretexts.org/Bookshelves/Physical_and_Theoretical_Chemistry_Textbook_Maps/Map%3A_Physical_C hemistry_(McQuarrie_and_Simon)/01%3A_The_Dawn_of_the_Quantum_Theory/1.01%3A_Blackbody_Radiation_Can not_Be_Explained_Classically Prof. Elias N. Glytsis, School of ECE, NTUA 5 Blackbody Radiation Prof. Elias N. Glytsis, School of ECE, NTUA 6 Electromagnetic Cavity Modes TEmpq Modes From Maxwell’s equations Electromagnetic Knowledge z a d TMmpq Modes y b x Dispersion Relation Prof. Elias N. Glytsis, School of ECE, NTUA 7 Blackbody Radiation 2ν q nd z c a R(ν) 1 1 2ν nb 1 c d p y 2ν b na x c m Density of Electromagnetic Modes per Frequency: Prof. Elias N. Glytsis, School of ECE, NTUA 8 Blackbody Radiation From Boltzmann’s statistics (energy of an em mode between E and E+dE): Normalization Average Energy per Electromagnetic Mode: Rayleigh-Jeans Equation Prof. -

Bright 1080P Laser Projector HZ39HDR
Bright 1080p Laser Projector HZ39HDR Exceptional colors and image quality for home entertainment 4,000 ANSI lumens with 300,000:1 contrast ratio Flexible installations with 1.3x zoom 4K UHD and 1080p HDR (HDMI 2.0) input compatible Accurate color with sRGB & REC.709 color profile Powerful 10-watt speaker DuraCore maintenance-free laser light source up to 30,000 hours Quiet operation 1080p Full 3D Bring the cinematic experience home with the incredible 4,000 lumens, 1080p Optoma HZ39HDR laser home theater projector. A DuraCore Laser light source eliminates lamp and filter replacements for up to 30,000 hours of maintenance-free operation with stunning color and image quality throughout the life of the projector. The compact size and low weight make mounting a breeze while its quiet operation ensures the HZ39HDR is seen, not heard. Vertical keystone correction and a 1.3x optical zoom provide flexible installation options. Blu-ray 3D support brings the immersive 3D movie experience home when paired with optional DLP-Link 3D glasses. Robust inputs include HDMI 2.0 and VGA for connectivity to a wide range of devices. CONNECTIVITY (May require optional accessories) 3D Blu-ray/DVD Players Smart ® Computers Phones Tablets Camcorders Apple TV Chromecast™ OPTICAL/TECHNICAL SPECIFICATIONS Display Technology Texas Instruments™ 0.65” 1080p DMD Color Wheel 4 segment RGBY Native Resolution 1080p 1 2 3 4 5 6 Maximum Resolution HDMI 2.0: 4K UHD (3840 x 2160 @ 60Hz) 4K (4096 x 2160, 60Hz) HDMI 1.4: WUXGA (1920 x 1200) 9 Brightness 4,000 ANSI lumens 7 8 Contrast Ratio 300,000:1 (Extreme Black enabled) 1,800:1 full on/full off 10 11 Displayable Colors 1.07 billion Lamp Life* Up to 30,000 hrs (Eco), 20,000 hrs (Normal) Light Source Type* DuraCore Laser Projection Method Front, rear, ceiling mount, table top 1. -
Light and Optics -- Build a Laser Communicator. Send Your Voice Over a Laser Beam
Chapter 7: Light and Optics -- Build a laser communicator. Send your voice over a laser beam. Scitoys.com Kitchen Science Ingredients Science Blog Custom Laser Crizal® No-Glare Lenses Power Do you stare at a computer all day? Try Crizal no-glare Supply lenses Rugged COTS Laser Diode Power Supplies for Military Science Toys Magnetism Electromagnetism Electrochemistry Radio Thermodynamics Aerodynamics Light and optics Simple laser communicator Make your own 3D pictures Making permanent rainbows. A solar powered marshmallow roaster Make a spectroscope from a CD. The impossible kaleidoscope Make a solar hotdog cooker Exploring invisible light A high resolution spectrograph. Time-lapse photography. High speed photography. Stacking photos for high depth of field. Biology Mathematics Computers and Electronics http://sci-toys.com/scitoys/scitoys/light/light.html[12/11/2014 12:08:29 PM] Chapter 7: Light and Optics -- Build a laser communicator. Send your voice over a laser beam. A simple laser communicator. How would you like to talk over a laser beam? In about 15 minutes you can set up your own laser communication system, using cheap laser pen pointers and a few parts from Radio Shack. For the transmitter you will need: 1. A laser pen pointer. You can get one for $10 from our catalog. 2. A battery holder that holds the same number of batteries as the laser pointer (often 3 cells). The batteries can be any size, but they must be the same voltage as the laser batteries. You may need to get one that holds two cells, and another that holds one cell, and wire them together in series. -
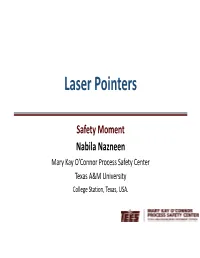
Laser Pointers
Laser Pointers Safety Moment Nabila Nazneen Mary Kay O’Connor Process Safety Center Texas A&M University College Station, Texas, USA. About me . Education: • Bachelor of Science, Chemical Engineering, Bangladesh University of Engineering and Technology (BUET) • MBA, Institute of Business Administration (IBA), University of Dhaka . Work Experience: • Supply Chain, Ericsson • Marketing and Supply Chain, DIRD Group 2 Red, Blue, Violet, Green . The human eye is most sensitive to light at a wavelength of 555 nanometers—a bright green. The green laser can produce brighter lights with less than 5mW output. Problem: Invisible infrared light 3 Class FDA Class IEC Laser Product Hazard Product Examples Considered non‐hazardous. Hazard increases if viewed ‐laser printers with optical aids, including magnifiers, binoculars, or I1, 1M ‐CD players telescopes. ‐DVD players Max output: <1 mW Hazard increases when viewed directly for long periods IIa, II 2, 2M of time. Hazard increases if viewed with optical aids. ‐bar code scanners Max output: 1 mW Depending on power and beam area, can be momentarily hazardous when directly viewed or when IIIa 3R staring directly at the beam with an unaided eye. Risk of ‐laser pointers injury increases when viewed with optical aids. Max output: 5 mW Immediate skin hazard from direct beam and immediate ‐laser light show projectors IIIb 3B eye hazard when viewed directly. ‐industrial lasers Max output: 500 mW research lasers Classification ‐laser light show projectors Immediate skin hazard and eye hazard from exposure to ‐industrial lasers either the direct or reflected beam; may also present a IV 4 ‐research lasers fire hazard. ‐lasers used to perform LASIK Max output: >500 mW eye surgery 4 Why Harmful? . -

WL-Manual 11232011.Pdf
Master Guide www.wickedlasers.com FOREWORD Absolute power. Unmatched performance. First and foremost, we are laser enthusiasts. We desire nothing more than Exceptional durability. to achieve perfection in our craft. For us, pushing the limits of technology is part of our daily routine. It’s only impossible if we don’t try. “Wicked” isn’t just our name, it is what we are. Those who seek us As we continue to advance in our search for perfection, we’ve set know what real lasers are about. benchmarks for others to follow and new limits for us to test. This is our What once was science fiction mission. We plan to continually push the boundaries of technology and is now reality. A technological create products that challenge the imagination far into the future. revolution has begun. Keep in mind, this is not a toy and this is definitely not a laser pointer. This is a Wicked Laser. WICKED LASERS Master Guide | 3 Table of Contents S3 Series 2 We wanted to create the world’s most powerful handheld laser - we E3 Series 4 succeeded and inadvertently set a world record in doing so. We are E2 Series 6 extremely proud to be included in the Guinness Book of World Records Core Series 8 for 2007. This will serve as a testament to our commitment to providing the FlashTorch 10 world with the most sophisticated laser products technology can offer. Laser Diagram (Core & E3 Series) 12 Laser Diagram (S3 Series) 14 Designed and developed by some of the world’s best engineers, the Spyder Using Your Laser 16 Series stands at the pinnacle of laser technology. -

2013:30 Laser Pointers and Eye Injuries an Analysis of Reported Cases
Author: Stefan Löfgren Jörgen Thaung Cesar Lopes Research 2013:30 Laser pointers and Eye injuries An analysis of reported cases Report number: 2013:30 ISSN: 2000-0456 Available at www.stralsakerhetsmyndigheten.se SSM perspective Background The safety limits that exist for human exposure of laser radiation are essential to reduce the risk of injuries. These values, however, give very little information on what tissue damages that may be expected at vari- ous elevated exposure levels. Similarly, the Swedish Radiation Protection Authority (SSM) has very little information on how such tissue damage is related to the impairment of the vision. This type of relationship bet- ween an imaginary exposure and a subsequent disability is very useful in the risk assessments that are made in the authority’s supervision acti- vities. Also, the damage’s evolvement over time is information that the authority can make use of in risk assessments. Objectives The purpose of this study was to investigate what dose of laser radia- tion, in terms of intensity and exposure time, may be associated with eye damages. The study has been limited to unwanted exposures of laser ra- diation from commercially available laser pointers. Of particular interest has been to search for data that clarify the dose-response relationships for functional disabilities that persist more than 6 months. Results The study shows that long-term vision loss can occur as a result of invo- luntary exposure from commercially available (strong) laser pointers at close range. The injury may occur before a normal person is able to re- spond by closing the eyelid, although there are only a few cases reported.